Otitis Media: Difference between revisions
Mohit Chand (talk | contribs) No edit summary |
Mohit Chand (talk | contribs) No edit summary |
||
| Line 38: | Line 38: | ||
== Pathophysiology == | == Pathophysiology == | ||
AOM is often, although not always, preceded by a viral upper respiratory tract infection that also affects the mucosa of the nose, nasopharynx, and Eustachian tubes.<ref>Winther B, Alper CM, Mandel EM, et al. Temporal relationships between colds, upper respiratory viruses detected by polymerase chain reaction, and otitis media in young children followed through a typical cold season. Pediatrics. 2007;119(6):1069–75. [https://pubmed.ncbi.nlm.nih.gov/17545372/]</ref> | |||
The middle ear has a narrow space, and the inflammation obstructs the narrowest part of the Eustachian tube, which leads to a decrease in ventilation. This causes negative pressure to increase in the middle ear and results in exudate from the inflamed mucosa. This leads to the growth of bacterial and viral organisms, which eventually causes suppuration and purulence in the middle ear | The middle ear has a narrow space, and the inflammation obstructs the narrowest part of the Eustachian tube, which leads to a decrease in ventilation. This causes negative pressure to increase in the middle ear and results in exudate from the inflamed mucosa. This leads to the growth of bacterial and viral organisms, which eventually causes suppuration and purulence in the middle ear. <ref>Fireman P. Otitis media and eustachian tube dysfunction: connection to allergic rhinitis. J Allergy Clin Immunol. 1997 Feb;99(2):S787-97.[https://pubmed.ncbi.nlm.nih.gov/9042072/] | ||
Fireman P. Eustachian tube obstruction and allergy: a role in otitis media with effusion? J Allergy Clin Immunol. 1985 Aug;76(2 Pt 1):137-40.[https://pubmed.ncbi.nlm.nih.gov/4019946/]</ref> | Fireman P. Eustachian tube obstruction and allergy: a role in otitis media with effusion? J Allergy Clin Immunol. 1985 Aug;76(2 Pt 1):137-40.[https://pubmed.ncbi.nlm.nih.gov/4019946/]</ref> | ||
== Histopathology == | == Histopathology == | ||
Acute purulent otitis media (APOM) is a condition in which the subepithelial space becomes swollen and red due to an infiltration of polymorphonuclear (PMN) leukocytes. As the inflammation progresses, the mucosal tissue undergoes changes and granulation tissue forms. After about five days, the epithelium changes from flat cuboidal to pseudostratified columnar, with the presence of goblet cells. | Acute purulent otitis media (APOM) is a condition in which the subepithelial space becomes swollen and red due to an infiltration of polymorphonuclear (PMN) leukocytes. As the inflammation progresses, the mucosal tissue undergoes changes, and granulation tissue forms. After about five days, the epithelium changes from flat cuboidal to pseudostratified columnar, with the presence of goblet cells. | ||
Serous acute otitis media (SAOM) occurs due to inflammation in the middle ear and eustachian tube, usually caused by venous or lymphatic stasis in the nasopharynx or eustachian tube. Inflammatory cytokines attract plasma cells, leukocytes, and macrophages to the site of inflammation, causing changes to the epithelium. This includes an increase in goblet cells due to hyperplasia of basal cells. | Serous acute otitis media (SAOM) occurs due to inflammation in the middle ear and eustachian tube, usually caused by venous or lymphatic stasis in the nasopharynx or eustachian tube. Inflammatory cytokines attract plasma cells, leukocytes, and macrophages to the site of inflammation, causing changes to the epithelium. This includes an increase in goblet cells due to hyperplasia of basal cells. | ||
| Line 57: | Line 57: | ||
* AOM is typically unilateral and causes ear pain (otalgia) and decreased or muffled hearing. The severity of the pain can range from mild to severe. | * AOM is typically unilateral and causes ear pain (otalgia) and decreased or muffled hearing. The severity of the pain can range from mild to severe. | ||
* If the tympanic membrane has ruptured, the patient will experience sudden relief of pain, possibly accompanied by purulent otorrhea. | * If the tympanic membrane has ruptured, the patient will experience sudden relief of pain, possibly accompanied by purulent otorrhea. | ||
* While dysequilibrium may also occur, it is not a common symptom. | * While dysequilibrium (balance and dizziness problems) may also occur, it is not a common symptom. | ||
