Psychosocial Considerations in Patellofemoral Pain: Difference between revisions
Carin Hunter (talk | contribs) No edit summary |
Carin Hunter (talk | contribs) No edit summary |
||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Carin Hunter|Carin Hunter]] based on the course by [https://members.physio-pedia.com/course_tutor/claire-robertson// Claire Robertson]<br> '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | <div class="editorbox"> '''Original Editor '''- [[User:Carin Hunter|Carin Hunter]] based on the course by [https://members.physio-pedia.com/course_tutor/claire-robertson// Claire Robertson]<br> '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== Pain and Movement Reasoning Model | == Introduction to the Pain and Movement Reasoning Model == | ||
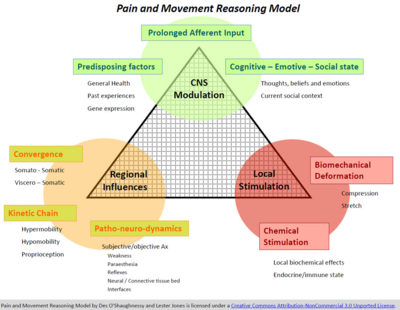
[[File:Pain & Movement Reasoning Model.png|alt=|frameless|400x400px|right]]When considering the psychosocial factors affecting the patellofemoral joint, even though the pain and movement reasoning model was not designed for patellofemoral pain, the theory can be effectively applied. | [[File:Pain & Movement Reasoning Model.png|alt=|frameless|400x400px|right]]When considering the psychosocial factors affecting the patellofemoral joint, even though the pain and movement reasoning model was not designed for patellofemoral pain, the theory can be effectively applied. | ||
When applying this model to patellofemoral pain, local stimulation consists of factors such as bone oedema, fat pad swelling, effusion, retinacular ischaemic changes, bone bruising, or anything local at the knee. Regional influences include excessively pronating feet, an anteverted femoral neck or poor hip abduction control. But there is not much available research to show the role played by the central nervous system. | |||
=== Factors in the Pain and Reasoning Model === | === Factors in the Pain and Reasoning Model === | ||
# '''Local Stimulation'''<ref name=":0">Jones LE, O'Shaughnessy DF. [https://www.sciencedirect.com/science/article/abs/pii/S1356689X14000113 The pain and movement reasoning model: introduction to a simple tool for integrated pain assessment.] Manual therapy. 2014 Jun 1;19(3):270-6.</ref><ref name=":1">O’Shaughnessy D, Jones LE. [https://books.google.co.uk/books?hl=en&lr=&id=dcQIEAAAQBAJ&oi=fnd&pg=PA107&dq=D+O%27Shaughnessy,+LE+Jones+-+Journal:+A+Comprehensive+Guide+to+Sports+Physiology+%E2%80%A6,+2020&ots=PjH08eowVX&sig=Futesk30qJXJbB4RL9fmAS4PcMs&redir_esc=y#v=onepage&q=D%20O'Shaughnessy%2C%20LE%20Jones%20-%20Journal%3A%20A%20Comprehensive%20Guide%20to%20Sports%20Physiology%20%E2%80%A6%2C%202020&f=false Making sense of pain in sports physiotherapy: applying the Pain and Movement Reasoning Model. A Comprehensive Guide to Sports Physiology and Injury Management: an interdisciplinary approach.] 2020 Nov 13:107.</ref> | # '''Local Stimulation'''<ref name=":0">Jones LE, O'Shaughnessy DF. [https://www.sciencedirect.com/science/article/abs/pii/S1356689X14000113 The pain and movement reasoning model: introduction to a simple tool for integrated pain assessment.] Manual therapy. 2014 Jun 1;19(3):270-6.</ref><ref name=":1">O’Shaughnessy D, Jones LE. [https://books.google.co.uk/books?hl=en&lr=&id=dcQIEAAAQBAJ&oi=fnd&pg=PA107&dq=D+O%27Shaughnessy,+LE+Jones+-+Journal:+A+Comprehensive+Guide+to+Sports+Physiology+%E2%80%A6,+2020&ots=PjH08eowVX&sig=Futesk30qJXJbB4RL9fmAS4PcMs&redir_esc=y#v=onepage&q=D%20O'Shaughnessy%2C%20LE%20Jones%20-%20Journal%3A%20A%20Comprehensive%20Guide%20to%20Sports%20Physiology%20%E2%80%A6%2C%202020&f=false Making sense of pain in sports physiotherapy: applying the Pain and Movement Reasoning Model. A Comprehensive Guide to Sports Physiology and Injury Management: an interdisciplinary approach.] 2020 Nov 13:107.</ref> | ||
## Biomechanical Stimulation | ## Biomechanical Stimulation | ||
## Chemical Stimulation | ## Chemical Stimulation | ||
# '''Regional Influences'''<ref name=":0" /><ref name=":1" /> | # '''Regional Influences'''<ref name=":0" /><ref name=":1" /> | ||
## Kinetic Chain | ## Kinetic Chain | ||
## Patho-neuro-dynamics | ## Patho-neuro-dynamics | ||
## Convergence | ## Convergence | ||
# '''Central Nervous System Modulation'''<ref name=":0" /><ref name=":1" /> | # '''Central Nervous System Modulation'''<ref name=":0" /><ref name=":1" /> | ||
## Prolonged Afferent Input | ## Prolonged Afferent Input | ||
## Predisposing Factors | ## Predisposing Factors | ||
| Line 19: | Line 21: | ||
