Assessment of Plantar Heel Pain - A Literature Review: Difference between revisions
No edit summary |
No edit summary |
||
| (16 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor '''- [[User: | '''Original Editor '''- [[User:Merinda Rodseth|Merinda Rodseth]] based on the course by | ||
[https://members.physio-pedia.com/course_tutor/bernice-saban/ Bernice Saban]<br> | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
The diagnosis of plantar heel pain syndrome (PHPS) is predominantly based on the symptoms of the patient together with manual palpation of the painful heel <ref name=":1">Saban B, Masharawi Y. [https://www.sciencedirect.com/science/article/abs/pii/S0031940616300323 Three single leg standing tests for clinical assessment of chronic plantar heel pain syndrome: static stance, half-squat and heel rise]. Physiotherapy. 2017 Jun 1;103(2):237-44. </ref><ref name=":2">Draghi F, Gitto S, Bortolotto C, Draghi AG, Belometti GO. [https://insightsimaging.springeropen.com/track/pdf/10.1007/s13244-016-0533-2.pdf Imaging of plantar fascia disorders: findings on plain radiography, ultrasound and magnetic resonance imaging]. Insights into imaging. 2017 Feb;8(1):69-78. </ref> | The diagnosis of [[Introduction to Plantar Heel Pain|plantar heel pain syndrome]] (PHPS) is predominantly based on the symptoms of the patient together with manual palpation of the painful heel.<ref name=":1">Saban B, Masharawi Y. [https://www.sciencedirect.com/science/article/abs/pii/S0031940616300323 Three single leg standing tests for clinical assessment of chronic plantar heel pain syndrome: static stance, half-squat and heel rise]. Physiotherapy. 2017 Jun 1;103(2):237-44. </ref><ref name=":2">Draghi F, Gitto S, Bortolotto C, Draghi AG, Belometti GO. [https://insightsimaging.springeropen.com/track/pdf/10.1007/s13244-016-0533-2.pdf Imaging of plantar fascia disorders: findings on plain radiography, ultrasound and magnetic resonance imaging]. Insights into imaging. 2017 Feb;8(1):69-78. </ref> Validation of this diagnosis through the use of a reliable clinical test is, however, still elusive. This is significant as valid assessment tools are necessary to ensure optimal management. These tools not only ensure health professionals can assess the status of the patient, but they also highlight the efficacy of treatment and guide which treatment methods to use. | ||
This article will provide an analysis of the available literature on the assessment of PHPS. | |||
== Assessment Tools for PHPS == | == Assessment Tools for PHPS == | ||
A variety of tests have been proposed for the assessment and diagnosis of PHPS but none have been accepted as the “gold standard”<ref name=":1" /> | A variety of tests have been proposed for the assessment and diagnosis of PHPS, but none have been accepted as the “gold standard”.<ref name=":1" /> This necessitates an analysis of the available research to identify which of the proposed tests are reliable and valid for assessing PHPS (Figure 1). | ||
[[File:Assessment tools for PHP.jpg|frameless|450x450px]] | [[File:Assessment tools for PHP.jpg|frameless|450x450px]] | ||
'''Figure 1'''. Assessment tools for PHPS <ref name=":0">Bernice Saban 2021. Assessment of Plantar Heel Pain - A Literature Review. | '''Figure 1'''. Assessment tools for PHPS <ref name=":0">Bernice Saban 2021. Assessment of Plantar Heel Pain - A Literature Review. Plus Course. 2021</ref> | ||
==== Windlass Test ==== | ==== Windlass Test ==== | ||
