Locked-In Syndrome: A Case Study: Difference between revisions
Saira Gill (talk | contribs) No edit summary |
No edit summary |
||
| Line 115: | Line 115: | ||
All three of these interventions can be beneficial to use for Mr. Gary to regain his functional status and help bring him closer to participating in activities he wishes to do so again. | All three of these interventions can be beneficial to use for Mr. Gary to regain his functional status and help bring him closer to participating in activities he wishes to do so again. | ||
==== Interdisciplinary Care ==== | |||
When discussing therapy for individuals with LIS, literature supports the value of an interdisciplinary team. Moreover, there is support for early (initiated within one month of onset) and aggressive intervention, which is associated with improved condition prognosis; namely, decreased mortality rate, more significant motor recovery, complete swallow recovery, verbal communication, communication through medical devices, and effective bowel and bladder control (Farr et al., 2021; Halan et al., 2021; Papadopoulou et al., 2019). The therapy team includes but is not limited to physiatrists, neurologists, neuropsychologist, physical therapist, cognitive therapist, speech therapist, occupational therapist, and nurse (Halan et al., 2021; Papadopoulou et al., 2019; Schnetzer et al., 2023). In the case of Gary, we as the physiotherapists would like to ensure his care is all encompassing, involving referrals to the respirologist, speech language pathologist (SLP) and occupational therapist (OT), among others. These specialists, all serving an integral role, are listed below based on priority (beginning with highest priority). While each play an important/key/invaluable role in the rehabilitation of an individual with LIS, the rankings were determined based on existing literature and consideration of whether the practitioner is ensuring survival or allowing for improvements in quality of life. | |||
For the purposes of this case, we will assume we are physiotherapists who are well acquainted to/well-educated in the realm of cardiorespiratory physiotherapy. If this was not the case, we would include/refer on to a physiotherapist who is confident and competent in this area of specialty. As mentioned in more detail in the intervention section, our role as a physiotherapist would include but not be limited to ensuring ROM and strengthening/ conditioning to prevent atrophy and further health complications which are associated with supine lying or immobility. More specific to our role as cardiorespiratory physiotherapists would be our facilitation of deep breathing exercises, postural drainage and positional changes (Papadopoulou et al., 2019). Acknowledging that these individuals may have restricted voluntary movements, as observed with Gary, positional changes will allow for prevention of contractures (Farr et al., 2021). Further, appreciating the amount of time spent primarily immobile, it is imperative that the OT is included for selection and fitting of an appropriate wheelchair (Farr et al., 2021). This will be discussed below. | |||
During the acute period of LIS, which has occurred secondary to an ischemic stroke of basilar artery, such as in our case, the neurologist would intervene with intraarterial thrombolysis (within 48 hours of the onset of symptoms) (Halan et al., 2021). The next step of acute care, in part provided by us as physiotherapists, is to ensure sufficient oxygenation (Halan et al., 2021). Our efforts would be accompanied with our highest priority referral, the respirologist. Through use of predictive measures such as heart rate and predictive markers, these professionals ensure not only proper airway functioning and adequate oxygen saturation levels, but also stability from a cardiac standpoint (Das et al., 2021). While patients with LIS showcase high prevalence of respiratory complications during hospitalization, a study by Svernling et al. (2019) found that no LIS patients under study, died as a result of respiratory complications. They attributed primarily to thorough care provided by the respirologists who prevent and treated respiratory problems in this population (Svernling et al., 2019). | |||
Our next referral is for Speech Language Pathology (SLP). In addition to respiratory function, swallowing and communication are imperative parts of everyday life. SLPs conduct assessments to evaluate swallowing via video fluoroscopy or fiberoptic endoscopic (Farr et al., 2021). Furthermore, they educate patients on assisted technologies, facilitating use of assisted technology such as infrared eye movement sensors and computer modulated voice tools (Das et al., 2021). Moreover, SLP involvement includes use of/application of VitalStim, a tool which addresses dysphagia through stimulating inactive swallowing muscles (Halan et al., 2019). This form of treatment improves both airway clearance as well as diet status, allowing for progression from NPO to small volumes of liquids and puree solids (Farr et al., 2021; Halan et al., 2019). Speech language therapy can also be accompanied by/supplemented with music therapy (Halan et al., 2019). This co-treatment allowed for improvements in outcomes such as voice output, initiation, and coordination (Halan et al., 2019.) | |||
