Alveoli: Difference between revisions
No edit summary |
No edit summary |
||
| Line 17: | Line 17: | ||
== Function == | == Function == | ||
A typical pair of human lungs contain about 480 million alveoli. This produces 50 to 75 square meters (540 to 810 sq ft) of surface area.<ref>Stanton, Bruce M.; Koeppen, Bruce A., eds. (2008). Berne & Levy physiology (6th ed.). Philadelphia: Mosby/Elsevier. pp. 418–422. <nowiki>ISBN 978-0-323-04582-7</nowiki>.</ref> | A typical pair of human lungs contain about 480 million alveoli. This produces 50 to 75 square meters (540 to 810 sq ft) of surface area.<ref name=":0">Stanton, Bruce M.; Koeppen, Bruce A., eds. (2008). Berne & Levy physiology (6th ed.). Philadelphia: Mosby/Elsevier. pp. 418–422. <nowiki>ISBN 978-0-323-04582-7</nowiki>.</ref> | ||
Alveolar cells | Alveolar cells have several different types according to function. Two major types are '''pneumocytes''' (Type I cells) or '''pneumonocytes''' (Type II cells). They are found in the alveolar wall and a large phagocytic cell known as an alveolar macrophage<ref name=":1">https://www.atsjournals.org/doi/full/10.1164/rccm.2210007</ref> that moves about in the lumens of the alveoli, and in the connective tissue between them. | ||
[[File:Original.jpg|center|thumb]] | |||
=== Type I cells === | === Pneumocytes (Type I cells) === | ||
They are thin, squamous and flat epithelial lining cells that form the structure of the alveoli.<ref name=":2">Knudsen, L; Ochs, M (December 2018). [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6267411 "The micromechanics of lung alveoli: structure and function of surfactant and tissue components"]. ''Histochemistry and Cell Biology''. '''150''' (6): 661–676. doi:[https://doi.org/10.1007%2Fs00418-018-1747-9 10.1007/s00418-018-1747-9]. PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6267411 6267411]. PMID [https://pubmed.ncbi.nlm.nih.gov/30390118 30390118].</ref> The have long cytoplasmic extensions that cover beyond 95% of the alveolar surface.<ref name=":0" /> The thin lining enables a fast diffusion of gas exchange between the air in the alveoli and the blood in the surrounding capillaries. The nucleus of the cell occupies a large area of free cytoplasm and its organelles are clustered around it reducing the thickness of the cell. This helps keeps the thickness of the blood-air barrier reduced to a minimum.The relatively low solubility of oxygen, necessitates the large internal surface area and very thin walls of the alveoli. | |||
The cytoplasm in the thin portion contains pinocytotic vesicles which may play a role in the removal of small particulate contaminants from the outer surface. In addition to desmosomes, all type I alveolar cells have occluding junctions that prevent the leakage of tissue fluid into the alveolar air space. To permit expansion and contraction of the walls during breathing, type I cells have a mesh-like fabric of elastic and collagenous fibers. the fibers allow for firmness and ekasticity. | |||
Type I pneumocytes are unable to replicate and are susceptible to toxic insults. These are the larger of the two cell types. In the event of damage, type II cells can proliferate and differentiate into type I cells to compensate. | |||
=== Pneumonocytes (Type II cells) === | |||
These are cuboidal and much smaller and numerous than type I cells.<ref name=":2" /> Type II cells in the alveolar wall contain secretory organelles known as lamellar bodies that fuse with the cell membranes and secrete pulmonary surfactant. This surfactant is a film of fatty substances that reduce alveolar surface tension. Continously released by exocytosis,the coating prevents the alveoli from collapse. The fluid coating is produced by the body in order to facilitate the transfer of gases between blood and alveolar air, and the type II cells are typically found at the blood-air barrier.<ref>Fehrenbach H (2001). [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC59567 "Alveolar epithelial type II cell: defender of the alveolus revisited"]. ''Respiratory Research''. '''2''' (1): 33–46. doi:[https://doi.org/10.1186%2Frr36 10.1186/rr36]. PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC59567 59567]. PMID [https://pubmed.ncbi.nlm.nih.gov/11686863 11686863].</ref> | |||
