Anthrax: Difference between revisions
No edit summary |
No edit summary |
||
| Line 31: | Line 31: | ||
In 1978, during the Rhodesian civil war, failure of veterinary vaccination programs led to a human epidemic, causing 6500 anthrax cases and 100 fatalities.<ref name=":1" /> | In 1978, during the Rhodesian civil war, failure of veterinary vaccination programs led to a human epidemic, causing 6500 anthrax cases and 100 fatalities.<ref name=":1" /> | ||
In 1982, Thailand had an outbreak of 24 cases, concurrently with 52 cases of cutaneous anthrax after ingestion of contaminated water buffalo meat.<ref name=":1" /> | |||
In October 2001, 22 cases of anthrax infection were identified.<ref name=":1" /> Most recently in 2016, in Siberia, Russia, there was an outbreak of anthrax that affected at least 13 Siberian people and killed over 2,000 reindeer.<ref name=":2" /> | In October 2001, 22 cases of anthrax infection were identified.<ref name=":1" /> Most recently in 2016, in Siberia, Russia, there was an outbreak of anthrax that affected at least 13 Siberian people and killed over 2,000 reindeer.<ref name=":2" /> | ||
| Line 71: | Line 73: | ||
Fever and chills | Fever and chills | ||
Swelling of neck | Swelling of neck and lymph node enlargement | ||
Sore throat | Sore throat | ||
Painful swallowing | Painful swallowing | ||
Dysphagia | |||
Respiratory distress | |||
Oral bleeding | |||
Hoarseness | Hoarseness | ||
Nausea and vomiting | Nausea and vomiting or hematemesis | ||
Diarrhea or bloody diarrhea | Diarrhea or bloody diarrhea | ||
| Line 99: | Line 107: | ||
Shortness of breath | Shortness of breath | ||
Tachypnea | |||
Cyanosis | |||
Confusion or dizziness | Confusion or dizziness | ||
| Line 104: | Line 116: | ||
Cough | Cough | ||
Nausea, vomiting, or stomach pains | Nausea, vomiting (hematemesis), or stomach pains | ||
Headache | Headache | ||
Diaphoresis | |||
Extreme tiredness | Extreme tiredness | ||
| Line 140: | Line 152: | ||
[https://wwwn.cdc.gov/nndss/conditions/anthrax/case-definition/2010/ Case Definition] | [https://wwwn.cdc.gov/nndss/conditions/anthrax/case-definition/2010/ Case Definition] | ||
=== Diagnostic Procedures === | === Diagnostic Procedures/ Laboratory Findings === | ||
* Gram Staining and Blood Culture | |||
* Enzyme-Linked Immunosorbent Assay (ELISA) | |||
** ELISA to detect immunoglobulin G (IgG) response to ''B anthracis'' protective antigen (PA) is 98.6% sensitive and 80% specific. Protective antigen–competitive inhibition ELISA is used as a second confirmatory step to improve specificity.<ref name=":1" /> | |||
* Chest Radiograph | |||
** widening of the mediastinum,paratracheal and hilar fullness, and pleural effusions<ref name=":1" /> | |||
* CT Scan | |||
** detects hemorrhagic mediastinal and hilar lymph nodes and edema, peribronchial thickening, and pleural effusions<ref name=":1" /> | |||
* Lumbar Puncture | |||
** CSF in patients with anthrax meningitis is grossly hemorrhagic with few polymorphonuclear neutrophils (PMNs) and numerous gram-positive bacilli.<ref name=":1" /> | |||
* Histologic Findings | |||
<br> | <br> | ||
| Line 153: | Line 174: | ||
Antibiotics | Antibiotics | ||
Antitoxins | |||
=== Physiotherapy Management === | === Physiotherapy Management === | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
<br> | === Cutaneous Anthrax === | ||
Bubonic Plague | |||
Primary Syphyilis | |||
=== Gastrointestinal Anthrax === | |||
Dysentery | |||
=== Inhalational Anthrax === | |||
[[Pneumonia]] (Atypcial or Community- Acquired) | |||
Bacterial Mediastinitis<br> | |||
=== Other Conditions: === | |||
[[Tularemia]] | |||
Typhoid | |||
Diphtheria | |||
Psittacosis | |||
Leprosy | |||
== Resources == | == Resources == | ||
Revision as of 07:41, 2 April 2020
This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! (2/04/2020)
Definition[edit | edit source]
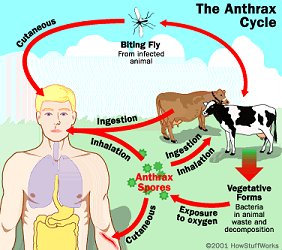
Anthrax is an acute zoonotic disease caused by the spore-forming bacterium Bacillus anthracis, a microbe that lives in the soil.[1]
- A serious infectious disease caused by gram-positive, rod-shaped bacteria known as Bacillus anthracis.[2]
- Anthrax can be found naturally in soil and commonly affects domestic and wild animals around the world.[2]
- Rare in the United States - people can get sick with anthrax if they come in contact with infected animals or contaminated animal products.[2]
- Contact with anthrax can cause severe illness in both humans and animals.[2]
- Anthrax is not contagious, which means you can’t catch it like the cold or flu.[2]
- Anthrax can occur in four forms: cutaneous, inhalation, gastrointestinal, and inhalation.[2]
Clinically Relevant Anatomy[edit | edit source]
Anthrax can affect different body systems, depending on the route of infection. It can affect the integumentary system, gastrointestinal/ digestive system and respiratory system.
