Myofascial Pelvic Pain
Original Editor - User Name
Top Contributors - Joseph Ayotunde Aderonmu, Khloud Shreif, David Olukayode, Kim Jackson and Leana Louw
Introduction[edit | edit source]
Myofascial Pelvic Pain (MPP) also called Myofascial Pelvic Pain Syndrome (MPPS) is a condition which affects the musculoskeletal system.[1] It is usually an unrecognized and untreated component of chronic pelvic pain (CPP) associated with high percentage of misdiagnosis, and high failure rate of medical interventions. Due to the above, it results in frustrated specialists and patients.[2]
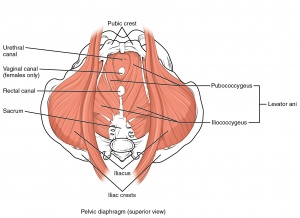
Myofascial pelvic pain refers to pain found in the pelvic floor musculature and connecting fascia. It is characterized by adverse symptoms of tender points, myofascial trigger points (MTrPs) in skeletal muscles.[3][4] It could exist alone with no concomitant medical pathology, exist as either a precursor or sequela to urological, gynecological, and colorectal medical conditions or other musculo-skeletal-neural issues. The hallmark diagnostic indicator of MFPP is myofascial trigger points in the pelvic floor musculature that refer pain to adjacent sites.[5][1]
Studies in the CPP literature have demonstrated existence of MTrPs or hypertonic pelvic floor muscles in medical conditions of different origins.[3][6][7] Yet, MPP is often overlooked by first-line health care providers as either a primary or contributing source of pain for conditions such as urgency/frequency, urge incontinence, constipation, dyspareunia, endometriosis, vulvodynia, coccygodynia, pudendal neuralgia, post-surgical or birthing pelvic pain, interstitial cystitis/painful bladder syndrome (IC/PBS). [8][3][9][6][7][10][11][12]
Sub Heading 2[edit | edit source]
Sub Heading 3[edit | edit source]
Resources[edit | edit source]
- bulleted list
- x
or
- numbered list
- x
References[edit | edit source]
- ↑ 1.0 1.1 Pastore EA and Katzman WB. Recognizing Myofascial Pelvic Pain in the Female Patient with Chronic Pelvic Pain. JOGNN, 41, 680-691; 2012.DOI: 10.1111/j.1552-6909.2012.01404.x
- ↑ Itza SF, Zarza D., Serra LL., Gómez SF., Salinas J., Bautrant E. (2014). Myofascial pain syndrome in the pelvic floor: etiology, mechanisms, symptoms, diagnosis, and treatment. DOI: 10.13140/RG.2.1.4482.7048
- ↑ 3.0 3.1 3.2 Bassaly, R., Tidwell, N., Bertolino, S., Hoyte, L., Downes, K., & Hart, S. (2010). Myofascial pain and pelvic floor dysfunction in patients with interstitial cystitis.International Urogynecology Journal, 22(4), 413–418. doi:10.1007/s00192-010-1301-3
- ↑ Doggweiler-Wiygul, R. (2004). Urologic myofascial pain syndromes. Current Pain and Headache Reports, 8(6), 445–451.
- ↑ Itza, F., Zarza, D., Serra, L., Gomez-Sancha, F., Salinas, J., & AllonaAlmagro, A. (2010). Myofascial pain syndrome in the pelvic floor: A common urological condition.Actas Urologicas Espanolas, 34(4), 318–326
- ↑ 6.0 6.1 Bendana, E. E., Belarmino, J. M., Dinh, J. H., Cook, C. L., Murray, B. P., & Feustel, P. J. (2009). Efficacy of transvaginal biofeedback and electrical stimulation in women with urinary urgency and frequency and associated pelvic floor muscle spasm. Urologic Nursing, 29(3), 171–176.
- ↑ 7.0 7.1 Chiarioni, G., Nardo, A., Vantini, I., Romito, A., & Whitehead, W. E. (2010). Biofeedback is superior to electrogalvanic stimulation and massage for treatment of levator ani syndrome. Gastroenterology,138(4), 1321–1329. doi:10.1053/j.gastro.2009.12.040
- ↑ Apte, G., Nelson, P., Brismee, J. M., Dedrick, G., Justiz, R., 3rd, & Sizer, P. S., Jr. (2011). Chronic female pelvic pain-part 1: Clinical pathoanatomy and examination of the pelvic region. Pain Practice: The Official Journal of World Institute of Pain, 12(2), 88–110. doi:10.1111/j.1533-2500.2011. 00465.x
- ↑ Butrick CW. Pelvic floor hypertonic disorders: Identification and management. Obstetrics and Gynecology Clinics of North America. 2009; 36(3):707–722.
- ↑ Doggweiler-Wiygul, R. (2004). Urologic myofascial pain syndromes. Current Pain and Headache Reports, 8(6), 445–451.
- ↑ Gentilcore-Saulnier, E., McLean, L., Goldfinger, C., Pukall, C. F., & Chamberlain, S. (2010). Pelvic floor muscle assessment outcomes in women with and without provoked vestibulodynia and the impact of a physical therapy program. Journal of Sexual Medicine, 7(2 Pt 2), 1003–1022. doi:10.1111/j.1743-6109.2009.01642.x
- ↑ Neville, C. E., Fitzgerald, C. M., Mallinson, T., Badillo, S. A., Hynes, C. K. (2010). Physical examination findings by physical therapists compared with physicians of musculoskeletal factors in women with chronic pelvic pain. Journal of Women’s Health Physical Therapy, 34(3), 73–80.