The alveolar macrophages (dust cells) reside on the internal lumenal surfaces of the alveoli, the alveolar ducts, and the bronchioles. They are mobile scavengers that serve to engulf foreign particles in the lungs, such as dust, bacteria, carbon particles, and blood cells from injuries.<ref name=":1" /> | |||
== Clinical relevance == | == Clinical relevance == | ||
| Line 49: | Line 40: | ||
=== Diseases === | === Diseases === | ||
==== Surfactant ==== | ==== Surfactant<ref>https://www.mpg.de/14673057/using-alveolar-epithelia-as-a-model-for-corona-infection</ref> ==== | ||
Type II cells start to develop at about 26 weeks of gestation, secreting small amounts of surfactant. However, adequate amounts of surfactant are not secreted until about 35 weeks of gestation – this is the main reason for increased rates of infant respiratory distress syndrome, which drastically reduces at ages above 35 weeks gestation. | |||
==== Inflammation ==== | ==== Inflammation ==== | ||
| Line 58: | Line 50: | ||
==== Coronavirus ==== | ==== Coronavirus ==== | ||
MUC1, a human gene associated with type II pneumocytes, has been identified as a marker in lung cancer.<sup>[18</sup> | |||
== Assessment == | == Assessment == | ||
Revision as of 15:45, 14 January 2021
This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! (14/01/2021)
Original Editor -
Top Contributors - Anthonia Abraham, Lucinda hampton and Kalyani Yajnanarayan
Description[edit | edit source]
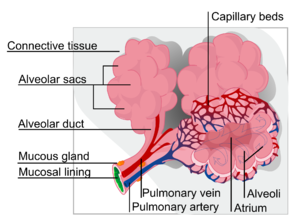
Pulmonary Alveolus ( Plural; Alveoli) are tiny air sacs that function as basic respiratory units. It is a hollow cup-shaped cavity in the lung parenchyma where gas exchange takes place. Lung alveoli are found in the acini at the beginning of the respiratory zone. They are located sparsely in the respiratory bronchioles, lining the walls of the alveolar ducts. The alveoli are located in the alveolar sacs of the lungs in the pulmonary lobules of the respiratory zone. They are more numerous in the blind-ended alveolar sacs.[1]
Respiratory bronchioles lead into alveolar ducts which are deeply lined with alveoli. Each respiratory bronchiole gives rise to between two and eleven alveolar ducts. Each duct opens into five or six alveolar sacs into which clusters of alveoli open. The number of alveoli in the human lung increased exponentially during the first 2 yr of life but continued to increase albeit at a reduced rate through adolescence.[2].
The alveolar membrane is the gas exchange surface, surrounded by a network of capillaries[3].
Function[edit | edit source]
A typical pair of human lungs contain about 480 million alveoli. This produces 50 to 75 square meters (540 to 810 sq ft) of surface area.[4]
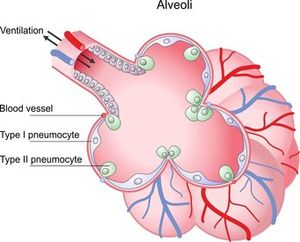
Alveolar cells have several different types according to function. Two major types are pneumocytes (Type I cells) or pneumonocytes (Type II cells). They are found in the alveolar wall and a large phagocytic cell known as an alveolar macrophage[5] that moves about in the lumens of the alveoli, and in the connective tissue between them.
Pneumocytes (Type I cells)[edit | edit source]
They are thin, squamous and flat epithelial lining cells that form the structure of the alveoli.[6] The have long cytoplasmic extensions that cover beyond 95% of the alveolar surface.[4] The thin lining enables a fast diffusion of gas exchange between the air in the alveoli and the blood in the surrounding capillaries. The nucleus of the cell occupies a large area of free cytoplasm and its organelles are clustered around it reducing the thickness of the cell. This helps keeps the thickness of the blood-air barrier reduced to a minimum.The relatively low solubility of oxygen, necessitates the large internal surface area and very thin walls of the alveoli.