Next, we believe it is important to refer to Occupational Therapy (OT). With this population, the OT team often works to implement and educate on available technologies, such as the universal ocular piloting system and Computer based augmentative and alternative communication systems (AAC) (Das et al., 2021; Farr et al., 2021; León-Carrión et al., 2002). These eye tracking techniques based on assessment of the patient’s eye shape and size as well as ocular behaviour (i.e.,gaze and movement), allow for improved communication (Das et al., 2021; Farr et al., 2021; León-Carrión et al., 2002). In addition to implementing up and coming communication techniques, the OT plays an important role in patient wheelchair use. The majority of LIS patients will require the long-term use of a wheelchair. For those who achieve only minimal recovery, a tilt-in-space wheelchair is the ideal choice for providing upright position, easy pressure relief, and transportation (Farr et al., 2021). The role of the OT would develop with progressions and developments in Gary’s abilities, allowing for strides in autonomous acts such as self-care and interacting with his environment. | |||
WILL PUT REFERRAL NOTE HERE | |||
==== Opportunities and Challenges of Utilizing Innovative Technology ==== | ==== Opportunities and Challenges of Utilizing Innovative Technology ==== | ||
Revision as of 18:43, 12 May 2023
Abstract[edit | edit source]
The following case study describes a patient with Locked-In Syndrome (LIS), a disorder of consciousness typically caused by an acquired brain injury. Patients present with tetraplegia and anarthria, despite unaffected/slightly affected cognition [1]. The patient in this case, Mr. Gary, sustained an occlusion to his basilar artery, leading to the diagnosis of LIS. The purpose of this case study is to outline expected clinical findings of a patient with LIS and recommended intervention strategies based on the current literature. Physiotherapists prove to have a vital role in the rehabilitation of patients with LIS. Prevention of common comorbidities such as pneumonia through breathing exercises and positioning is an area where physiotherapists play a key role. In addition, there are innovative evidence based interventions that can be individualized to the patient's presentation. Within the case of Mr. Gary, a treatment plan that focuses on motor control recovery through the use of tilt table training, treadmill therapy and repetitive sensorimotor training (RST) is emphasized to improve the patient's quality of life, ability to communicate, and regain some independence in mobility and activities of daily living. It is importantly noted that individuals with LIS benefit greatly from an interdisciplinary team consisting of respiratory therapists, speech language pathologists, occupational therapists, and many more.
Introduction[edit | edit source]
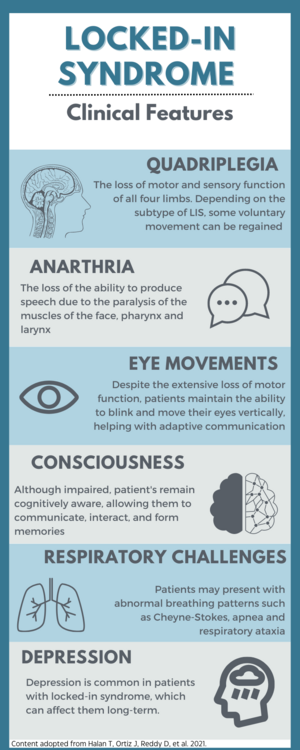
LIS is a disorder of consciousness that is caused by damage to the brainstem, specifically the ventral pons . Damage to this area can be caused by a stroke (hemorrhagic or ischemic) or trauma [1]. Patients with LIS will experience quadriplegia and the inability to speak, leaving them feeling “locked” inside their body [1]. Despite these significant motor losses, the function of their ocular muscles is preserved [1]. Paired with their intact cognitive awareness, patients are able to hear auditory stimuli, can communicate through blinking, and have the ability to move their eyes vertically [1]. LIS has three different subtypes, classic, partial, and complete, which categorize the patient’s presentation based on their motor and communication impairments. Classic LIS presents tetraplegia and anarthria. Patients with partial LIS have symptoms of classic as well as some voluntary movement other than vertical eye movement. Those with complete LIS have complete tetraplegia and are unable to move their eyes or blink, thus losing the ability to communicate.
Disruption to the corticospinal tracts and corticobulbar tracts are responsible for the quadriplegia and anarthria seen, respectively [1]. Patients with LIS will also experience changes to their respiratory function, demonstrating abnormal breathing patterns such as Cheyne-Stokes and apnea [1].