* Conductive hearing loss, which is usually transient, can be caused by the presence of middle ear fluid. | * Conductive hearing loss, which is usually transient, can be caused by the presence of middle ear fluid. | ||
* If the patient experiences high fever, severe pain behind the ear, or facial paralysis, it could be a sign of unusual complications.[https://www.uptodate.com/contents/acute-otitis-media-in-adults#] | * If the patient experiences high fever, severe pain behind the ear, or facial paralysis, it could be a sign of unusual complications.[https://www.uptodate.com/contents/acute-otitis-media-in-adults#] | ||
Diagnostic accuracy is challenging because of the wide spectrum of signs and symptoms that develop throughout the course of the disease, the difficulties in examining the ears of young children who may be uncooperative or have occluding cerumen, and the overlap of symptoms (fever, otalgia, irritability, insomnia) with other entities such as viral illness.<ref>Kontiokari T, Koivunen P, Niemelä M, Pokka T, Uhari M. Symptoms of acute otitis media. Pediatr Infect Dis J. 1998;17:676–9. doi: 10.1097/00006454-199808000-00003. [https://pubmed.ncbi.nlm.nih.gov/9726339/]</ref> | |||
Signs and symptoms of ear infection in children may include: | Signs and symptoms of ear infection in children may include: | ||
| Line 90: | Line 90: | ||
Homme JH. Acute Otitis Media and Group A Streptococcal Pharyngitis: A Review for the General Pediatric Practitioner. Pediatr Ann. 2019 Sep 01;48(9):e343-e348.[https://pubmed.ncbi.nlm.nih.gov/31505007/]</ref> | Homme JH. Acute Otitis Media and Group A Streptococcal Pharyngitis: A Review for the General Pediatric Practitioner. Pediatr Ann. 2019 Sep 01;48(9):e343-e348.[https://pubmed.ncbi.nlm.nih.gov/31505007/]</ref> | ||
'''<u>Tympanocentesis:</u>''' | |||
'''Tympanocentesis''' is the drainage of fluid from the middle ear usually caused by otitis media, by using a small-gauge needle to puncture the tympanic membrane, also known as the eardrum. | |||
Tympanocentesis is reserved for extreme or refractory cases. It can improve diagnostic accuracy and guide treatment decisions after the middle ear fluid is removed and cultured to identify pathogens.<ref>Vayalumkal J, Kellner JD. Tympanocentesis for the management of acute otitis media in children: a survey of Canadian pediatricians and family physicians. Arch Pediatr Adolesc Med. 2004 Oct;158(10):962-5. [https://pubmed.ncbi.nlm.nih.gov/15466683/] | |||
Schaad UB. Predictive value of double tympanocentesis in acute otitis media. Pharmacotherapy. 2005 Dec;25(12 Pt 2):105S-10S.[https://pubmed.ncbi.nlm.nih.gov/16305279/]</ref> | |||
'''<u>Laboratory Studies:</u>''' | '''<u>Laboratory Studies:</u>''' | ||
| Line 103: | Line 111: | ||
# When a complication of otitis media is suspected, computed tomography of the temporal bones can help identify several potential issues such as mastoiditis, epidural abscess, sigmoid sinus thrombophlebitis, meningitis, brain abscess, subdural abscess, ossicular disease, and cholesteatoma. | # When a complication of otitis media is suspected, computed tomography of the temporal bones can help identify several potential issues such as mastoiditis, epidural abscess, sigmoid sinus thrombophlebitis, meningitis, brain abscess, subdural abscess, ossicular disease, and cholesteatoma. | ||
# Additionally, magnetic resonance imaging can be used to detect fluid collections, particularly in the middle ear. | # Additionally, magnetic resonance imaging can be used to detect fluid collections, particularly in the middle ear. | ||
'''<u>Other Tests:</u>''' | '''<u>Other Tests:</u>''' | ||
| Line 118: | Line 120: | ||
When acute otitis media is diagnosed, the primary goal of treatment is to relieve pain and address the underlying infection with antibiotics. | When acute otitis media is diagnosed, the primary goal of treatment is to relieve pain and address the underlying infection with antibiotics. | ||
To relieve pain, non-steroidal anti-inflammatory drugs (NSAIDs) or acetaminophen can be used. The use of antibiotics to treat otitis media early on is a controversial issue and varies based on the guidelines of the country. In Europe, a watchful waiting approach is practiced, but it is not widely accepted in the United States. However, if there is evidence of suppurative AOM, oral antibiotics should be given to treat the bacterial infection. High-dose amoxicillin or a second-generation cephalosporin are the preferred first-line agents for this purpose. | To relieve pain, non-steroidal anti-inflammatory drugs (NSAIDs) or acetaminophen can be used. The use of antibiotics to treat otitis media early on is a controversial issue and varies based on the guidelines of the country.<ref>Rettig, E., & Tunkel, D. E. (2014). Contemporary Concepts in Management of Acute Otitis Media in Children. ''Otolaryngologic Clinics of North America'', ''47''(5), 651. <nowiki>https://doi.org/10.1016/j.otc.2014.06.006</nowiki></ref> In Europe, a watchful waiting approach is practiced, but it is not widely accepted in the United States. However, if there is evidence of suppurative AOM, oral antibiotics should be given to treat the bacterial infection. High-dose amoxicillin or a second-generation cephalosporin are the preferred first-line agents for this purpose. | ||
