Muscle Length Assessment and Treatment Related to Patellofemoral Pain: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) No edit summary |
||
| (34 intermediate revisions by 3 users not shown) | |||
| Line 2: | Line 2: | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Introduction == | |||
Patellofemoral pain often results from cumulative load. It reveals itself with prolonged and or repetitive activity or holding of a certain position. Subtle changes in load can add up over time to create a large load.<ref name=":0" /> Thorough assessment and the subjective interview will provide clues to causative factors of the patient's patellofemoral pain. | |||
For a review of the gait cycle, please read [[Gait#The Gait Cycle|this article]]. | |||
== Hamstrings == | |||
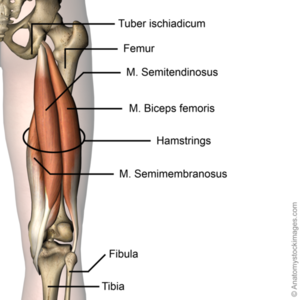
[[File:Hip-hamstring-hamstrings-semi-membranosis-biceps-femoris-semitendinosus-tuber-ischiadicum-back-skin-names.png|Hamstrings in situ. Note their relationship with the knee.|alt=|thumb]] | |||
'''Why is it mechanically relevant to assess this muscle?''' | |||
* Tight, tense, and shortened hamstrings can pull the knee into excessive knee flexion. During the gait cycle, this can result in a greater knee flexion moment at initial contact or heel strike. | |||
* Any resulting increase in knee flexion will increase patellofemoral contact pressures. Therefore, it is important to avoid the situation where the tibia is being pulled back and there is enhanced knee flexion.<ref name=":0">Robertson, C. Patellofemoral Joint Programme. Muscle Length Assessment and Treatment Related to Patellofemoral Pain. Physioplus. 2022.</ref> | |||
'''How should we assess and test for muscle length?''' | |||
* It is important to assess hamstring length in conjunction with stride length | |||
* Bedside clinical exams: [[Sit and Reach Test|sit-and-reach]], [[Straight Leg Raise Test|straight leg raise]] | |||
* It is important to assess and compare the muscle length of both hamstrings. The rehabilitation professional should also take the patient's relative flexibility into consideration, ie: is this patient's body flexible overall or tight. This will help determine the patient's muscle length norm. | |||
* Other muscle groups to assess: [[Gluteal Muscles|gluteal extensors]] | |||
* Clues from the patient interview or past medical history: a patient may state that they stretch regularly but have not noticed any change in their flexibility; a history of repeated injury to a muscle group might mean that it has more scarring in the intramuscular matter; having regular repeating injuries.<ref name=":0" /> | |||
''' | '''What treatments can we offer?''' | ||
* | * The literature gives little insight into the duration or frequency of stretching.<ref name=":0" /> | ||
* | * Consistent, regular stretching that the patient will be able to complete is key. Find out about the patient's schedule and lifestyle and help them create an exercise programme they will be able to stick to and faithfully perform. Create easy, pragmatic exercises the patient will most likely complete.<ref name=":0" /> | ||
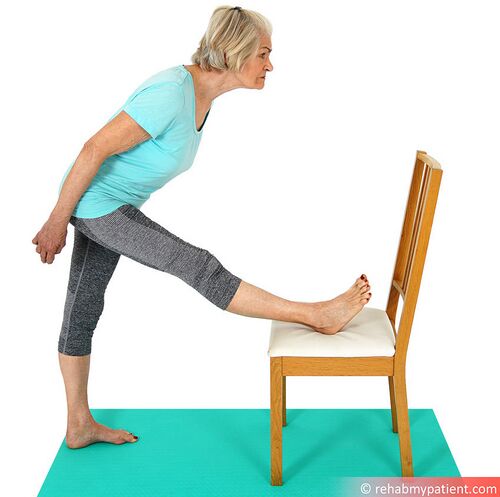
* | * Types of hamstring stretches: (1) standing static stretch, (2) dynamic stretching, (3) hold-relax (also known as contract-relax). | ||
* There is some literature supporting that dynamic stretching is slightly more effective.<ref name=":0" /> In patients with inflexible hamstrings, dynamic hamstring stretching improved muscle activation time and clinical outcomes compared with static hamstring stretching, when both were combined with strengthening exercises.<ref>Lee JH, Jang KM, Kim E, Rhim HC, Kim HD. [https://scholar.google.com/scholar?output=instlink&q=info:DdpWGc-dxd8J:scholar.google.com/&hl=en&as_sdt=0,44&scillfp=2077570342394376331&oi=lle Effects of static and dynamic stretching with strengthening exercises in patients with patellofemoral pain who have inflexible hamstrings: a randomized controlled trial]. Sports health. 2021 Jan;13(1):49-56.</ref> Hold-relax stretching tends to decrease muscle tone which allows the stretch to be deepened. However, it is important to create an exercise programme that is best suited for the patient.<ref name=":0" /> | |||