== Mindfulness == | == Mindfulness == | ||
Wride<ref name=":2">Wride J, Bannigan K. [https://www.degruyter.com/document/doi/10.1515/sjpain-2018-0347/html Investigating the prevalence of anxiety and depression in people living with patellofemoral pain in the UK: the Dep-Pf Study.] Scandinavian Journal of Pain. 2019 Apr 1;19(2):375-82.</ref>'s work shows | Wride<ref name=":2">Wride J, Bannigan K. [https://www.degruyter.com/document/doi/10.1515/sjpain-2018-0347/html Investigating the prevalence of anxiety and depression in people living with patellofemoral pain in the UK: the Dep-Pf Study.] Scandinavian Journal of Pain. 2019 Apr 1;19(2):375-82.</ref>'s work shows important correlations with regards to anxiety and depression: | ||
# The prevalence of anxiety and/or depression is higher in the patellofemoral population than the normal population. <ref name=":2" /> | # The prevalence of anxiety and/or depression is higher in the patellofemoral population than the normal population. <ref name=":2" /> | ||
# The prevalence of anxiety and/or depression is higher in young females <ref name=":2" /> | # The prevalence of anxiety and/or depression is higher in young females <ref name=":2" /> | ||
# | # High anxiety scores were more likely female<ref name=":2" /> | ||
# The rate of patellofemoral pain is higher in females<ref>Boling M, Padua D, Marshall S, Guskiewicz K, Pyne S, Beutler A. [https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1600-0838.2009.00996.x Gender differences in the incidence and prevalence of patellofemoral pain syndrome.] Scandinavian journal of medicine & science in sports. 2010 Oct;20(5):725-30.</ref> | |||
When patients had patellofemoral pain, many of them experienced a sense of loss of identity and a loss of social interactions. When an individual has patellofemoral pain which limits them from participating in their sport of choice, we need to consider that it is not only the activity they are suddenly unable to participate in. They also often loose the sense of wellbeing and social interaction that the sport offered. | When patients had patellofemoral pain, many of them experienced a sense of loss of identity and a loss of social interactions. When an individual has patellofemoral pain which limits them from participating in their sport of choice, we need to consider that it is not only the activity they are suddenly unable to participate in. They also often loose the sense of wellbeing and social interaction that the sport offered. | ||
| Line 35: | Line 38: | ||
Another factor to consider is the patients sleep. We should look at the only the quantity or duration of sleep but the quality as well. We should be asking questions such as, How many times does someone wake up in the night? How long does it take to get to sleep? | Another factor to consider is the patients sleep. We should look at the only the quantity or duration of sleep but the quality as well. We should be asking questions such as, How many times does someone wake up in the night? How long does it take to get to sleep? | ||
Bagheri<ref>Bagheri S, Naderi A, Mirali S, Calmeiro L, Brewer BW. [https://meridian.allenpress.com/jat/article/56/8/902/448491/Adding-Mindfulness-Practice-to-Exercise-Therapy Adding mindfulness practice to exercise therapy for female recreational runners with patellofemoral pain: A randomized controlled trial.] Journal of Athletic Training. 2021 Aug 1;56(8):902-11.</ref> | The work carried out by Bagheri<ref name=":3">Bagheri S, Naderi A, Mirali S, Calmeiro L, Brewer BW. [https://meridian.allenpress.com/jat/article/56/8/902/448491/Adding-Mindfulness-Practice-to-Exercise-Therapy Adding mindfulness practice to exercise therapy for female recreational runners with patellofemoral pain: A randomized controlled trial.] Journal of Athletic Training. 2021 Aug 1;56(8):902-11.</ref> showed that when mindfulness was included with physical treatments, there was a greater improvement in pain reduction, catastrophisation, kinesiophobia. The focus of mindfulness is to reduce stress, take control of the situation, stay in control, and not be overly alarmed by it. While as therapists, we are often focussed on reducing pain, if a patient is discharged from treatment with incorrect beliefs regarding their knee pain, they could continue the fear avoidance behaviours and have anxiety while playing their sport.<ref>Smith IV BN. [https://digitalcommons.memphis.edu/etd/1672/ Resiliency, Generalized Self-Efficacy and Mindfulness as Moderators of the Relationship between Stress and both Life Satisfaction and Depression among College Students: An Investigation of the Resilience Process. 2017]</ref> It is important to address the psychosocial factors, as well as the physical ones. | ||