The cytoplasm in the thin portion contains pinocytotic vesicles which may play a role in the removal of small particulate contaminants from the outer surface. In addition to desmosomes, all type I alveolar cells have occluding junctions that prevent the leakage of tissue fluid into the alveolar air space. To permit expansion and contraction of the walls during breathing, type I cells have a mesh-like fabric of elastic and collagenous fibers. the fibers allow for firmness and ekasticity.
Type I pneumocytes are unable to replicate and are susceptible to toxic insults. These are the larger of the two cell types. In the event of damage, type II cells can proliferate and differentiate into type I cells to compensate.
Pneumonocytes (Type II cells)[edit | edit source]
These are cuboidal and much smaller and numerous than type I cells.[6] Type II cells in the alveolar wall contain secretory organelles known as lamellar bodies that fuse with the cell membranes and secrete pulmonary surfactant. This surfactant is a film of fatty substances that reduce alveolar surface tension. Continously released by exocytosis,the coating prevents the alveoli from collapse. The fluid coating is produced by the body in order to facilitate the transfer of gases between blood and alveolar air, and the type II cells are typically found at the blood-air barrier.[7]
The alveolar macrophages (dust cells) reside on the internal lumenal surfaces of the alveoli, the alveolar ducts, and the bronchioles. They are mobile scavengers that serve to engulf foreign particles in the lungs, such as dust, bacteria, carbon particles, and blood cells from injuries.[5]
Clinical relevance[edit | edit source]
Diseases[edit | edit source]
Surfactant[8][edit | edit source]
Type II cells start to develop at about 26 weeks of gestation, secreting small amounts of surfactant. However, adequate amounts of surfactant are not secreted until about 35 weeks of gestation – this is the main reason for increased rates of infant respiratory distress syndrome, which drastically reduces at ages above 35 weeks gestation.
Inflammation[edit | edit source]
Structural[edit | edit source]
Fluid[edit | edit source]
[edit | edit source]
MUC1, a human gene associated with type II pneumocytes, has been identified as a marker in lung cancer.[18
Assessment[edit | edit source]
Visual inspection can be used to appreciate the level of distress, use of accessory muscles, respiratory position, chest structure, respiratory pattern, and other clues outside of the chest.[9]
The pulmonary examination consists of inspection, palpation, percussion, and auscultation. The inspection process initiates and continues throughout the patient encounter. Palpation, confirmed by percussion, assesses for tenderness and degree of chest expansion. Auscultation, a more sensitive process, confirms earlier findings and may help to identify specific pathologic processes not previously recognized.[10]
Resources[edit | edit source]
- ↑ Moore K (2018). Clinically oriented anatomy. Wolters Kluwer. p. 336. ISBN .
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4137164/
- ↑ Paxton S, Peckham M, Knibbs A (2003). "Functions of the Respiratory Portion". The Leeds Histology Guide. Faculty of Biological Sciences, University of Leeds.
- ↑ 4.0 4.1 Stanton, Bruce M.; Koeppen, Bruce A., eds. (2008). Berne & Levy physiology (6th ed.). Philadelphia: Mosby/Elsevier. pp. 418–422. ISBN 978-0-323-04582-7.
- ↑ 5.0 5.1 https://www.atsjournals.org/doi/full/10.1164/rccm.2210007
- ↑ 6.0 6.1 Knudsen, L; Ochs, M (December 2018). "The micromechanics of lung alveoli: structure and function of surfactant and tissue components". Histochemistry and Cell Biology. 150 (6): 661–676. doi:10.1007/s00418-018-1747-9. PMC 6267411. PMID 30390118.
- ↑ Fehrenbach H (2001). "Alveolar epithelial type II cell: defender of the alveolus revisited". Respiratory Research. 2 (1): 33–46. doi:10.1186/rr36. PMC 59567. PMID 11686863.
- ↑ https://www.mpg.de/14673057/using-alveolar-epithelia-as-a-model-for-corona-infection
- ↑ https://emedicine.medscape.com/article/1909159-technique
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK368/