<div class="row"> | |||
<div class="col-md-6">[[File:Hamstring Stretch on Chair.jpeg|thumb|Standing static stretch|alt=|center|500x500px]]</div> | |||
<div class="col-md-6"> [[File:Hamstring Hold-Relax.jpeg|thumb|Hold-relax (contract-relax) stretch|alt=|center]]</div> | |||
</div> | |||
To learn more about the types of stretches and how stretching effects muscle anatomy and physiology, please read [[Stretching|this article]]. | To learn more about the types of stretches and how stretching effects muscle anatomy and physiology, please read [[Stretching|this article]]. For demonstrations of various methods of hamstring stretching, please view the optional video in the additional resources section at the bottom of this page. | ||
== Quadriceps == | == Quadriceps == | ||
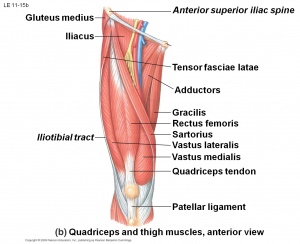
'''Why is it mechanically relevant to assess?''' | [[File:Quadriceps muscle.jpg|thumb|Quadriceps in situ. Please note their relationship with the patella and hip adductors.|alt=]] | ||
'''Why is it mechanically relevant to assess this muscle?''' | |||
* Look for clues in the patient's subjective interview and past medical history. | |||
* If the patient reports knee pain with prolonged sitting (i.e. with the knee flexed), it is important to rule out: (1) quadriceps strength issues, (2) gluteal strength issues, (3) foot posture issues, (4) load issues when considering quadriceps length issues. | |||
* So, when we sit for a prolonged period with tight quadriceps, we have a large compressive vector through our patellofemoral joint. This might be tolerated for a short while, but after a while the pressure in the subchondral bone can keep increasing. Eventually, the individual reaches a point where the only way they can alleviate that pressure pain is to straighten out their leg.<ref name=":0" /> | |||
'''How should we assess and test for muscle length?''' | |||
* Bedside clinical exams: modified [[Thomas Test]]. | |||
** If the patient has some quadriceps tightness, the knee will maintain 45-60 degrees of knee flexion. This signals that the knee is hanging on quadriceps tension. And when they are passively moved to 90 degrees of knee flexion, the examiner can feel the level of resistance in the muscle. | |||
** During this test test, if when the knee is flexed, the hip comes into more flexion, part of the tightness is from [[Rectus Femoris|rectus femoris;]] if the hip does not flex, then there is more tightness in the vastii muscles. | |||
* Cinema Sign (also known as Theatre sign, Movie-goers sign, Movie sign): Pain in the knee results from compression in the patellofemoral joint caused by tight quadriceps with prolonged sitting in knee flexion.<ref name=":0" /> | |||
'''What treatments can we offer?''' | |||
* Stretching of the quadriceps is needed, but may need to be modified based on the patient's level of tightness. | |||
** If the patient is currently experiencing a sore patellofemoral joint, performing a classic standing quadriceps stretch will most likely exacerbate their pain. This stretch can be modified by standing with their foot supported on a chair behind them. The following verbal cues are provided: "stand tall and imagine a helium balloon attached to your breastbone, pulling you up."<ref name=":0" /> | |||
** If the patient's knee is not irritated by this stretch, they can perform a hold-relax (contract-relax) in the same modified position described above. Ask them to push the foot down into the chair and perform an isometric hold for 10 seconds.<ref name=":0" /> | |||
* The patient can also attempt flexibility gains with eccentric exercise. However, patients with patellofemoral pain often will not tolerate exercises that take them eccentrically to end range.<ref name=":0" /> | |||