Etiology[edit | edit source]
The pathogen that causes Anthrax is a bacterium known as Bacillus anthracis.
Epidemiology[edit | edit source]
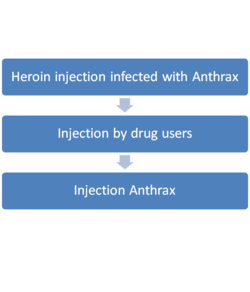
Most cases of anthrax are cutaneous (95%); the remaining cases are inhalation (5%) and gastrointestinal (< 1%).[3] Injection Anthrax have only been reported in Northern Europe.[2][4]
Incidence of any anthrax infection has been less than 1 case per year in the US for the last 30 years. From 1955–1994, US cases totaled 235, with 224 cases of cutaneous anthrax, 11 cases of inhalation anthrax, and 20 fatalities.[3]
Anthrax is common in Middle East, the Indian subcontinent, Africa, Asia, and Latin America and is rare in Western Europe. In 1958, approximately 100,000 cases of anthrax occurred worldwide. Anthrax is endemic in Africa and Asia despite vaccination programs.[3]
In 1978, during the Rhodesian civil war, failure of veterinary vaccination programs led to a human epidemic, causing 6500 anthrax cases and 100 fatalities.[3]
In 1982, Thailand had an outbreak of 24 cases, concurrently with 52 cases of cutaneous anthrax after ingestion of contaminated water buffalo meat.[3]
In October 2001, 22 cases of anthrax infection were identified.[3] Most recently in 2016, in Siberia, Russia, there was an outbreak of anthrax that affected at least 13 Siberian people and killed over 2,000 reindeer.[4]
Risk Factors[edit | edit source]
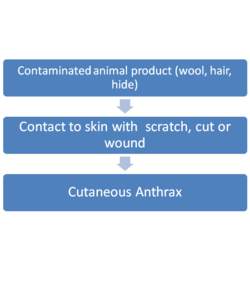
Occupational hazard for:
- Veterinarians
- Farmers
- Individuals who handle animal wool, hair, hides, or bone meal products.[3]
- Travelers
- Laboratory professionals
- Mail handlers, military personnel, and response workers who may be exposed during a bioterror event involving anthrax spores[2]
There is no racial, sexual, or age predilection for anthrax. However, because anthrax is often related to industrial exposure and farming, the disease most often affects young and middle-aged adults.[3]
Pathophysiology[edit | edit source]
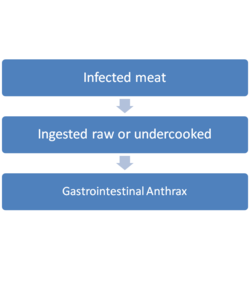
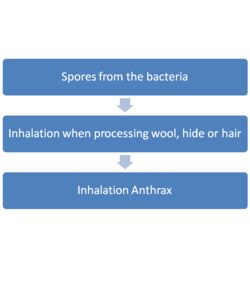
Anthrax can occur in four different forms, depending on the route of infection.
|
|
|
|
When the spores get inside the body, from any route mentioned from above, the spores then become anthrax bacteria. Then the bacteria can multiply, spread out in the body, produce toxins (poisons), and cause severe illness. [2]
Clinical Presentation[edit | edit source]
Clinical manifestations usually happen 1-7 days after exposure from the spores.