To verify that the patient has a ventral pons lesion their vestibular ocular reflex will remain intact. They will demonstrate a positive Babinski sign indicating corticospinal tract damage. In addition, they will exhibit intact pupillary light reflex, all confirming their locked-in syndrome is due to a ventral pons lesion [2].
Patient Characteristics[edit | edit source]
Mr. Gary is a 38-year-old male who lives with his wife and three kids in a three-story home backing onto Lake Ontario. Mr. Gary is a landlord of multiple apartment buildings at Queen’s University and a high school basketball coach. In his free time, he enjoys playing basketball with his old high school basketball teammates, who scrimmage every Saturday afternoon. 2 weeks ago, Mr. Gary came to the hospital with coordination deficits, dizziness, headache, and aphagia, and it was determined that he had a basilar artery occlusion impacting the brainstem, specifically the ventral region of the pons. Over the course of his hospital stay, he has progressively been showing signs of deterioration and decreased consciousness. At present, Mr. Gary has minimal body movements, only slight movements at his extremities. However, he still demonstrates pupillary responses, cognitive functioning and voluntary eye movements. Based on the current information and expert opinions, Mr. Gary was diagnosed with partial locked-in syndrome.
Examination Findings[edit | edit source]
When evaluating Mr. Gary, the following problem list was formed:
| Component of the ICF Model | Problem(s) |
|---|---|
| Body Structure and Function | Mr. Gary is unable to produce voluntary muscle movements of the trunk and extremities leading to difficulties executing physical activities done during a typical day (e.g. walking, stairs, bending over). |
| Activity Limitation | Loss of the ability to perform basic hygiene tasks such as brushing teeth, washing face. |
| Participation Restriction | Unable to take part in meaningful interactions such as driving his children to school and partaking in his work, limiting his ability to contribute to his family, which may lead to loss of purpose and depression. |
To target Mr. Gary's goals, we assigned an outcome measure to each portion of the ICF model to accurately and efficiently track his progress during the treatment intervention and ensure we reach his overall objectives.
To evaluate this problem list, the RAND 36-Item Health Survey can be used. The RAND-36 is an instrument that assesses health-related Quality of Life (HRQoL). This survey evaluates 8 various concepts such as physical functioning, role limitations due to physical health problems, bodily pain, and more. The RAND 36 survey has been shown to be both reliable and valid for evaluating HRQoL in individuals who have had a stroke and has been used extensively for persons with LIS. As such, to evaluate the problems identified under Mr. Gary’s body structure and functions, the RAND-36 is a valid, reliable and appropriate tool to assess his physical functioning and voluntary muscle movement[3].
An evidence-based outcome measure that will help establish and monitor Mr. Gary’s activity limitations and ability to be discharged from the hospital is the Functional Independence Measure (FIM). The FIM is an 18-item test which measures an individual’s level of disability. The test develops a motor score and cognitive score. The motor portion examines the patient’s ability to do activities such as showering, walking, using stairs, and the toilet, all correlating to his activity limitations indicated in the problem list [4]. This information determines whether we are improving upon Mr. Gary’s activity goals/impairments and when he will be ready for discharge from the hospital.
The Impact on Participation and Autonomy Questionnaire is an evidence-based outcome measure that will adequately analyze Mr. Gray's participation goals. This questionnaire is composed of 5 different domains: autonomy indoors, autonomy outdoors, social life and relationships, family role and education and work[3]. This questionnaire will give us a baseline on where he is regarding his participation goals of returning to work and hanging out with his family. Then, over time with our treatment interventions, we can utilize this questionnaire again to ensure we satisfy our patients' main concerns and objectives.
Common co-morbidities seen in LIS[edit | edit source]
It is well known that respiratory failure is a significant comorbidity among patients with Locked-in syndrome. Due to the reduced respiratory function, absent cough reflex, and the nature of being immobilized, there is an increased risk of secretion accumulation and aspiration (Newsome & Melton, 2023 [1]. As a result, the leading causes of death in patients with LIS is pneumonia and atelectasis [1]. Thus, it is vital to screen Mr. Gary for respiratory failure and assist with ventilation as required (e.g., breathing exercises, frequent position changes) [5]. Additionally, depression is a possible comorbidity seen in patients with LIS. Patients may feel depressed due to the prolonged stay in a hospital, the increased burden on family members, and the impression that their quality of life is significantly worse than it used to be [6]. As such, we must screen Mr. Gary for depressive symptoms so that referrals can be made to help treat them quickly and effectively.