The “windlass mechanism” describes the way in which the plantar fascia supports the foot during weight-bearing activities while providing information about the biomechanical stresses placed on the plantar fascia<ref name=":3">Bolgla LA, Malone TR. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC385265/pdf/attr_39_01_0077.pdf Plantar fasciitis and the windlass mechanism: a biomechanical link to clinical practice]. Journal of athletic training. 2004 Jan;39(1):77. </ref> | The “windlass mechanism” describes the way in which the [[Plantar Aponeurosis|plantar fascia]] supports the foot during weight-bearing activities while providing information about the biomechanical stresses placed on the plantar fascia.<ref name=":3">Bolgla LA, Malone TR. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC385265/pdf/attr_39_01_0077.pdf Plantar fasciitis and the windlass mechanism: a biomechanical link to clinical practice]. Journal of athletic training. 2004 Jan;39(1):77. </ref> Hicks<ref>Hicks JH. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1244640/pdf/janat00463-0036.pdf The mechanics of the foot: II. The plantar aponeurosis and the arch]. Journal of anatomy. 1954 Jan;88(Pt 1):25. </ref> originally described the foot and its ligaments as an “arch-like triangular structure” with the plantar fascia forming the base/tie-rod that runs from the calcaneus to the phalanges.<ref name=":3" /> In the propulsive phase of gait, the plantar fascia is wound around the head of the first metatarsal during ankle and hallux dorsiflexion. This shortens the distance between the calcaneus and the metatarsals. The shortening of the plantar fascia that results from dorsiflexion of the big toe simulates the “windlass” (tightening rope/cable) mechanism.<ref name=":3" /> | ||
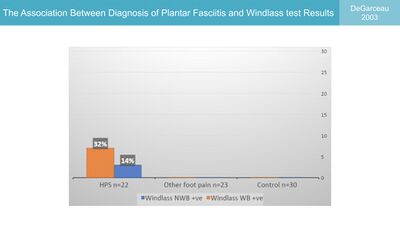
The Windlass Test, therefore, induces strain on the plantar fascia through forced dorsiflexion of the great toe | The [[Windlass Test]], therefore, induces strain on the plantar fascia through forced dorsiflexion of the great toe. This strain is associated with increased pain at the site of the insertion of the plantar fascia in patients with plantar fasciitis.<ref name=":4">De Garceau D, Dean D, Requejo SM, Thordarson DB. [https://journals.sagepub.com/doi/10.1177/107110070302400309 The association between diagnosis of plantar fasciitis and Windlass test results]. Foot & ankle international. 2003 Mar;24(3):251-5. </ref> However, when De Garceau et al. <ref name=":4" /> studied the association between the diagnosis of plantar fasciitis and the results of the windlass test, they found that even though the test is specific for PHPS, it has a low rate of sensitivity which limits its value in clinical evaluation (Figure 2). | ||
[[File:Plantar fasciitis and Windlass test.jpg|frameless|400x400px]] | [[File:Plantar fasciitis and Windlass test.jpg|frameless|400x400px]] | ||
'''Figure 2'''. The association between the diagnosis of plantar fasciitis and the | '''Figure 2'''. The association between the diagnosis of plantar fasciitis and the windlass test results <ref name=":0" /><ref name=":4" /> | ||