* There is a small amount of emerging evidence looking at dry needling to trigger points in the vastii muscles as being preferential to sham needling for patellofemoral pain management. A 2020 study by Ma et al.<ref>Ma YT, Li LH, Han Q, Wang XL, Jia PY, Huang QM, Zheng YJ. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7354013/ Effects of trigger point dry needling on neuromuscular performance and pain of individuals affected by patellofemoral pain: a randomized controlled trial]. Journal of Pain Research. 2020;13:1677.</ref> found that dry needling of the quadriceps, when combined with stretching can reduce pain, improve function, and the coordination of the vastus medialis oblique (VMO) and vastus lateralis (VL) in patients with patellofemoral pain syndrome. | |||
* Foam rolling<ref name=":0" /> | |||
<div class="row"> | |||
<div class="col-md-6">[[File:Quadriceps Stretch with Chair.jpeg|none|thumb|Standing modified quadriceps stretch]]</div> | |||
<div class="col-md-6">[[File:Quadriceps Stretch.png|thumb|alt=|center|416x416px|Standing classic quadriceps stretch]]</div> | |||
</div> | |||
'''What | '''What does the literature say?''' | ||
* Bethel et al.<ref name=":1" /> studied the effects of a 7-week stretching programme on healthy adults. They found that completing three sets of a three-stretch programme, three times per week created a significant decrease in the muscle fibre angle in both the VMO and the VL.<ref name=":1">Bethel J, Killingback A, Robertson C, Adds PJ. [https://www.jstage.jst.go.jp/article/jpts/34/2/34_2021-158/_pdf The effect of stretching exercises on the fibre angle of the vastus lateralis and vastus medialis oblique: an ultrasound study.] Journal of Physical Therapy Science. 2022;34(2):161-6.</ref> To learn more about changing the muscle architecture of the quadriceps, please read [[Effective Quadriceps Training in Patellofemoral Pain#Quadriceps and patellar control|this article]]. | |||
* Torrente et al.<ref name=":2" /> looked at the effects of self myofascial release using a foam roller on hypertrophy of the quadriceps. The study found that a 7-week programme of self myofascial release resulted in a statistically significant decrease in the pennation angles of both the VMO and VL in healthy adult males.<ref name=":2">Torrente QM, Killingback A, Robertson C, Adds PJ. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9159710/ The effect of self-myofascial release on the pennation angle of the vastus medialis oblique and the vastus lateralis in athletic male individuals: an ultrasound investigation]. International Journal of Sports Physical Therapy. 2022;17(4):636.</ref> | |||
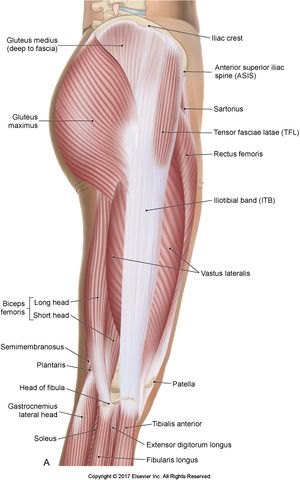
== Iliotibial Band == | |||
'''Why is it mechanically relevant to assess this structure?''' | |||
The iliotibial band (ITB) can be a controversial anatomical structure. It is very strong and thick, and it is not capable of changing length.<ref name=":0" /> <blockquote>"Gratz investigated the tensile properties of human TFL muscle and found similarities with those of “soft steel”, based on its tendon-like histologic structure comprised of an inconspicuous number of elastic fibres."<ref>Seeber GH, Wilhelm MP, Sizer Jr PS, Guthikonda A, Matthijs A, Matthijs OC, Lazovic D, Brismée JM, Gilbert KK. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7296993/ The tensile behaviours OF the iliotibial band–a cadaveric investigation]. International journal of sports physical therapy. 2020 May;15(3):451.</ref></blockquote> | |||
[[File:Iliotibial tract.jpg|thumb|The Iliotibial band in situ. Please note the relationship between the tensor fascia lata and the gluteus maximus.]] | |||
The origins of the ITB are contractile: the [[Tensor Fascia Lata|tensor fascia lata]] (TFL) and the [[Gluteus Maximus|gluteus maximus]]. If there is muscle tension or hypertrophy causing a shortening of the soft tissue structures, then it is going to proximate the ITB. This can cause two issues which can irritate the patellofemoral joint: (1) it can cause a lateral tilt of the patella and (2) through its tibial attachment beyond about 60 degrees of knee flexion, it can externally rotate the tibia. This ultimately will create a functional knee valgus moment, a large [[Q Angle|Q-angle]], which can overload the lateral patellofemoral joint.<ref name=":0" /> | |||