Clinical Impression[edit | edit source]
Mr. Gary is a 38-year-old male presenting with partial LIS following an occlusion to the basilar artery. He has an overall loss of motor function, presenting as tetraplegia. He is cognitively intact and demonstrates his ability to communicate through blinking and vertical eye movement. Through observation, Mr. Gary has evidence of slight voluntary flexion and extension of his fingers and toes, however there are no other signs of body movement at this point. He displays signs of spasticity bilaterally in both arms, seen with a flexor movement synergy.
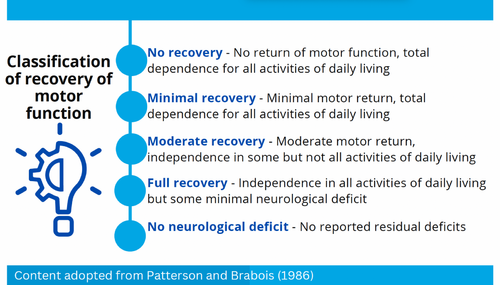
Prognostically, it is advantageous that the patient is young, and that rehabilitation can begin within the acute stage. Additionally, it is a good sign that Mr. Gary is already showing signs of motor movement, indicating the potential for recovery in his case. It will be essential to monitor for signs of respiratory failure, which is common in patients with LIS and can impact Mr. Gary’s prognostic timeline. As of now, Mr. Gary falls within the minimal recovery classification, and it is predicted that through rehabilitation, he will progress to moderate recovery as he gains more voluntary function of his distal extremities.
Intervention[edit | edit source]
Treatment Goals[edit | edit source]
Short Term Goal: To prepare Mr. Gary for wheelchair mobility, he will improve his upright posture tolerance as measured through increasing time tolerated on tilt table at larger angles of inclination in the next 3 weeks. Tolerance will be determined by light headedness, dizziness, and/or a decrease in blood pressure greater than 20 mmHg.
Long Term Goal: Mr. Gary will regain motor control of voluntary hand movements such as functional grasp, as measured through patient’s ability to grasp different objects of varying sizes, shapes and textures with accuracy and repetition within 2 months. Recovery of motor control can be applied to independent use of an electric wheelchair joystick and the ability to use electronic communication methods to improve activity limitations, patient quality of life and independence.
Treatment Plan[edit | edit source]
The treatment intervention for Mr. Gary will begin immediately, as early extensive physiotherapy is recommended for patients with LIS [7]. Immediate and aggressive therapy, 5-6 times per week, has been found to improve functional recovery and decrease the severity of LIS and mortality rate [7]. Rehabilitation interventions for LIS should focus on upright tolerance training followed by balance and mobility[8]. In addition, interventions should focus on distal motor control, as motor recovery tends to occur from distal to proximal [7]. The treatment program for Mr. Gary will begin with using a tilt table to improve upright postural tolerance. Tilt tables are a common therapeutic approach for patients with LIS [8]. Tilt table training has been shown to improve trunk stability, strengthen cervical muscles, and maintain flexibility of the ankles [8]. The treatment program will begin with gradually raising Mr. Gary to 60 degrees and having him sustain this inclination for a minimum of 5 minutes without signs of intolerance. The program will progress with 10 degree intervals from 60 to 90 degrees as tolerated by Mr. Gary. This protocol was supported by a study of a tilt table on improving functioning in patients in the acute stage following stroke [9]. Once Mr. Gary can sustain 90 degrees of inclination without symptoms of intolerance, the physiotherapy team will progress to treadmill therapy with body weight support.
Research has found that for patients with LIS, once they can tolerate an upright position, training on a treadmill with body weight support is essential for improving mobility [8]. Treadmill training with body weight support has been found to improve postural control, physical endurance, and mobility for patients with LIS [8]. The treatment program will involve the treadmill therapy with body weight support, where Mr. Gary will be secured by a harness and attached to a suspension system where two physiotherapists will assist him with walking movements. The treadmill will have handrails attached in front and on either side to promote grasping for Mr. Gary. The gait velocity will begin at 0.2 km per hour to achieve the walking movement and progress to 1-1.2 km per hour for a 15-20 minute session based on responses from Mr. Gary. Treadmill therapy has been found to be effective with 0.2-1.2 km per hour speeds for approximately 20-minute sessions for about 10 weeks for patients with partial LIS after stroke [10]. This protocol improved postural control, allowed patients to maintain a standing position over time, and improved overall physical functioning [10].