The strain induced with first metatarsal extension was also not limited to the plantar fascia alone, but included various structures in the foot, including the tibial nerve and the medial plantar nerve <ref>Alshami AM, Babri AS, Souvlis T, Coppieters MW. [https://d1wqtxts1xzle7.cloudfront.net/47367905/Alshami_et_al_2007.pdf?1468987571=&response-content-disposition=inline%3B+filename%3DFOOT_and_ANKLE_INTERNATIONAL_Biomechanic.pdf&Expires=1626888706&Signature=XKaY7uBwngnCGoiaySU9lc1zW12PM3b6dBK2rvwh~SVvVxLjKcg4Lmd1AmhOr4pOVH0ywxSvFvrqr45kixqx7hpBdVA79vxYU~6TAU9B7Pv0ToPmo0q-Nl2cMNisaWUggHRQjJJ8bSSMboPT-5qDZvVmM0f4K7MxmB~T2eJkDH4Pme6V0Q0ucRu~RmtX9JpJUbitLdk4okKJ4ijCq-qOKsJ-ouZZolUNBkIJJVnDvfUnDCO2dy1xnhF6m9LZkc4-OUtAoD1Jz1psTYtYlWwBZv~y0e4IO-iGDjhdRytHe831FbM-X0YPoQoZFqFr71dc6w~VeVSWllF64gK84niBKQ__&Key-Pair-Id=APKAJLOHF5GGSLRBV4ZA Biomechanical evaluation of two clinical tests for plantar heel pain: the dorsiflexion-eversion test for tarsal tunnel syndrome and the windlass test for plantar fasciitis]. Foot & ankle international. 2007 Apr;28(4):499-505. </ref> | The strain induced with first metatarsal extension was also not limited to the plantar fascia alone, but included various structures in the foot, including the tibial nerve and the medial plantar nerve.<ref>Alshami AM, Babri AS, Souvlis T, Coppieters MW. [https://d1wqtxts1xzle7.cloudfront.net/47367905/Alshami_et_al_2007.pdf?1468987571=&response-content-disposition=inline%3B+filename%3DFOOT_and_ANKLE_INTERNATIONAL_Biomechanic.pdf&Expires=1626888706&Signature=XKaY7uBwngnCGoiaySU9lc1zW12PM3b6dBK2rvwh~SVvVxLjKcg4Lmd1AmhOr4pOVH0ywxSvFvrqr45kixqx7hpBdVA79vxYU~6TAU9B7Pv0ToPmo0q-Nl2cMNisaWUggHRQjJJ8bSSMboPT-5qDZvVmM0f4K7MxmB~T2eJkDH4Pme6V0Q0ucRu~RmtX9JpJUbitLdk4okKJ4ijCq-qOKsJ-ouZZolUNBkIJJVnDvfUnDCO2dy1xnhF6m9LZkc4-OUtAoD1Jz1psTYtYlWwBZv~y0e4IO-iGDjhdRytHe831FbM-X0YPoQoZFqFr71dc6w~VeVSWllF64gK84niBKQ__&Key-Pair-Id=APKAJLOHF5GGSLRBV4ZA Biomechanical evaluation of two clinical tests for plantar heel pain: the dorsiflexion-eversion test for tarsal tunnel syndrome and the windlass test for plantar fasciitis]. Foot & ankle international. 2007 Apr;28(4):499-505. </ref> | ||
[[File:Windlass and assessment PHPS2.jpg|frameless|700x700px]] | [[File:Windlass and assessment PHPS2.jpg|frameless|700x700px]] | ||
==== Palpation of the Painful Heel Area ==== | ==== Palpation of the Painful Heel Area ==== | ||
Manual palpation of the heel by thumb pressure is a common tool used by clinicians to locate the exact site of pain | Manual palpation of the heel by thumb pressure is a common tool used by clinicians to locate the exact site of pain. It has been proposed that this can aid with both diagnosis and the prescription of treatment in patients with PHPS.<ref name=":0" /><ref name=":5" /><ref name=":6">Martin RL, Davenport TE, Reischl SF, McPoil TG, Matheson JW, Wukich DK, McDonough CM, Altman RD, Beattie P, Cornwall M, Davis I. [https://www.jospt.org/doi/pdfplus/10.2519/jospt.2014.0303?download=true Heel pain—plantar fasciitis: revision 2014]. Journal of Orthopaedic & Sports Physical Therapy. 2014 Nov;44(11):A1-33. </ref><ref>Drake C, Mallows A, Littlewood C. [https://onlinelibrary.wiley.com/doi/pdfdirect/10.1002/msc.1246 Psychosocial variables and presence, severity and prognosis of plantar heel pain: A systematic review of cross‐sectional and prognostic associations]. Musculoskeletal Care. 2018 Sep;16(3):329-38. DOI:10.1002/msc.1246 | ||
</ref> | </ref> No study has, however, quantified the mechanical pressure needed to elicit pain in patients with PHPS and no clinical trials exist to support it as a valid assessment tool for PHPS.<ref name=":0" /><ref name=":5" /> | ||
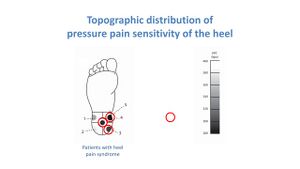