* The patient may reveal that, in addition to their patellofemoral pain, they have some pain at the side of their pelvis when walking. This may indicate that they have a tight and overactive TFL as well. | |||
* They may have a positive cinema sign, but it is more enhanced when their legs are crossed.<ref name=":0" /> | |||
'''How should we assess and test for muscle length?''' | |||
''' | |||
* Bedside clinical exams: [[Ober's Test|Obers test]] (however this can be a challenging position for patients to maintain and for the clinician to fully assess all needed angles).<ref name=":0" /> | |||
''' | '''What does the literature say?''' Kwan et al.<ref name=":3" /> looked at the relationship between hip adduction and patellar position as an alternative to the Obers test. Excessive hip adduction can lead to knee valgus and increased Q-angle which predisposes the patient to patellar displacement. This phenomenon is caused by the tightening of the ITB during hip adduction which places stress on the lateral retinaculum, and leads to lateral patellar movement. This study found that hip adduction consistently produced a smaller patella-condyle distance than the neutral position. This indicates a lateral patellar displacement which could increase the relative load on the lateral patellofemoral joint and cause pain. This study also demonstrated that ultrasound was a reliable assessment tool for patella displacement.<ref name=":3">Kwan LY, Killingback A, Robertson C, Adds P. [https://www.jstage.jst.go.jp/article/jpts/33/7/33_2020-222/_pdf Ultrasound investigation into the relationship between hip adduction and the patellofemoral joint]. Journal of Physical Therapy Science. 2021;33(7):511-6.</ref> | ||
''To perform this test'': with the patient in supine and legs in neutral, assess the initial tilt of the patella. Move the leg to be tested into hip adduction and reassess the tilt of the patella.<ref name=":0" /> | |||
* If the patellar tilt is driven purely by the retinaculum, it will not change much with hip adduction | |||
* If the tilt is from the lateral structures also crossing the hip, then it will change dramatically with hip adduction<ref name=":0" /> | |||
'''What treatments can we offer?''' | |||
* Manual therapy for myofascial release of the contractile tissues of the ITB. | |||
* Instrument-assisted soft tissue release using a spiky massage ball, particularly on TFL. | |||
* Leaning against the wall to provide pressure over the contractile tissues of the ITB. | |||
* Trialing a variety of stretches which impact the contractile tissues and assess which give the best relief. The most effective can be added to the patient's home exercise programme.<ref name=":0" /> | |||
[[File:ITB Stretch.jpeg|thumb|alt=|center|400x400px|Standing TFL stretch]] | |||
== Gastrocnemius and Soleus == | == Gastrocnemius and Soleus == | ||
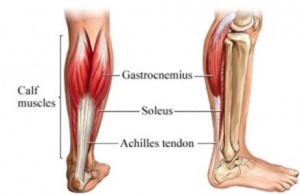
'''Why is it mechanically relevant to assess?''' | [[File:Anatomy of the calf muscles.jpg|thumb|Gastrocnemius and soleus in situ. Please note their relationship with the knee.]] | ||
'''Why is it mechanically relevant to assess these muscles?''' | |||
* During the gait cycle, heel strike occurs at initial contact, then the tibia must translate over the foot in midstance. Tightness in the calf muscles can prevent this from happening. To compensate patients with tight calf muscles will: (1) move into excessive pronation or (2) have an early heel rise in the gait cycle. Both of these compensations have negative effects on the patellofemoral joint causing tibial rotation and patellofemoral pain, and increasing patellofemoral contact pressure respectively.<ref name=":0" /> | |||
* A study performed in 2015 showed that people with osteoarthritic patellofemoral joints have more bone oedema in their patellofemoral joint if they have increased knee flexion at the end of their gait cycle.<ref>Teng HL, MacLeod TD, Link TM, Majumdar S, Souza RB. [https://www.jospt.org/doi/pdf/10.2519/jospt.2015.5859?download=true Higher knee flexion moment during the second half of the stance phase of gait is associated with the progression of osteoarthritis of the patellofemoral joint on magnetic resonance imaging]. journal of orthopaedic & sports physical therapy. 2015 Sep;45(9):656-64.</ref> This can be caused in two ways: (1) tight calf muscles or (2) tight hip flexors which limit the ability to get into hip extension. This will make the patient have to flex the knee to offload the hip.<ref name=":0" /> | |||