Furthermore, in order to address Mr. Gary’s long-term goal of regaining motor control of the upper extremities repetitive sensorimotor training will be used. Repetitive sensorimotor training (RST) encourages patients to repeatedly attempt to complete specific movements of the shoulder, elbow, wrist, and fingers respectively [11]. In instances where the patient is unable to complete the motion throughout the full range of motion, the therapist may assist the patient throughout the movement (Papadopoulou et al., 2019). As the patient begins to progress through larger ranges of motion, the therapist can progress the RST protocol by challenging the patient with gravity resisted movements or even the implementation of additional resistance [12]. With Mr. Gary, minimal voluntary movement was seen in both upper extremities therefore intensive RST will be completed with both upper extremities in order to regain as much functional motor control. In LIS patients recover distal extremity function prior to proximal therefore the initial RST sessions will involve movements specific to the fingers and wrist and over time progress to include elbow and shoulder movements [12]. A review conducted by Papadopoulou et al. was completed in order to determine the best clinical practice guidelines for patients with LIS [12]. Their research determined that RST was an effective treatment for patients with partial LIS to recover functional motor control of paretic upper extremities while also significantly shortening the expected rate of recovery [12]. An additional study demonstrated significant increase in patients upper extremity function through RST as seen through increased ability to complete ADL’s such as shaving and teeth brushing without the use an additional aid [11].
Specific RST protocol for Mr. Gary will begin with 60 minute sessions 5-6 times per week. The therapist will encourage Mr. Gary to complete large movements of the fingers and wrist into flexion and extension repeatedly in a gravity eliminated plane of motion. Mr. Gary will complete as much of the movements as possible autonomously, if needed the therapist will complete the movement throughout the full range of motion. Over time as motor control begins to improve the therapist will position Mr. Gary so that the joints will be moving through a gravity resisted plane of motion, increasing the difficulty of the motion for the patient. Additional progressions will begin to include movements of the elbow and shoulder joints as well as beginning to repeat functional motions such as reaching and grasping techniques.
The goal of RST therapy with Mr. Gary is to improve motor control of his upper extremities so that he may be able to complete functional activities such as operating an electric wheelchair for mobility, brushing his teeth, combing his hair, shaving, assisting with dressing etc. In the long term, technologies such as the Bioness H2000 can help to enhance mobility and daily function with Mr. Gary.
| Intervention | Parameters | Progression |
|---|---|---|
| Tilt Table | x 5-6/week
inclination from 0 degrees increasing 10 degrees every 5 minutes (symptom permitting). |
Over multiple sessions patient to be able to tolerate 90 degrees of inclination for 5+ minutes. |
| Treadmill Therapy with Body Weight Support | x 5-6/week
initial gait speed = 0.2 km/hour assist x2 of therapist moving lower limbs in proper gait pattern (symptom permitting). Walking time per session = 10 minutes |
Over multiple session therapists will increase gait speed up to 1.2 km/hour (increasing at 0.2 km/hour increments between sessions). Total talking time will increase to 20 minutes per session (increasing at 2–5-minute increments) |
| Repetitive Sensorimotor Training (RST) | x5-6/week
Large movements of the fingers and wrist into flexion and extension repeatedly in a gravity eliminated plane of motion Treatment time = 60 minutes |
Over multiple sessions the patient will begin to move more proximal upper extremity joints such as elbow and shoulders. Movements will become larger, move into gravity resisted plane and eventually movements with the addition of external resistance to motion. Functional movements such as reaching and grasping should be included as patient ability increases. |
Outcome[edit | edit source]
Adverse Events[edit | edit source]
Potential adverse events that can occur with patients who have LIS may include low blood pressure, dizziness, and lightheadedness. If a patient reports any of these symptoms during therapy, for example when using the tilt table intervention, the physiotherapy team could alter the parameters to decrease intensity for the patient. Specifically, if the patient is not tolerating the 10-degree increments to upright positioning, the physiotherapy team could use 5-degree increments. Additionally, the team could increase time spent at each increment to allow the patient’s body to better adapt before moving to the next increment.