Mindfulness | |||
Mindfulness is aimed at increasing awareness of thoughts, sensations, emotions all with an attitude of acceptance, curiosity and openness.<ref name=":3" /> | |||
==== Tampa Scale of Kinesiophobia ==== | ==== Tampa Scale of Kinesiophobia ==== | ||
Revision as of 18:07, 31 July 2022
Top Contributors - Carin Hunter, Jess Bell, Ewa Jaraczewska, Kim Jackson and Wanda van Niekerk
Introduction to the Pain and Movement Reasoning Model[edit | edit source]
When considering the psychosocial factors affecting the patellofemoral joint, even though the pain and movement reasoning model was not designed for patellofemoral pain, the theory can be effectively applied.
When applying this model to patellofemoral pain, local stimulation consists of factors such as bone oedema, fat pad swelling, effusion, retinacular ischaemic changes, bone bruising, or anything local at the knee. Regional influences include excessively pronating feet, an anteverted femoral neck or poor hip abduction control. But there is not much available research to show the role played by the central nervous system.
Factors in the Pain and Reasoning Model[edit | edit source]
- Local Stimulation[1][2]
- Biomechanical Stimulation
- Chemical Stimulation
- Regional Influences[1][2]
- Kinetic Chain
- Patho-neuro-dynamics
- Convergence
- Central Nervous System Modulation[1][2]
- Prolonged Afferent Input
- Predisposing Factors
- Cognitive - Emotive - Social state
Mindfulness[edit | edit source]
Wride[3]'s work shows important correlations with regards to anxiety and depression:
- The prevalence of anxiety and/or depression is higher in the patellofemoral population than the normal population. [3]
- The prevalence of anxiety and/or depression is higher in young females [3]
- High anxiety scores were more likely female[3]
- The rate of patellofemoral pain is higher in females[4]
When patients had patellofemoral pain, many of them experienced a sense of loss of identity and a loss of social interactions. When an individual has patellofemoral pain which limits them from participating in their sport of choice, we need to consider that it is not only the activity they are suddenly unable to participate in. They also often loose the sense of wellbeing and social interaction that the sport offered.
A few patients have even been known the change career aspirations and housing choices because of their patellofemoral pain. These types of large lifestyle adaptations, due to a belief regarding their knee pain can
Patients can battle with their understanding of the causes of their knee pain, especially when it is of insidious onset. Unlike a traumatic injury, knee pain of insidious onset is not marked by an event which the pain can be attributed to. This can be influential to the incorrect assumption that exercise can worsen the pain. When a physical therapist then prescribes exercise based treatment, a patient can be hesitant and non-compliant due to their beliefs. The patient should be educated on the effects of load, repetitive volume, warm up, cool down, footwear, and many other facets vital to understanding exercise. Treatments that patients felt were of benefit to patellofemoral pain where often passive, primarily painkillers, knee supports, and rest. While these might help the pain temporarily, they will not be beneficial to the patient in the long term.
A study by Selhorst [5] showed that a short educational video shown to a group of adolescents can reduce kinesiophobia, catastrophisation, pain scores, immediately and at two weeks. This shows the significance of education in patellofemoral pain.
Another factor to consider is the patients sleep. We should look at the only the quantity or duration of sleep but the quality as well. We should be asking questions such as, How many times does someone wake up in the night? How long does it take to get to sleep?