If there is a perforation of the tympanic membrane, treatment should proceed with ototopical antibiotics that are safe for middle-ear use, such as ofloxacin. This method delivers much higher concentrations of antibiotics without any systemic side effects compared to systemic antibiotics.<ref>Chiappini E, Ciarcià M, Bortone B, Doria M, Becherucci P, Marseglia GL, Motisi MA, de Martino M, Galli L, Licari A, De Masi S, Lubrano R, Bettinelli M, Vicini C, Felisati G, Villani A, Marchisio P., Italian Panel for the Management of Acute Otitis Media in Children. Updated Guidelines for the Management of Acute Otitis Media in Children by the Italian Society of Pediatrics: Diagnosis. Pediatr Infect Dis J. 2019 Dec;38(12S Suppl):S3-S9.[https://pubmed.ncbi.nlm.nih.gov/31876600/]</ref> | If there is a perforation of the tympanic membrane, treatment should proceed with ototopical antibiotics that are safe for middle-ear use, such as ofloxacin. This method delivers much higher concentrations of antibiotics without any systemic side effects compared to systemic antibiotics.<ref>Chiappini E, Ciarcià M, Bortone B, Doria M, Becherucci P, Marseglia GL, Motisi MA, de Martino M, Galli L, Licari A, De Masi S, Lubrano R, Bettinelli M, Vicini C, Felisati G, Villani A, Marchisio P., Italian Panel for the Management of Acute Otitis Media in Children. Updated Guidelines for the Management of Acute Otitis Media in Children by the Italian Society of Pediatrics: Diagnosis. Pediatr Infect Dis J. 2019 Dec;38(12S Suppl):S3-S9.[https://pubmed.ncbi.nlm.nih.gov/31876600/]</ref> | ||
| Line 124: | Line 126: | ||
When a bacterial infection is suspected, the recommended antibiotic for both children and adults who are not allergic to penicillin is high-dose amoxicillin. The treatment should last for ten days. Amoxicillin is particularly effective in treating otitis media due to its high concentration in the middle ear. It is not recommended to use systemic steroids and antihistamines as they do not provide significant benefits. | When a bacterial infection is suspected, the recommended antibiotic for both children and adults who are not allergic to penicillin is high-dose amoxicillin. The treatment should last for ten days. Amoxicillin is particularly effective in treating otitis media due to its high concentration in the middle ear. It is not recommended to use systemic steroids and antihistamines as they do not provide significant benefits. | ||
Patients who have experienced four or more episodes of AOM in the past 12 months should be considered for '''myringotomy''' with tube (grommet) placement, according to the guidelines of the American Academy of Pediatrics. Recurrent infections that require antibiotics are clinical evidence of Eustachian tube dysfunction, and placement of the '''tympanostomy''' tube allows for ventilation of the middle ear space and maintenance of normal hearing. Moreover, if the patient develops otitis media while a functioning tube is in place, they can be treated with ototopical antibiotic drops instead of systemic antibiotics.<ref>Marchica CL, Dahl JP, Raol N. What's New with Tubes, Tonsils, and Adenoids? Otolaryngol Clin North Am. 2019 Oct;52(5):779-794. | Patients who have experienced four or more episodes of AOM in the past 12 months should be considered for '''myringotomy''' with tube (grommet) placement, according to the guidelines of the American Academy of Pediatrics. | ||
Recurrent infections that require antibiotics are clinical evidence of Eustachian tube dysfunction, and placement of the '''tympanostomy''' tube allows for ventilation of the middle ear space and maintenance of normal hearing. Moreover, if the patient develops otitis media while a functioning tube is in place, they can be treated with ototopical antibiotic drops instead of systemic antibiotics.<ref>Marchica CL, Dahl JP, Raol N. What's New with Tubes, Tonsils, and Adenoids? Otolaryngol Clin North Am. 2019 Oct;52(5):779-794. | |||