[[File:Topographic distribution of pressure pain sensitivity Saban 2016.jpg|thumb|'''Figure 3'''. Topographic distribution of pressure pain sensitivity of the heel <ref name=":0" /> <ref name=":5">Saban B, Masharawi Y. [https://sci-hub.se/10.1177/1071100716642038 Pain threshold tests in patients with heel pain syndrome]. Foot & ankle international. 2016 Jul;37(7):730-6. </ref>]] | [[File:Topographic distribution of pressure pain sensitivity Saban 2016.jpg|thumb|'''Figure 3'''. Topographic distribution of pressure pain sensitivity of the heel <ref name=":0" /> <ref name=":5">Saban B, Masharawi Y. [https://sci-hub.se/10.1177/1071100716642038 Pain threshold tests in patients with heel pain syndrome]. Foot & ankle international. 2016 Jul;37(7):730-6. </ref>]] | ||
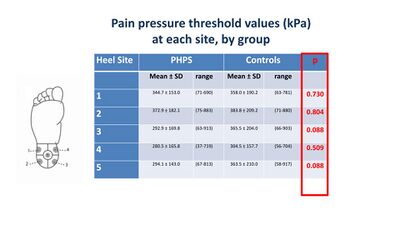
Saban | Saban and Masharawi<ref name=":5" /> used pain pressure threshold (PPT) to assess the area and extent of pain sensitivity in individuals with and without heel pain (Figure 3). They identified the anterior medial heel as the most sensitive location in the heel, but no significant differences were found between those with and without heel pain (Figure 4). This means the test is not sensitive enough for PHPS and is, therefore, not a diagnostic tool for heel pain. <ref name=":5" /> | ||
[[File:PPT for heel pain Saban 2016.jpg|none|thumb|400x400px|'''Figure 4'''. Pressure pain threshold values <ref name=":0" /><ref name=":5" /> ]] | [[File:PPT for heel pain Saban 2016.jpg|none|thumb|400x400px|'''Figure 4'''. Pressure pain threshold values <ref name=":0" /><ref name=":5" /> ]] | ||
| Line 39: | Line 42: | ||
==== Imaging ==== | ==== Imaging ==== | ||
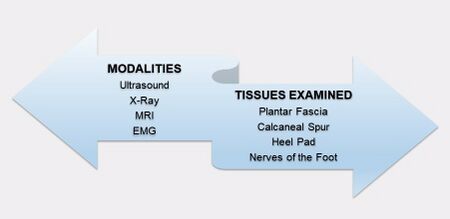
Imaging is generally useful for acquiring accurate diagnoses, prompting appropriate treatment and determining prognosis <ref name=":2" /> | Imaging is generally useful for acquiring accurate diagnoses, prompting appropriate treatment and determining prognosis.<ref name=":2" /> Various imaging methods, including conventional [[X-Rays|radiograph]], [[Ultrasound Scans|ultrasound]] and [[MRI Scans|magnetic resonance imaging]] (MRI), have been used to assess various structures implicated in [[Plantar Heel Pain|plantar heel pain]] (Figure 5).<ref name=":1" /><ref name=":2" /><ref name=":0" /><ref>Allam AE, Chang KV. [https://www.ncbi.nlm.nih.gov/books/NBK499868/ Plantar Heel Pain]. StatPearls [Internet]. 2021 Feb 5. </ref><ref name=":7">Riel H, Cotchett M, Delahunt E, Rathleff MS, Vicenzino B, Weir A, Landorf KB. [https://sci-hub.se/https://bjsm.bmj.com/content/51/22/1576 Is ‘plantar heel pain’a more appropriate term than ‘plantar fasciitis’? Time to move on]. Br J Sports Med.2017 Nov;51(22):1576-1577. </ref><ref>Drake C, Whittaker GA, Kaminski MR, Chen J, Keenan AM, Rathleff MS, et al. [https://jfootankleres.biomedcentral.com/articles/10.1186/s13047-021-00507-2 Medical imaging for plantar heel pain: a systematic review and meta-analysis]. J Foot Ankle Res. 2022 Jan 22;15(1):4.</ref> | ||
[[File:Imaging PHPS2.jpg|frameless|450x450px]] | [[File:Imaging PHPS2.jpg|frameless|450x450px]] | ||
| Line 47: | Line 50: | ||
'''<u>Imaging of the plantar fascia</u>''' | '''<u>Imaging of the plantar fascia</u>''' | ||
Individuals with PHPS were found to be 105 times more likely to present with a thickened plantar fascia measuring more than 4.0 mm compared to those without making it a reliable sign of PHPS <ref name=":2" /><ref name=":7" /> | Individuals with PHPS were found to be 105 times more likely to present with a thickened plantar fascia measuring more than 4.0 mm compared to those without making it a reliable sign of PHPS.<ref name=":2" /><ref name=":7" /> | ||