If they experience these symptoms during the treadmill training, the physiotherapist can decrease the frequency or length of treadmill sessions to prevent adverse effects from occurring. During treadmill therapy the patient must be in upright standing position therefore it is possible that the initial transfer from sit to stand will provoke patient symptoms; the physiotherapist can eliminate this risk by slowly transferring the patient from sit to standing position to allow the patients body to adapt to the new position.
Furthermore, it is possible that fatigue may be induced in this population, due to the high intensity and frequency of treatment protocols. To reduce the risk of excessive fatigue, the physiotherapy team can decrease intensity and frequency of the intervention as necessary and ensure that frequent monitoring of perceived rates of exertion are noted using a pre-determined communication method with the patient. Physiotherapists must implement principles of pacing, prioritizing and planning to maximize therapy sessions for optimal patient outcomes.
Innovative Technology to Enhance Treatment Interventions[edit | edit source]
Utilizing innovative technology-mediated tools can enhance the treatment approach for individuals with LIS and help restore some of their lost motor function.
The Armeo Spring Program is a limb robotic utilized for upper extremity training. This machine connects to a virtual reality system with varying degrees of difficulty [13]. The patient puts their arm into an exoskeleton which supports them proximally to distally. They will then proceed to complete functional tasks based on what the virtual reality is [13]. This program has demonstrated efficacy in increasing accuracy and time of movement initiation in individuals with LIS. Completing repetitive movements with constant visual feedback enables the patient improvements in self-monitoring, sensory feedback and upper limb motor function control [1]. The program allows patients to use any remaining motor functions they have and continue to work and progress on reaching and grasping movements in a stimulating and functional environment [14].
Another innovative technology-mediated tool beneficial in individuals with LIS is Bioness H200. Bioness H200 is an extremity neuroprosthesis used for functional recovery of grasp in the upper extremities. The benefits of using this machine are that it can facilitate functional arm use, reduces spasticity, improves grip strength and allows for an active range of motion in the upper limb [15].
Lastly, treadmill therapy with body weight support is another innovative tool utilized with this population. This therapy can increase their motor function and postural control. With treadmill therapy, it can start with more passive movements and, throughout their recovery, transition to more independent body support [1]. Overall, treadmill therapy with body weight support allows individuals with locked-in syndrome the ability to be upright and walk when otherwise would be impossible [10].
All three of these interventions can be beneficial to use for Mr. Gary to regain his functional status and help bring him closer to participating in activities he wishes to do so again.
Interdisciplinary Care[edit | edit source]
When discussing therapy for individuals with LIS, literature supports the value of an interdisciplinary team. Moreover, there is support for early (initiated within one month of onset) and aggressive intervention, which is associated with improved condition prognosis; namely, decreased mortality rate, more significant motor recovery, complete swallow recovery, verbal communication, communication through medical devices, and effective bowel and bladder control (Farr et al., 2021; Halan et al., 2021; Papadopoulou et al., 2019). The therapy team includes but is not limited to physiatrists, neurologists, neuropsychologist, physical therapist, cognitive therapist, speech therapist, occupational therapist, and nurse (Halan et al., 2021; Papadopoulou et al., 2019; Schnetzer et al., 2023). In the case of Gary, we as the physiotherapists would like to ensure his care is all encompassing, involving referrals to the respirologist, speech language pathologist (SLP) and occupational therapist (OT), among others. These specialists, all serving an integral role, are listed below based on priority (beginning with highest priority). While each play an important/key/invaluable role in the rehabilitation of an individual with LIS, the rankings were determined based on existing literature and consideration of whether the practitioner is ensuring survival or allowing for improvements in quality of life.
For the purposes of this case, we will assume we are physiotherapists who are well acquainted to/well-educated in the realm of cardiorespiratory physiotherapy. If this was not the case, we would include/refer on to a physiotherapist who is confident and competent in this area of specialty. As mentioned in more detail in the intervention section, our role as a physiotherapist would include but not be limited to ensuring ROM and strengthening/ conditioning to prevent atrophy and further health complications which are associated with supine lying or immobility. More specific to our role as cardiorespiratory physiotherapists would be our facilitation of deep breathing exercises, postural drainage and positional changes (Papadopoulou et al., 2019). Acknowledging that these individuals may have restricted voluntary movements, as observed with Gary, positional changes will allow for prevention of contractures (Farr et al., 2021). Further, appreciating the amount of time spent primarily immobile, it is imperative that the OT is included for selection and fitting of an appropriate wheelchair (Farr et al., 2021). This will be discussed below.