[https://pubmed.ncbi.nlm.nih.gov/31353143/]</ref> | [https://pubmed.ncbi.nlm.nih.gov/31353143/]</ref> | ||
| Line 158: | Line 162: | ||
== Resources == | == Resources == | ||
[https://publications.aap.org/pediatrics/article/131/3/e964/30912/The-Diagnosis-and-Management-of-Acute-Otitis-Media?autologincheck=redirected American Academy of Pediatrics] | |||
[https://archive.org/details/otitismediaininf0000blue/page/n3/mode/1up?view=theater Otitis Media in Infants and Children by Charles D. Bluestone, MD] | [https://archive.org/details/otitismediaininf0000blue/page/n3/mode/1up?view=theater Otitis Media in Infants and Children by Charles D. Bluestone, MD] | ||
== References == | == References == | ||
<references /> | <references /> | ||
Revision as of 08:27, 26 November 2023
Original Editor - Mohit Chand[edit | edit source]
Introduction[edit | edit source]
Otitis media refers to inflammation or infection of the middle ear, a common condition that can affect individuals of all ages, with a higher incidence in children.
It is a spectrum of diseases that includes:[1]
- Acute otitis media (AOM): A sudden onset of infection or inflammation in the middle ear.
- Chronic suppurative otitis media (CSOM): Persistent or recurrent inflammation or infection of the middle ear.
- Otitis media with effusion (OME): Fluid accumulation in the middle ear without active infection.
It is prevalent in all age groups, with a higher incidence in children, particularly between 6 to 24 months. This article explores the spectrum of otitis media, its etiology, epidemiology, pathophysiology, clinical features, diagnosis, and treatment modalities.[2]
Etiology[edit | edit source]
Otitis media is a complex condition that results from various factors such as infections, allergies, and environmental elements. The causes and risk factors include:
- Reduced immunity due to immuno-deficiencies like HIV, diabetes, and other similar conditions.
- Abnormalities in mucins gene expression, specifically upregulation of MUC5B
- Anatomic abnormalities of the palate and tensor veli palatini
- Ciliary dysfunction
- Genetic predisposition[3]
- Cochlear implants[4]
- Deficiency of Vitamin A
- Bacterial pathogens, including Streptococcus pneumoniae, Haemophilus influenza, and Moraxella (Branhamella) catarrhalis, are responsible for over 95% of cases.
- Viral pathogens such as respiratory syncytial virus, influenza virus, parainfluenza virus, rhinovirus, and adenovirus[5]
- Allergies
- Lack of breastfeeding[6]
- Exposure to passive smoke[7]
- Exposure to passive smoke
- Lower socioeconomic status
- Family history of frequent AOM in parents or siblings[8]
Epidemiology[edit | edit source]
Otitis media is a widespread issue that seems to affect males slightly more than females. However, due to varying reporting rates and differences in incidence across geographical regions, it's hard to pinpoint the exact number of cases that occur each year. Typically, otitis media is most common between the ages of six and twelve months and decreases after the age of five. [9]
Statistics show that approximately 80% of children will experience otitis media at least once in their lifetime, and between 80% and 90% of all children will experience otitis media with an effusion before starting school. While it's less common in adults than in children, certain sub-populations are still at risk, such as those with a history of recurrent OM in childhood, cleft palate, immunodeficiency, or immunocompromised status.[10]
Pathophysiology[edit | edit source]
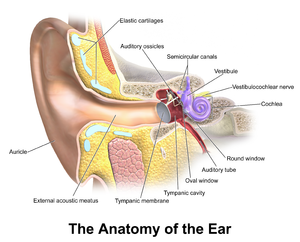
AOM is often, although not always, preceded by a viral upper respiratory tract infection that also affects the mucosa of the nose, nasopharynx, and Eustachian tubes.[11]
The middle ear has a narrow space, and the inflammation obstructs the narrowest part of the Eustachian tube, which leads to a decrease in ventilation. This causes negative pressure to increase in the middle ear and results in exudate from the inflamed mucosa. This leads to the growth of bacterial and viral organisms, which eventually causes suppuration and purulence in the middle ear. [12]
Histopathology[edit | edit source]
Acute purulent otitis media (APOM) is a condition in which the subepithelial space becomes swollen and red due to an infiltration of polymorphonuclear (PMN) leukocytes. As the inflammation progresses, the mucosal tissue undergoes changes, and granulation tissue forms. After about five days, the epithelium changes from flat cuboidal to pseudostratified columnar, with the presence of goblet cells.
