Pneumocystis Jirovecii Pneumonia: Difference between revisions
No edit summary |
No edit summary |
||
| Line 56: | Line 56: | ||
Thorough evaluation that includes physical examination, laboratory findings and/or imaging studies are warranted in order to make a specific diagnosis of PJP and to differentiate it from other conditions with similar presentation, which include but not limited to: | Thorough evaluation that includes physical examination, laboratory findings and/or imaging studies are warranted in order to make a specific diagnosis of PJP and to differentiate it from other conditions with similar presentation, which include but not limited to: | ||
* Bacterial [[pneumonia]]<ref name=":4" /> | |||
Bacterial pneumonia<ref name=":4" /> | * [[Acute Respiratory Distress Syndrome (ARDS)|Acute Respiratory Distress Syndrome]]<ref name=":3" /> | ||
* Viral [[pneumonia]] | |||
Acute Respiratory Distress Syndrome<ref name=":3" /> | * Pulmonary Tuberculosis<ref name=":4" /> | ||
* [[Pulmonary Embolism]]<ref name=":3" /> | |||
Viral pneumonia | * Mycobacterium Avium Complex<ref name=":3" /> | ||
* [[Cytomegalovirus (CMV) Infection|Cytomegalovirus]]<ref name=":4" /> | |||
Pulmonary Tuberculosis<ref name=":4" /> | * Histoplasmosis | ||
Pulmonary Embolism<ref name=":3" /> | |||
Mycobacterium Avium Complex | |||
Cytomegalovirus<ref name=":4" /> | |||
Histoplasmosis | |||
== Prognosis == | == Prognosis == | ||
Revision as of 12:25, 16 February 2020
Introduction[edit | edit source]
Pneumocystis Jirovecii Pneumonia (PJP) was previously called as Pneumocystis Carinii Pneumonia (PCP), it is one of the most common opportunistic fungal infection in immuno-compromised conditions such as haematological malignancy, congenital immunodeficiency, organ transplantation, immunosuppressive therapy, under medication and predominantly in HIV/AIDS. [1]
Epidemiology[edit | edit source]
PJP has a high incidence before the advent of prophylaxis treatment and highly active antiretroviral therapy (HAART). A study about the epidemiology of PJP showed that the incidence has significantly decreased both for the adult and pediatric population.[2] However, the same study showed that there is difference with the prevalence of PJP in industrialized countries, such as those in Europe and North America, and in developing countries , such as in Southeast Asia and Sub-Saharan Africa, wherein the former has a continuous decline while the latter is at a greater risk of incidence.[2]
A recent nationwide study in Spain, conducted by Pereira-Diaz et al, reported that PJP is an emerging disease in patients without HIV infection of which risk factors include haematological neoplasms, chronic lung diseases and, non-hematological cancers with high mean mortality and hospitalization costs.[3]
Etiology[edit | edit source]
The pathogen responsible for PJP is Pneumocystis Jirovecii, an organism classified as a fungus.
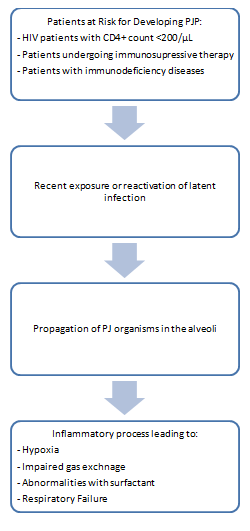
Pathophysiology[edit | edit source]
Signs and Symptoms[edit | edit source]
- Subacute onset exertional dyspnea[4]
- Dry and non-productive cough[4]
- Fever or subfebrile temperatures[4]
- Chest pain
- Tachypnea
- Tachycardia
- Cyanosis
- Weight loss
Diagnostic Procedures[edit | edit source]
Diagnosis of PJP relies on combination of laboratory findings and diagnostic imaging together with physical examination and history-taking.