* The patient may reveal that they stretch often, but that their calf muscles will not stop cramping or are always tight. In these cases, it is important to assess their hip flexor endurance. The patient may be pushing through their calf muscles to compensate for a lack of ability to pull through their hip flexors.<ref name=":0" /> | |||
* | |||
'''How should we assess and test for muscle length?''' | |||
* It is important to distinguish between the [[gastrocnemius]] and [[soleus]]. | |||
* Assess the gastrocnemius with a straight knee, soleus with a flexed knee. Testing can be done in supine for either muscle or the standing [[Knee to Wall Test|knee-to-wall test]] can assess the soleus.<ref name=":0" /> | |||
'''What treatments can we offer?''' | |||
* Manual therapy for myofascial release or instrument-assisted soft tissue release | |||
* Foam rolling | |||
* Dynamic stretching<ref name=":0" /> | |||
<div class="row"> | |||
<div class="col-md-6">[[File:Gastrocnemius Stretching.jpeg|none|thumb|alt=|403x403px]]</div> | |||
<div class="col-md-6">[[File:Gastrocnemius Stretching Against Wall.jpeg|none|thumb|alt=|400x400px]]</div> | |||
</div> | |||
== Resources == | == Resources == | ||
''' | '''Optional Viewing:''' | ||
* | Please view this short video for demonstrations of various types of hamstring stretches. | ||
{{#ev:youtube| oRdXgERlSag |500}}<ref>YouTube. Hamstring Stretches for Tight or Sore Hamstrings - Ask Doctor Jo. Available from: https://www.youtube.com/watch?v=oRdXgERlSag [last accessed 29/08/2022]</ref> | |||
'''Optional Suggested Physiopedia Pages:''' | |||
* [[Patellofemoral Pain Syndrome]] | |||
* [[Patellofemoral Pain Syndrome and Hip Strength]] | |||
'''Additional Optional Reading:''' | '''Additional Optional Reading:''' | ||
* Bethel J, Killingback A, Robertson C, Adds PJ. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8860688/ The effect of stretching exercises on the fibre angle of the vastus lateralis and vastus medialis oblique: an ultrasound study.] Journal of Physical Therapy Science. 2022;34(2):161-6. | |||
* Fredericson M, White JJ, MacMahon JM, Andriacchi TP. [https://www.researchgate.net/profile/Michael-Fredericson/publication/11375416_Quantitative_analysis_of_the_relative_effectiveness_of_3_iliotibial_band_stretches/links/5a25961daca2727dd880e0e5/Quantitative-analysis-of-the-relative-effectiveness-of-3-iliotibial-band-stretches.pdf Quantitative analysis of the relative effectiveness of 3 iliotibial band stretches]. Archives of physical medicine and rehabilitation. 2002 May 1;83(5):589-92. | |||
* Torrente QM, Killingback A, Robertson C, Adds PJ. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9159710/ The effect of self-myofascial release on the pennation angle of the vastus medialis oblique and the vastus lateralis in athletic male individuals: an ultrasound investigation]. International Journal of Sports Physical Therapy. 2022;17(4):636. | |||
== References == | == References == | ||
| Line 101: | Line 162: | ||
<references /> | <references /> | ||
[[Category:Course Pages]] | [[Category:Course Pages]] | ||
[[Category:Plus Content]] | [[Category:Plus Content]] | ||
[[Category:Knee]] | |||
[[Category:Musculoskeletal/Orthopaedics]] | |||
Latest revision as of 14:42, 24 October 2023
Top Contributors - Stacy Schiurring, Jess Bell and Kim Jackson
Introduction[edit | edit source]
Patellofemoral pain often results from cumulative load. It reveals itself with prolonged and or repetitive activity or holding of a certain position. Subtle changes in load can add up over time to create a large load.[1] Thorough assessment and the subjective interview will provide clues to causative factors of the patient's patellofemoral pain.
For a review of the gait cycle, please read this article.
Hamstrings[edit | edit source]
Why is it mechanically relevant to assess this muscle?