Serous acute otitis media (SAOM) occurs due to inflammation in the middle ear and eustachian tube, usually caused by venous or lymphatic stasis in the nasopharynx or eustachian tube. Inflammatory cytokines attract plasma cells, leukocytes, and macrophages to the site of inflammation, causing changes to the epithelium. This includes an increase in goblet cells due to hyperplasia of basal cells.
Biopsy for histology is typically not carried out for OM outside of research environments.[13]
Clinical Features[edit | edit source]
Upper respiratory tract infections or seasonal allergic rhinitis often precede the onset of Acute Otitis Media (AOM) in adults.
- AOM is typically unilateral and causes ear pain (otalgia) and decreased or muffled hearing. The severity of the pain can range from mild to severe.
- If the tympanic membrane has ruptured, the patient will experience sudden relief of pain, possibly accompanied by purulent otorrhea.
- While dysequilibrium (balance and dizziness problems) may also occur, it is not a common symptom.
- Conductive hearing loss, which is usually transient, can be caused by the presence of middle ear fluid.
- If the patient experiences high fever, severe pain behind the ear, or facial paralysis, it could be a sign of unusual complications.[33]
Diagnostic accuracy is challenging because of the wide spectrum of signs and symptoms that develop throughout the course of the disease, the difficulties in examining the ears of young children who may be uncooperative or have occluding cerumen, and the overlap of symptoms (fever, otalgia, irritability, insomnia) with other entities such as viral illness.[14]
Signs and symptoms of ear infection in children may include:
- Irritability
- Headache
- Disturbed or restless sleep
- Poor feeding or anorexia
- Vomiting
- Diarrhea
- Pulling or tugging at the ears.
- About two-thirds of patients may also have a low-grade fever.
The diagnosis of otitis media mainly relies on clinical observations and accompanying signs and symptoms. Lab tests or imaging scans are not necessary.
The American Academy of Pediatrics has established guidelines for diagnosing acute otitis media, which involve the presence of moderate to severe bulging of the tympanic membrane or new onset of otorrhea (ear pain) not caused by otitis externa, or mild tympanic membrane bulging with recent onset of ear pain or erythema. These criteria are meant to assist primary care clinicians in making accurate diagnoses and informed clinical decisions, but not to replace their clinical judgment.[15]
The most effective and convenient way to diagnose ear problems is through an otoscopic examination. Acute otitis media (AOM) may cause reddish or normal tympanic membrane (TM) with fluid present in the middle ear, while suppurative otitis media shows obvious purulent fluid and a bulging TM.
If there is swelling in the external ear canal (EAC), significant swelling should be taken as a sign of otitis externa or AOE. AOE requires different treatment from other ear infections. It is essential to examine the TM to ensure it is not ruptured if there is swelling in the EAC. In the case of intact TM, painful and reddish EAC requires treatment with ototopical drops for AOE.
Both AOM and AOE may coexist, so it is important to examine the middle ear. Reactive EAC swelling can be assumed in case of TM perforation, and the use of ototopical medication is necessary. Only approved medications such as ofloxacin should be used as other agents can be ototoxic.[16]
Diagnosis[edit | edit source]
The diagnosis of otitis media should always begin with a physical examination using an otoscope, preferably a pneumatic one.[17]
Tympanocentesis:
Tympanocentesis is the drainage of fluid from the middle ear usually caused by otitis media, by using a small-gauge needle to puncture the tympanic membrane, also known as the eardrum.