Cutaneous Anthrax[edit | edit source]
Small blisters/ bumps
Swelling
Painless skin sore (ulcer), most often the sore will be on the face, neck, arms, or hands[2]
Gastrointestinal Anthrax[edit | edit source]
Fever and chills
Swelling of neck and lymph node enlargement
Sore throat
Painful swallowing
Dysphagia
Respiratory distress
Oral bleeding
Hoarseness
Nausea and vomiting or hematemesis
Diarrhea or bloody diarrhea
Headache
Flushing (red face) and red eyes
Stomach pain
Fainting
Swelling of abdomen (stomach)
Inhalation Anthrax[edit | edit source]
Fever and chills
Chest Discomfort
Shortness of breath
Tachypnea
Cyanosis
Confusion or dizziness
Cough
Nausea, vomiting (hematemesis), or stomach pains
Headache
Diaphoresis
Extreme tiredness
Body aches
Injection Anthrax[edit | edit source]
Injection anthrax has almost the same manifestation as Cutaneous Anthrax except for it could affect deeper structures and can spread more easily.[2]
Fever and chills
A group of small blisters or bumps that may itch, appearing where the drug was injected
A painless skin sore with a black center that appears after the blisters or bumps
Swelling around the sore
Abscesses deep under the skin or in the muscle where the drug was injected
Diagnosis[edit | edit source]
Diagnosis is made through history-taking for possible exposure, evaluation of signs and symptoms, diagnostic procedures, and laboratory findings.
The Centers for Disease Control and Prevention (CDC) has resources that can help in diagnosing and investigating anthrax. These are:
Anthrax Case Investigation System
Anthrax Investigation Database
Diagnostic Procedures/ Laboratory Findings[edit | edit source]
- Gram Staining and Blood Culture
- Enzyme-Linked Immunosorbent Assay (ELISA)
- ELISA to detect immunoglobulin G (IgG) response to B anthracis protective antigen (PA) is 98.6% sensitive and 80% specific. Protective antigen–competitive inhibition ELISA is used as a second confirmatory step to improve specificity.[3]
- Chest Radiograph
- widening of the mediastinum,paratracheal and hilar fullness, and pleural effusions[3]
- CT Scan
- detects hemorrhagic mediastinal and hilar lymph nodes and edema, peribronchial thickening, and pleural effusions[3]
- Lumbar Puncture
- CSF in patients with anthrax meningitis is grossly hemorrhagic with few polymorphonuclear neutrophils (PMNs) and numerous gram-positive bacilli.[3]
- Histologic Findings
Outcome Measures[edit | edit source]
Management / Interventions[edit | edit source]
The CDC has a set of guidelines for the Prevention and Treatment of Anthrax.
Medical Management[edit | edit source]
Antibiotics
Antitoxins
Physiotherapy Management[edit | edit source]
Differential Diagnosis[edit | edit source]
Cutaneous Anthrax[edit | edit source]
Bubonic Plague
Primary Syphyilis
Gastrointestinal Anthrax[edit | edit source]
Dysentery
Inhalational Anthrax[edit | edit source]
Pneumonia (Atypcial or Community- Acquired)
Bacterial Mediastinitis
Other Conditions:[edit | edit source]
Typhoid
Diphtheria
Psittacosis
Leprosy
Resources[edit | edit source]
CDC- Anthrax
CDC- Anthrax Resources- for additional readings
References[edit | edit source]
- ↑ U.S. National Library of Medicine. National Institute of Health. Medline Plus. Anthrax.http://www.nlm.nih.gov/medlineplus/anthrax.html (accessed 2 March 2011)
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 CDC- Anthrax- Basic Information. Available at https://www.cdc.gov/anthrax/basics/index.html (Accessed March 30, 2020)
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 Medscape- Anthrax. Available at https://emedicine.medscape.com/article/212127-overview (Accessed March 31, 2020)
- ↑ 4.0 4.1 Medicinenet- Anthrax. Available at https://www.medicinenet.com/anthrax/article.htm#anthrax_facts (Accessed March 31, 2020)