Laboratory procedures and findings pertinent to PJP diagnosis include:
- Quantitative polymerase chain reaction (qPCR)- more accurate way to diagnose PJP[5]
- (1–3)-β-d-glucan (BG) -most reliable serologic biomarker for PJP diagnosis[6]
- Krebs von den Lungen-6 antigen (KL-6)- together with BG, is the most accurate serologic apptoach for PJP diagnosis[6]
- Lactate dehydrogenase (LDH)[6]
- S-adenosyl methionine (SAM)[6]
- Sputum induction
Imaging studies used in the diagnosis of PJP include:
Chest CT Scan- most pertinent finding is ground glass opacity (GGO) indicative of alveolar subtotal consolidation[7]
Chest Radiography- nonspecific, can be normal, less common patterns have been reported, including lobar infiltrates, pulmonary nodules, and pneumatoceles and other cystic changes.[8]
Differential Diagnosis[edit | edit source]
Thorough evaluation that includes physical examination, laboratory findings and/or imaging studies are warranted in order to make a specific diagnosis of PJP and to differentiate it from other conditions with similar presentation, which include but not limited to:
- Bacterial pneumonia[8]
- Acute Respiratory Distress Syndrome[1]
- Viral pneumonia
- Pulmonary Tuberculosis[8]
- Pulmonary Embolism[1]
- Mycobacterium Avium Complex[1]
- Cytomegalovirus[8]
- Histoplasmosis
Prognosis[edit | edit source]
Pharmacological Management[edit | edit source]
Physiotherapy Intervention[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Kante, Meenakshi & Racherla, Rishi & Usha, Kalawat. (2019). Pneumocystis jirovecii Pneumonia: A Revisit to the Old Malady. JOURNAL OF CLINICAL AND DIAGNOSTIC RESEARCH. 10.7860/JCDR/2019/42636.13318 retrieved from https://www.researchgate.net/publication/337105006_Pneumocystis_jirovecii_Pneumonia_A_Revisit_to_the_Old_Malady
- ↑ 2.0 2.1 Morris A, Lundgren JD, Masur H, et al. Current epidemiology of Pneumocystis pneumonia. Emerg Infect Dis. 2004;10(10):1713–1720. doi:10.3201/eid1010.030985 retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3323247/
- ↑ Pereira-Díaz E, Moreno-Verdejo F, de la Horra C, Guerrero JA, Calderón EJ, Medrano FJ. Changing Trends in the Epidemiology and Risk Factors of Pneumocystis Pneumonia in Spain. Front Public Health. 2019;7:275. Published 2019 Oct 4. doi:10.3389/fpubh.2019.00275 retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6788256/
- ↑ 4.0 4.1 4.2 Salzer H, J, F, Schäfer G, Hoenigl M, Günther G, Hoffmann C, Kalsdorf B, Alanio A, Lange C: Clinical, Diagnostic, and Treatment Disparities between HIV-Infected and Non-HIV-Infected Immunocompromised Patients with <b><i>Pneumocystis jirovecii</i></b> Pneumonia. Respiration 2018;96:52-65. doi: 10.1159/000487713 retrieved from https://www.karger.com/Article/FullText/487713#
- ↑ Alanio A, Bretagne S. Pneumocystis jirovecii detection in asymptomatic patients: what does its natural history tell us?. F1000Res. 2017;6:739. Published 2017 May 23. doi:10.12688/f1000research.10619.1 retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5464226/
- ↑ 6.0 6.1 6.2 6.3 Esteves F., Calé S. S., Badura R., De Boer M. G., Maltez F., Calderon E. J., et al. (2015). Diagnosis of Pneumocystis pneumonia: evaluation of four serologic biomarkers. Clin. Microbiol. Infect. 21:379.e1–e10. 10.1016/j.cmi.2014.11.025 retrieved from https://www.sciencedirect.com/science/article/pii/S1198743X14001116
- ↑ Ebner L, Walti LN, Rauch A, et al. Clinical Course, Radiological Manifestations, and Outcome of Pneumocystis jirovecii Pneumonia in HIV Patients and Renal Transplant Recipients. PLoS One. 2016;11(11):e0164320. Published 2016 Nov 8. doi:10.1371/journal.pone.0164320 retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5100884/
- ↑ 8.0 8.1 8.2 8.3 Tasaka, S. (2015). Pneumocystis Pneumonia in Human Immunodeficiency Virus–infected Adults and Adolescents: Current Concepts and Future Directions. Clinical Medicine Insights: Circulatory, Respiratory and Pulmonary Medicine. https://doi.org/10.4137/CCRPM.S23324 retrieved from https://journals.sagepub.com/doi/full/10.4137/CCRPM.S23324#articleCitationDownloadContainer