Tympanocentesis is reserved for extreme or refractory cases. It can improve diagnostic accuracy and guide treatment decisions after the middle ear fluid is removed and cultured to identify pathogens.[18]
Laboratory Studies:
Laboratory tests are not usually required. However, if an infant below 12 weeks shows symptoms of fever with no apparent cause except acute otitis media, a thorough sepsis investigation may be necessary. There may be a need for laboratory tests to confirm or rule out any underlying systemic or congenital illnesses.
Imaging Studies:
Imaging studies should only be considered if there is a concern for intra-temporal or intracranial complications. Otherwise, they are not necessary.[19]
- When a complication of otitis media is suspected, computed tomography of the temporal bones can help identify several potential issues such as mastoiditis, epidural abscess, sigmoid sinus thrombophlebitis, meningitis, brain abscess, subdural abscess, ossicular disease, and cholesteatoma.
- Additionally, magnetic resonance imaging can be used to detect fluid collections, particularly in the middle ear.
Other Tests:
Middle ear effusion can also be evaluated using tympanometry and acoustic reflectometry.[20]
Treatment / Management[edit | edit source]
When acute otitis media is diagnosed, the primary goal of treatment is to relieve pain and address the underlying infection with antibiotics.
To relieve pain, non-steroidal anti-inflammatory drugs (NSAIDs) or acetaminophen can be used. The use of antibiotics to treat otitis media early on is a controversial issue and varies based on the guidelines of the country.[21] In Europe, a watchful waiting approach is practiced, but it is not widely accepted in the United States. However, if there is evidence of suppurative AOM, oral antibiotics should be given to treat the bacterial infection. High-dose amoxicillin or a second-generation cephalosporin are the preferred first-line agents for this purpose.
If there is a perforation of the tympanic membrane, treatment should proceed with ototopical antibiotics that are safe for middle-ear use, such as ofloxacin. This method delivers much higher concentrations of antibiotics without any systemic side effects compared to systemic antibiotics.[22]
When a bacterial infection is suspected, the recommended antibiotic for both children and adults who are not allergic to penicillin is high-dose amoxicillin. The treatment should last for ten days. Amoxicillin is particularly effective in treating otitis media due to its high concentration in the middle ear. It is not recommended to use systemic steroids and antihistamines as they do not provide significant benefits.
Patients who have experienced four or more episodes of AOM in the past 12 months should be considered for myringotomy with tube (grommet) placement, according to the guidelines of the American Academy of Pediatrics.
Recurrent infections that require antibiotics are clinical evidence of Eustachian tube dysfunction, and placement of the tympanostomy tube allows for ventilation of the middle ear space and maintenance of normal hearing. Moreover, if the patient develops otitis media while a functioning tube is in place, they can be treated with ototopical antibiotic drops instead of systemic antibiotics.[23]
Differential Diagnosis[edit | edit source]
The differential diagnosis of otitis media encompasses a range of conditions that could potentially cause ear pain.[24]
- Cholesteatoma
- Fever in the infant and toddler
- Fever without a focus
- Hearing impairment
- Pediatric nasal polyps
- Nasopharyngeal cancer
- Otitis externa
- Human parainfluenza viruses (HPIV) and other parainfluenza viruses
- Passive smoking and lung disease
- Pediatric allergic rhinitis
- Pediatric bacterial meningitis
- Pediatric gastroesophageal reflux
- Pediatric Haemophilus influenzae infection
- Pediatric HIV infection
- Pediatric mastoiditis
- Pediatric pneumococcal infections
- Primary ciliary dyskinesia
- Respiratory syncytial virus infection
- Rhinovirus (RV) infection (common cold)
- Teething
Resources[edit | edit source]
American Academy of Pediatrics
Otitis Media in Infants and Children by Charles D. Bluestone, MD
References[edit | edit source]
- ↑ Rettig E, Tunkel DE. Contemporary concepts in management of acute otitis media in children. Otolaryngol Clin North Am. 2014 Oct;47(5):651-72. [1]
- ↑ [2] Meherali S, Campbell A, Hartling L, Scott S. Understanding Parents' Experiences and Information Needs on Pediatric Acute Otitis Media: A Qualitative Study. J Patient Exp. 2019 Mar;6(1):53-61.