The work carried out by Bagheri[6] showed that when mindfulness was included with physical treatments, there was a greater improvement in pain reduction, catastrophisation, kinesiophobia. The focus of mindfulness is to reduce stress, take control of the situation, stay in control, and not be overly alarmed by it. While as therapists, we are often focussed on reducing pain, if a patient is discharged from treatment with incorrect beliefs regarding their knee pain, they could continue the fear avoidance behaviours and have anxiety while playing their sport.[7] It is important to address the psychosocial factors, as well as the physical ones.
Mindfulness is aimed at increasing awareness of thoughts, sensations, emotions all with an attitude of acceptance, curiosity and openness.[6]
Tampa Scale of Kinesiophobia[edit | edit source]
The original Tampa Scale of Kinesiophobia is (TSK) was first developed in 1991 by R. Miller, S. Kopri, and D. Todd. TSK is 17 items a self-reporting questionnaire based on evaluation of fear of movement, fear of physical activity, and fear avoidance. It was first developed to distinguish between non-excessive fear and phobia in patients with chronic musculoskeletal pain, specifically the fear of movement in patients with chronic low back pain then widely used for different parts of the body. The questionnaire using 4 points to assess that are based on; the model of fear-avoidance, fear of work-related activities, fear of movement, and fear of re-injury.[8]
Links:
- Tampa Scale of Kinesiophobia
- Tampa Scale of Kinesiophobia (TSK) pdf
- MDApp, Tampa Scale of Kinesiophobia
Key Questions to ask and why[edit | edit source]
| Question | Reason | Treatment Implication |
| Duration of symptoms | The longer the duration the more likely there will be central pain changes. | Assess for central changes |
| Alteration in sleep quality? | Serotonin (natural painkiller) production suppressed with poor sleep | Recommend re-establishing routine. Non-painful exercise.
Decrease anxiety through education |
| Change in exercise profile? | Can affect sleep, mood, self-esteem, social interactions and conditioning. | Consider exercise programmes for non-painful body parts initially.
Education to minimise fear-avoidance. |
| Can they tolerate the sense of clothing on their knee, eg skinny jeans/tights? | Some patients cannot bear the feeling of material on their knee. Highly suggestive of non-mechanical pain. | Graduated exposure. May need medical management to de-sensitise. |
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Jones LE, O'Shaughnessy DF. The pain and movement reasoning model: introduction to a simple tool for integrated pain assessment. Manual therapy. 2014 Jun 1;19(3):270-6.
- ↑ 2.0 2.1 2.2 O’Shaughnessy D, Jones LE. Making sense of pain in sports physiotherapy: applying the Pain and Movement Reasoning Model. A Comprehensive Guide to Sports Physiology and Injury Management: an interdisciplinary approach. 2020 Nov 13:107.
- ↑ 3.0 3.1 3.2 3.3 Wride J, Bannigan K. Investigating the prevalence of anxiety and depression in people living with patellofemoral pain in the UK: the Dep-Pf Study. Scandinavian Journal of Pain. 2019 Apr 1;19(2):375-82.
- ↑ Boling M, Padua D, Marshall S, Guskiewicz K, Pyne S, Beutler A. Gender differences in the incidence and prevalence of patellofemoral pain syndrome. Scandinavian journal of medicine & science in sports. 2010 Oct;20(5):725-30.
- ↑ Selhorst M, Fernandez-Fernandez A, Schmitt L, Hoehn J. Effect of a Psychologically Informed Intervention to Treat Adolescents With Patellofemoral Pain: A Randomized Controlled Trial. Archives of Physical Medicine and Rehabilitation. 2021 Jul 1;102(7):1267-73.
- ↑ 6.0 6.1 Bagheri S, Naderi A, Mirali S, Calmeiro L, Brewer BW. Adding mindfulness practice to exercise therapy for female recreational runners with patellofemoral pain: A randomized controlled trial. Journal of Athletic Training. 2021 Aug 1;56(8):902-11.
- ↑ Smith IV BN. Resiliency, Generalized Self-Efficacy and Mindfulness as Moderators of the Relationship between Stress and both Life Satisfaction and Depression among College Students: An Investigation of the Resilience Process. 2017
- ↑ Hudes K. The Tampa Scale of Kinesiophobia and neck pain, disability and range of motion: a narrative review of the literature. The Journal of the Canadian Chiropractic Association. 2011 Sep;55(3):222.