- Tight, tense, and shortened hamstrings can pull the knee into excessive knee flexion. During the gait cycle, this can result in a greater knee flexion moment at initial contact or heel strike.
- Any resulting increase in knee flexion will increase patellofemoral contact pressures. Therefore, it is important to avoid the situation where the tibia is being pulled back and there is enhanced knee flexion.[1]
How should we assess and test for muscle length?
- It is important to assess hamstring length in conjunction with stride length
- Bedside clinical exams: sit-and-reach, straight leg raise
- It is important to assess and compare the muscle length of both hamstrings. The rehabilitation professional should also take the patient's relative flexibility into consideration, ie: is this patient's body flexible overall or tight. This will help determine the patient's muscle length norm.
- Other muscle groups to assess: gluteal extensors
- Clues from the patient interview or past medical history: a patient may state that they stretch regularly but have not noticed any change in their flexibility; a history of repeated injury to a muscle group might mean that it has more scarring in the intramuscular matter; having regular repeating injuries.[1]
What treatments can we offer?
- The literature gives little insight into the duration or frequency of stretching.[1]
- Consistent, regular stretching that the patient will be able to complete is key. Find out about the patient's schedule and lifestyle and help them create an exercise programme they will be able to stick to and faithfully perform. Create easy, pragmatic exercises the patient will most likely complete.[1]
- Types of hamstring stretches: (1) standing static stretch, (2) dynamic stretching, (3) hold-relax (also known as contract-relax).
- There is some literature supporting that dynamic stretching is slightly more effective.[1] In patients with inflexible hamstrings, dynamic hamstring stretching improved muscle activation time and clinical outcomes compared with static hamstring stretching, when both were combined with strengthening exercises.[2] Hold-relax stretching tends to decrease muscle tone which allows the stretch to be deepened. However, it is important to create an exercise programme that is best suited for the patient.[1]
To learn more about the types of stretches and how stretching effects muscle anatomy and physiology, please read this article. For demonstrations of various methods of hamstring stretching, please view the optional video in the additional resources section at the bottom of this page.
Quadriceps[edit | edit source]
Why is it mechanically relevant to assess this muscle?
- Look for clues in the patient's subjective interview and past medical history.
- If the patient reports knee pain with prolonged sitting (i.e. with the knee flexed), it is important to rule out: (1) quadriceps strength issues, (2) gluteal strength issues, (3) foot posture issues, (4) load issues when considering quadriceps length issues.
- So, when we sit for a prolonged period with tight quadriceps, we have a large compressive vector through our patellofemoral joint. This might be tolerated for a short while, but after a while the pressure in the subchondral bone can keep increasing. Eventually, the individual reaches a point where the only way they can alleviate that pressure pain is to straighten out their leg.[1]
How should we assess and test for muscle length?
- Bedside clinical exams: modified Thomas Test.
- If the patient has some quadriceps tightness, the knee will maintain 45-60 degrees of knee flexion. This signals that the knee is hanging on quadriceps tension. And when they are passively moved to 90 degrees of knee flexion, the examiner can feel the level of resistance in the muscle.
- During this test test, if when the knee is flexed, the hip comes into more flexion, part of the tightness is from rectus femoris; if the hip does not flex, then there is more tightness in the vastii muscles.
- Cinema Sign (also known as Theatre sign, Movie-goers sign, Movie sign): Pain in the knee results from compression in the patellofemoral joint caused by tight quadriceps with prolonged sitting in knee flexion.[1]
What treatments can we offer?
- Stretching of the quadriceps is needed, but may need to be modified based on the patient's level of tightness.
- If the patient is currently experiencing a sore patellofemoral joint, performing a classic standing quadriceps stretch will most likely exacerbate their pain. This stretch can be modified by standing with their foot supported on a chair behind them. The following verbal cues are provided: "stand tall and imagine a helium balloon attached to your breastbone, pulling you up."[1]
- If the patient's knee is not irritated by this stretch, they can perform a hold-relax (contract-relax) in the same modified position described above. Ask them to push the foot down into the chair and perform an isometric hold for 10 seconds.[1]
- The patient can also attempt flexibility gains with eccentric exercise. However, patients with patellofemoral pain often will not tolerate exercises that take them eccentrically to end range.[1]
- There is a small amount of emerging evidence looking at dry needling to trigger points in the vastii muscles as being preferential to sham needling for patellofemoral pain management. A 2020 study by Ma et al.[3] found that dry needling of the quadriceps, when combined with stretching can reduce pain, improve function, and the coordination of the vastus medialis oblique (VMO) and vastus lateralis (VL) in patients with patellofemoral pain syndrome.