- ↑ Mittal R, Robalino G, Gerring R, Chan B, Yan D, Grati M, Liu XZ. Immunity genes and susceptibility to otitis media: a comprehensive review. J Genet Genomics. 2014 Nov 20;41(11):567-81.[3]
- ↑ Vila PM, Ghogomu NT, Odom-John AR, Hullar TE, Hirose K. Infectious complications of pediatric cochlear implants are highly influenced by otitis media. Int J Pediatr Otorhinolaryngol. 2017 Jun;97:76-82.[4]
- ↑ Seppälä E, Sillanpää S, Nurminen N, Huhtala H, Toppari J, Ilonen J, Veijola R, Knip M, Sipilä M, Laranne J, Oikarinen S, Hyöty H. Human enterovirus and rhinovirus infections are associated with otitis media in a prospective birth cohort study. J Clin Virol. 2016 Dec;85:1-6. [5]
- ↑ Ardiç C, Yavuz E. Effect of breastfeeding on common pediatric infections: a 5-year prospective cohort study. Arch Argent Pediatr. 2018 Apr 01;116(2):126-132.[6]
- ↑ Strachan DP, Cook DG. Health effects of passive smoking. 4. Parental smoking, middle ear disease and adenotonsillectomy in children. Thorax. 1998 Jan;53(1):50-6.[7] Jones LL, Hassanien A, Cook DG, Britton J, Leonardi-Bee J. Parental smoking and the risk of middle ear disease in children: a systematic review and meta-analysis. Arch Pediatr Adolesc Med. 2012 Jan;166(1):18-27. [8]
- ↑ Kraemer MJ, Richardson MA, Weiss NS, Furukawa CT, Shapiro GG, Pierson WE, Bierman CW. Risk factors for persistent middle-ear effusions. Otitis media, catarrh, cigarette smoke exposure, and atopy. JAMA. 1983 Feb 25;249(8):1022-5. [9]
- ↑ Usonis V, Jackowska T, Petraitiene S, Sapala A, Neculau A, Stryjewska I, Devadiga R, Tafalla M, Holl K. Incidence of acute otitis media in children below 6 years of age seen in medical practices in five East European countries. BMC Pediatr. 2016 Jul 26;16:108.[10]
- ↑ Schilder AG, Chonmaitree T, Cripps AW, Rosenfeld RM, Casselbrant ML, Haggard MP, Venekamp RP. Otitis media. Nat Rev Dis Primers. 2016 Sep 08;2(1):16063.[11]
- ↑ Winther B, Alper CM, Mandel EM, et al. Temporal relationships between colds, upper respiratory viruses detected by polymerase chain reaction, and otitis media in young children followed through a typical cold season. Pediatrics. 2007;119(6):1069–75. [12]
- ↑ Fireman P. Otitis media and eustachian tube dysfunction: connection to allergic rhinitis. J Allergy Clin Immunol. 1997 Feb;99(2):S787-97.[13] Fireman P. Eustachian tube obstruction and allergy: a role in otitis media with effusion? J Allergy Clin Immunol. 1985 Aug;76(2 Pt 1):137-40.[14]
- ↑ Meyerhoff WL, Giebink GS. Panel discussion: pathogenesis of otitis media. Pathology and microbiology of otitis media. Laryngoscope. 1982 Mar;92(3):273-7.[15]
- ↑ Kontiokari T, Koivunen P, Niemelä M, Pokka T, Uhari M. Symptoms of acute otitis media. Pediatr Infect Dis J. 1998;17:676–9. doi: 10.1097/00006454-199808000-00003. [16]
- ↑ Siddiq S, Grainger J. The diagnosis and management of acute otitis media: American Academy of Pediatrics Guidelines 2013. Arch Dis Child Educ Pract Ed. 2015 Aug;100(4):193-7.[17]