During the acute period of LIS, which has occurred secondary to an ischemic stroke of basilar artery, such as in our case, the neurologist would intervene with intraarterial thrombolysis (within 48 hours of the onset of symptoms) (Halan et al., 2021). The next step of acute care, in part provided by us as physiotherapists, is to ensure sufficient oxygenation (Halan et al., 2021). Our efforts would be accompanied with our highest priority referral, the respirologist. Through use of predictive measures such as heart rate and predictive markers, these professionals ensure not only proper airway functioning and adequate oxygen saturation levels, but also stability from a cardiac standpoint (Das et al., 2021). While patients with LIS showcase high prevalence of respiratory complications during hospitalization, a study by Svernling et al. (2019) found that no LIS patients under study, died as a result of respiratory complications. They attributed primarily to thorough care provided by the respirologists who prevent and treated respiratory problems in this population (Svernling et al., 2019).
Our next referral is for Speech Language Pathology (SLP). In addition to respiratory function, swallowing and communication are imperative parts of everyday life. SLPs conduct assessments to evaluate swallowing via video fluoroscopy or fiberoptic endoscopic (Farr et al., 2021). Furthermore, they educate patients on assisted technologies, facilitating use of assisted technology such as infrared eye movement sensors and computer modulated voice tools (Das et al., 2021). Moreover, SLP involvement includes use of/application of VitalStim, a tool which addresses dysphagia through stimulating inactive swallowing muscles (Halan et al., 2019). This form of treatment improves both airway clearance as well as diet status, allowing for progression from NPO to small volumes of liquids and puree solids (Farr et al., 2021; Halan et al., 2019). Speech language therapy can also be accompanied by/supplemented with music therapy (Halan et al., 2019). This co-treatment allowed for improvements in outcomes such as voice output, initiation, and coordination (Halan et al., 2019.)
Next, we believe it is important to refer to Occupational Therapy (OT). With this population, the OT team often works to implement and educate on available technologies, such as the universal ocular piloting system and Computer based augmentative and alternative communication systems (AAC) (Das et al., 2021; Farr et al., 2021; León-Carrión et al., 2002). These eye tracking techniques based on assessment of the patient’s eye shape and size as well as ocular behaviour (i.e.,gaze and movement), allow for improved communication (Das et al., 2021; Farr et al., 2021; León-Carrión et al., 2002). In addition to implementing up and coming communication techniques, the OT plays an important role in patient wheelchair use. The majority of LIS patients will require the long-term use of a wheelchair. For those who achieve only minimal recovery, a tilt-in-space wheelchair is the ideal choice for providing upright position, easy pressure relief, and transportation (Farr et al., 2021). The role of the OT would develop with progressions and developments in Gary’s abilities, allowing for strides in autonomous acts such as self-care and interacting with his environment.
WILL PUT REFERRAL NOTE HERE
Opportunities and Challenges of Utilizing Innovative Technology[edit | edit source]
An opportunity for using innovative robotic interventions is they can get the patient more engaged and make treatment more entertaining. In addition, the machine itself can change its sensitivity based on the severity of the locked-in syndrome, essentially tailoring the difficulty of the movements based on the patient’s current status [13]. This feature provides a more individualized treatment plan for each patient, creating better results and enabling a more effective intervention plan.
With implementing innovative technology, there will be barriers to incorporating it in clinical practice. The first is feasibility. With new and innovative robotic technology, they cost a lot of money to produce, which many clinics don’t have the capacities to afford. In addition, the patient will most likely be unable to afford the robotic and, therefore, won’t be able to practice these techniques at home only when they come in for physiotherapy.
A way to mitigate this situation would be to provide alternative treatments with similar benefits. For example, a NMES machine can induce muscle contractions and potentially target the same goals. Another method would be to develop funding or apply for different funding for the patient, as this is a beneficial technique for individuals with locked-in syndrome. Lastly, you can always refer a patient to another clinic that offers these machines.