- Foam rolling[1]
What does the literature say?
- Bethel et al.[4] studied the effects of a 7-week stretching programme on healthy adults. They found that completing three sets of a three-stretch programme, three times per week created a significant decrease in the muscle fibre angle in both the VMO and the VL.[4] To learn more about changing the muscle architecture of the quadriceps, please read this article.
- Torrente et al.[5] looked at the effects of self myofascial release using a foam roller on hypertrophy of the quadriceps. The study found that a 7-week programme of self myofascial release resulted in a statistically significant decrease in the pennation angles of both the VMO and VL in healthy adult males.[5]
Iliotibial Band[edit | edit source]
Why is it mechanically relevant to assess this structure?
The iliotibial band (ITB) can be a controversial anatomical structure. It is very strong and thick, and it is not capable of changing length.[1]
"Gratz investigated the tensile properties of human TFL muscle and found similarities with those of “soft steel”, based on its tendon-like histologic structure comprised of an inconspicuous number of elastic fibres."[6]
The origins of the ITB are contractile: the tensor fascia lata (TFL) and the gluteus maximus. If there is muscle tension or hypertrophy causing a shortening of the soft tissue structures, then it is going to proximate the ITB. This can cause two issues which can irritate the patellofemoral joint: (1) it can cause a lateral tilt of the patella and (2) through its tibial attachment beyond about 60 degrees of knee flexion, it can externally rotate the tibia. This ultimately will create a functional knee valgus moment, a large Q-angle, which can overload the lateral patellofemoral joint.[1]
- The patient may reveal that, in addition to their patellofemoral pain, they have some pain at the side of their pelvis when walking. This may indicate that they have a tight and overactive TFL as well.
- They may have a positive cinema sign, but it is more enhanced when their legs are crossed.[1]
How should we assess and test for muscle length?
- Bedside clinical exams: Obers test (however this can be a challenging position for patients to maintain and for the clinician to fully assess all needed angles).[1]
What does the literature say? Kwan et al.[7] looked at the relationship between hip adduction and patellar position as an alternative to the Obers test. Excessive hip adduction can lead to knee valgus and increased Q-angle which predisposes the patient to patellar displacement. This phenomenon is caused by the tightening of the ITB during hip adduction which places stress on the lateral retinaculum, and leads to lateral patellar movement. This study found that hip adduction consistently produced a smaller patella-condyle distance than the neutral position. This indicates a lateral patellar displacement which could increase the relative load on the lateral patellofemoral joint and cause pain. This study also demonstrated that ultrasound was a reliable assessment tool for patella displacement.[7]
To perform this test: with the patient in supine and legs in neutral, assess the initial tilt of the patella. Move the leg to be tested into hip adduction and reassess the tilt of the patella.[1]
- If the patellar tilt is driven purely by the retinaculum, it will not change much with hip adduction
- If the tilt is from the lateral structures also crossing the hip, then it will change dramatically with hip adduction[1]
What treatments can we offer?
- Manual therapy for myofascial release of the contractile tissues of the ITB.
- Instrument-assisted soft tissue release using a spiky massage ball, particularly on TFL.
- Leaning against the wall to provide pressure over the contractile tissues of the ITB.
- Trialing a variety of stretches which impact the contractile tissues and assess which give the best relief. The most effective can be added to the patient's home exercise programme.[1]
Gastrocnemius and Soleus[edit | edit source]
Why is it mechanically relevant to assess these muscles?
- During the gait cycle, heel strike occurs at initial contact, then the tibia must translate over the foot in midstance. Tightness in the calf muscles can prevent this from happening. To compensate patients with tight calf muscles will: (1) move into excessive pronation or (2) have an early heel rise in the gait cycle. Both of these compensations have negative effects on the patellofemoral joint causing tibial rotation and patellofemoral pain, and increasing patellofemoral contact pressure respectively.[1]
- A study performed in 2015 showed that people with osteoarthritic patellofemoral joints have more bone oedema in their patellofemoral joint if they have increased knee flexion at the end of their gait cycle.[8] This can be caused in two ways: (1) tight calf muscles or (2) tight hip flexors which limit the ability to get into hip extension. This will make the patient have to flex the knee to offload the hip.[1]
- The patient may reveal that they stretch often, but that their calf muscles will not stop cramping or are always tight. In these cases, it is important to assess their hip flexor endurance. The patient may be pushing through their calf muscles to compensate for a lack of ability to pull through their hip flexors.[1]
How should we assess and test for muscle length?