- ↑ Marchisio P, Galli L, Bortone B, Ciarcià M, Motisi MA, Novelli A, Pinto L, Bottero S, Pignataro L, Piacentini G, Mattina R, Cutrera R, Varicchio A, Luigi Marseglia G, Villani A, Chiappini E., Italian Panel for the Management of Acute Otitis Media in Children. Updated Guidelines for the Management of Acute Otitis Media in Children by the Italian Society of Pediatrics: Treatment. Pediatr Infect Dis J. 2019 Dec;38(12S Suppl):S10-S21.[18] Moazzami B, Mohayeji Nasrabadi MA, Abolhassani H, Olbrich P, Azizi G, Shirzadi R, Modaresi M, Sohani M, Delavari S, Shahkarami S, Yazdani R, Aghamohammadi A. Comprehensive assessment of respiratory complications in patients with common variable immunodeficiency. Ann Allergy Asthma Immunol. 2020 May;124(5):505-511.e3.[19] Kaur R, Czup K, Casey JR, Pichichero ME. Correlation of nasopharyngeal cultures prior to and at onset of acute otitis media with middle ear fluid cultures. BMC Infect Dis. 2014 Dec 05;14:640. [20]
- ↑ Chiappini E, Ciarcià M, Bortone B, Doria M, Becherucci P, Marseglia GL, Motisi MA, de Martino M, Galli L, Licari A, De Masi S, Lubrano R, Bettinelli M, Vicini C, Felisati G, Villani A, Marchisio P., Italian Panel for the Management of Acute Otitis Media in Children. Updated Guidelines for the Management of Acute Otitis Media in Children by the Italian Society of Pediatrics: Diagnosis. Pediatr Infect Dis J. 2019 Dec;38(12S Suppl):S3-S9.[21] Homme JH. Acute Otitis Media and Group A Streptococcal Pharyngitis: A Review for the General Pediatric Practitioner. Pediatr Ann. 2019 Sep 01;48(9):e343-e348.[22]
- ↑ Vayalumkal J, Kellner JD. Tympanocentesis for the management of acute otitis media in children: a survey of Canadian pediatricians and family physicians. Arch Pediatr Adolesc Med. 2004 Oct;158(10):962-5. [23] Schaad UB. Predictive value of double tympanocentesis in acute otitis media. Pharmacotherapy. 2005 Dec;25(12 Pt 2):105S-10S.[24]
- ↑ Penido Nde O, Borin A, Iha LC, Suguri VM, Onishi E, Fukuda Y, Cruz OL. Intracranial complications of otitis media: 15 years of experience in 33 patients. Otolaryngol Head Neck Surg. 2005 Jan;132(1):37-42.[25] Mattos JL, Colman KL, Casselbrant ML, Chi DH. Intratemporal and intracranial complications of acute otitis media in a pediatric population. Int J Pediatr Otorhinolaryngol. 2014 Dec;78(12):2161-4. [26]
- ↑ Lampe RM, Weir MR, Spier J, Rhodes MF. Acoustic reflectometry in the detection of middle ear effusion. Pediatrics. 1985 Jul;76(1):75-8.[27]
- ↑ Rettig, E., & Tunkel, D. E. (2014). Contemporary Concepts in Management of Acute Otitis Media in Children. Otolaryngologic Clinics of North America, 47(5), 651. https://doi.org/10.1016/j.otc.2014.06.006
- ↑ Chiappini E, Ciarcià M, Bortone B, Doria M, Becherucci P, Marseglia GL, Motisi MA, de Martino M, Galli L, Licari A, De Masi S, Lubrano R, Bettinelli M, Vicini C, Felisati G, Villani A, Marchisio P., Italian Panel for the Management of Acute Otitis Media in Children. Updated Guidelines for the Management of Acute Otitis Media in Children by the Italian Society of Pediatrics: Diagnosis. Pediatr Infect Dis J. 2019 Dec;38(12S Suppl):S3-S9.[28]
- ↑ Marchica CL, Dahl JP, Raol N. What's New with Tubes, Tonsils, and Adenoids? Otolaryngol Clin North Am. 2019 Oct;52(5):779-794. [29]
- ↑ Abdelaziz AA, Sadek AA, Talaat M. Differential Diagnosis of Post Auricular Swelling with Mastoid Bone Involvement. Indian J Otolaryngol Head Neck Surg. 2019 Nov;71(Suppl 2):1374-1376.[30] Suri NA, Meehan CW, Melwani A. A Healthy Toddler With Fever and Lethargy. Pediatrics. 2019 May;143(5)[31] Dorner RA, Ryan E, Carter JM, Fajardo M, Marsden L, Fricchione M, Higgins A. Gradenigo Syndrome and Cavitary Lung Lesions in a 5-Year-Old With Recurrent Otitis Media. J Pediatric Infect Dis Soc. 2017 Sep 01;6(3):305-308.[32]