Discussion[edit | edit source]
Test Your Knowledge[edit | edit source]
Question 1: Which of the following is NOT a clinical feature of a patient with locked-in syndrome?
a) Quadriplegia
b) Anarthria
c) Loss of cognitive awareness
d) Maintained hearing ability
Question 2: Which of the following is a possible adverse event that must be monitored during physical therapy for an individual with locked-in syndrome?
a) Tingling in the feet
b) Low blood pressure
c) Loss of peripheral vision
d) Nausea/vomiting
Question 3:
*Answers available after the reference list
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 Halan T, Ortiz JF, Reddy D, Altamimi A, Ajibowo AO, Fabara SP. Locked-In syndrome: a systematic review of long-term management and prognosis. Cureus. 2021 Jul 29;13(7).
- ↑ Surdyke L, Fernandez J, Foster H, Spigel P. Differential diagnosis and management of incomplete locked-in syndrome after traumatic brain injury. Case Reports in Neurological Medicine. 2017 Jun 14;2017.
- ↑ 3.0 3.1 Svernling K, Törnbom M, Nordin Å, Sunnerhagen KS. Locked-in syndrome in Sweden, an explorative study of persons who underwent rehabilitation: a cohort study. BMJ open. 2019 Apr 1;9(4):e023185.
- ↑ Ferrucci L, Koh C, Bandinelli S, Guralnik JM. Disability, functional status, and activities of daily living. InEncyclopedia of gerontology 2010 (pp. 427-436). Elsevier Inc..
- ↑ Schnetzer L, McCoy M, Bergmann J, Kunz A, Leis S, Trinka E. Locked-in syndrome revisited. Therapeutic Advances in Neurological Disorders. 2023 Mar;16:17562864231160873.
- ↑ Smith E, Delargy M. Locked-in syndrome. Bmj. 2005 Feb 17;330(7488):406-9.
- ↑ 7.0 7.1 7.2 Casanova E, Lazzari RE, Lotta S, Mazzucchi A. Locked-in syndrome: improvement in the prognosis after an early intensive multidisciplinary rehabilitation. Archives of physical medicine and rehabilitation. 2003 Jun 1;84(6):862-7.
- ↑ 8.0 8.1 8.2 8.3 8.4 Farr E, Altonji K, Harvey RL. Locked‐In Syndrome: Practical Rehabilitation Management. PM&R. 2021 Dec;13(12):1418-28.
- ↑ Baltz M, Lietz HL, Trott-Sausser I, Kalpakjian C, Brown D. Tolerance of a tilt table protocol in an in-patient stroke unit setting: A pilot study. Journal of neurologic physical therapy: JNPT. 2013 Mar;37(1):9.
- ↑ 10.0 10.1 10.2 Høyer E, Normann B, Sørsdal R, Strand LI. Rehabilitation including treadmill therapy for patients with incomplete locked-in syndrome after stroke; a case series study of motor recovery. Brain Injury. 2010 Jan 1;24(1):34-45.
- ↑ 11.0 11.1 Hummelsheim H, Eickhof C. Repetitive sensorimotor training for arm and hand in a patient with locked-in syndrome. Scandinavian journal of rehabilitation medicine. 1999 Dec 1;31(4):250-6.
- ↑ 12.0 12.1 12.2 12.3 Papadopoulou SL, Dionyssiotis Y, Krikonis K, Lаgopati N, Kamenov I, Markoula S. Therapeutic approaches in locked-in syndrome. Folia Medica. 2019 Sep 30;61(3):343-51.
- ↑ 13.0 13.1 13.2 Colomer C, Baldoví A, Torromé S, Navarro MD, Moliner B, Ferri J, Noé E. Efficacy of Armeo® Spring during the chronic phase of stroke. Study in mild to moderate cases of hemiparesis. Neurologia (English Edition). 2013 Jun 1;28(5):261-7.
- ↑ Bartolo M, De Nunzio AM, Sebastiano F, Spicciato F, Tortola P, Nilsson J, Pierelli F. Arm weight support training improves functional motor outcome and movement smoothness after stroke. Functional neurology. 2014 Jan;29(1):15.
- ↑ McNair K, Lutjen M, Langhamer K, Nieves J, Hreha K. Comprehensive, technology-based, team approach for a patient with locked-in syndrome: A case report of improved function & quality of life. Assistive Technology. 2019 Jan 1;31(1):53-8.
Question Answers[edit | edit source]
- c
- b