- It is important to distinguish between the gastrocnemius and soleus.
- Assess the gastrocnemius with a straight knee, soleus with a flexed knee. Testing can be done in supine for either muscle or the standing knee-to-wall test can assess the soleus.[1]
What treatments can we offer?
- Manual therapy for myofascial release or instrument-assisted soft tissue release
- Foam rolling
- Dynamic stretching[1]
Resources[edit | edit source]
Optional Viewing:
Please view this short video for demonstrations of various types of hamstring stretches.
Optional Suggested Physiopedia Pages:
Additional Optional Reading:
- Bethel J, Killingback A, Robertson C, Adds PJ. The effect of stretching exercises on the fibre angle of the vastus lateralis and vastus medialis oblique: an ultrasound study. Journal of Physical Therapy Science. 2022;34(2):161-6.
- Fredericson M, White JJ, MacMahon JM, Andriacchi TP. Quantitative analysis of the relative effectiveness of 3 iliotibial band stretches. Archives of physical medicine and rehabilitation. 2002 May 1;83(5):589-92.
- Torrente QM, Killingback A, Robertson C, Adds PJ. The effect of self-myofascial release on the pennation angle of the vastus medialis oblique and the vastus lateralis in athletic male individuals: an ultrasound investigation. International Journal of Sports Physical Therapy. 2022;17(4):636.
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 1.22 1.23 1.24 Robertson, C. Patellofemoral Joint Programme. Muscle Length Assessment and Treatment Related to Patellofemoral Pain. Physioplus. 2022.
- ↑ Lee JH, Jang KM, Kim E, Rhim HC, Kim HD. Effects of static and dynamic stretching with strengthening exercises in patients with patellofemoral pain who have inflexible hamstrings: a randomized controlled trial. Sports health. 2021 Jan;13(1):49-56.
- ↑ Ma YT, Li LH, Han Q, Wang XL, Jia PY, Huang QM, Zheng YJ. Effects of trigger point dry needling on neuromuscular performance and pain of individuals affected by patellofemoral pain: a randomized controlled trial. Journal of Pain Research. 2020;13:1677.
- ↑ 4.0 4.1 Bethel J, Killingback A, Robertson C, Adds PJ. The effect of stretching exercises on the fibre angle of the vastus lateralis and vastus medialis oblique: an ultrasound study. Journal of Physical Therapy Science. 2022;34(2):161-6.
- ↑ 5.0 5.1 Torrente QM, Killingback A, Robertson C, Adds PJ. The effect of self-myofascial release on the pennation angle of the vastus medialis oblique and the vastus lateralis in athletic male individuals: an ultrasound investigation. International Journal of Sports Physical Therapy. 2022;17(4):636.
- ↑ Seeber GH, Wilhelm MP, Sizer Jr PS, Guthikonda A, Matthijs A, Matthijs OC, Lazovic D, Brismée JM, Gilbert KK. The tensile behaviours OF the iliotibial band–a cadaveric investigation. International journal of sports physical therapy. 2020 May;15(3):451.
- ↑ 7.0 7.1 Kwan LY, Killingback A, Robertson C, Adds P. Ultrasound investigation into the relationship between hip adduction and the patellofemoral joint. Journal of Physical Therapy Science. 2021;33(7):511-6.
- ↑ Teng HL, MacLeod TD, Link TM, Majumdar S, Souza RB. Higher knee flexion moment during the second half of the stance phase of gait is associated with the progression of osteoarthritis of the patellofemoral joint on magnetic resonance imaging. journal of orthopaedic & sports physical therapy. 2015 Sep;45(9):656-64.
- ↑ YouTube. Hamstring Stretches for Tight or Sore Hamstrings - Ask Doctor Jo. Available from: https://www.youtube.com/watch?v=oRdXgERlSag [last accessed 29/08/2022]