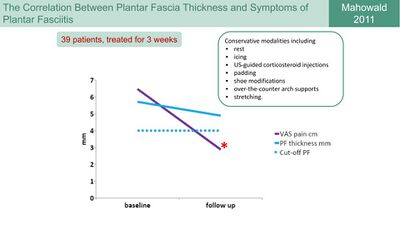
Following this, Mahowald et al <ref name=":8">Mahowald S, Legge BS, Grady JF. [https://pubmed.ncbi.nlm.nih.gov/21957269/ The correlation between plantar fascia thickness and symptoms of plantar fasciitis]. Journal of the American Podiatric Medical Association. 2011 Sep;101(5):385-9. </ref> investigated the correlation between plantar fascia thickness and symptoms of plantar fasciitis as a way to gauge the efficacy of treatment modalities | Following this, Mahowald et al. <ref name=":8">Mahowald S, Legge BS, Grady JF. [https://pubmed.ncbi.nlm.nih.gov/21957269/ The correlation between plantar fascia thickness and symptoms of plantar fasciitis]. Journal of the American Podiatric Medical Association. 2011 Sep;101(5):385-9. </ref> investigated the correlation between plantar fascia thickness and symptoms of [[Plantar Fasciitis|plantar fasciitis]] as a way to gauge the efficacy of treatment modalities. They found that a reduction in pain correlated strongly with a reduction in plantar fascia thickness. The thickness of the plantar fascia, however, remained above 4 mm, which would still be indicative of PHPS (Figure 6).<ref name=":0" /><ref name=":8" /> | ||
[[File:Plantar fasia thickness and symptoms Mahowald 2011.jpg|none|thumb|400x400px|'''Figure 6'''. Correlation between Plantar Facia Thickness and Symptoms of Plantar Fasciitis <ref name=":0" /><ref name=":8" /> ]] | [[File:Plantar fasia thickness and symptoms Mahowald 2011.jpg|none|thumb|400x400px|'''Figure 6'''. Correlation between Plantar Facia Thickness and Symptoms of Plantar Fasciitis <ref name=":0" /><ref name=":8" /> ]] | ||
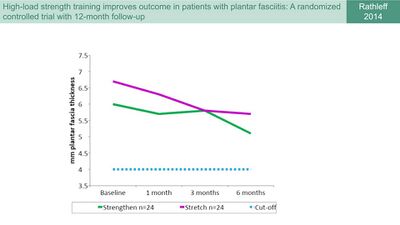
Rathleff et al <ref name=":9">Rathleff MS, Mølgaard CM, Fredberg U, Kaalund S, Andersen KB, Jensen TT, Aaskov S, Olesen JL. [https://sci-hub.se/10.1111/sms.12313 High‐load strength training improves outcome in patients with plantar fasciitis: A randomized controlled trial with 12‐month follow‐up]. Scandinavian journal of medicine & science in sports. 2015 Jun;25(3):e292-300. </ref> used thickness of the plantar fascia as an outcome measure to assess the efficacy of shoe inserts and plantar fascia specific stretching vs shoe inserts and high-load strength training in patients with plantar fasciitis. They also reported a reduction in plantar fascia thickness in both groups but similarly the plantar fascia thickness remained more than 4 mm (Figure 7) <ref name=":0" /><ref name=":9" /> | |||
Rathleff et al. <ref name=":9">Rathleff MS, Mølgaard CM, Fredberg U, Kaalund S, Andersen KB, Jensen TT, Aaskov S, Olesen JL. [https://sci-hub.se/10.1111/sms.12313 High‐load strength training improves outcome in patients with plantar fasciitis: A randomized controlled trial with 12‐month follow‐up]. Scandinavian journal of medicine & science in sports. 2015 Jun;25(3):e292-300. </ref> used thickness of the plantar fascia as an outcome measure to assess the efficacy of shoe inserts and plantar fascia specific stretching vs shoe inserts and high-load strength training in patients with plantar fasciitis. They also reported a reduction in plantar fascia thickness in both groups, but similarly the plantar fascia thickness remained more than 4 mm (Figure 7).<ref name=":0" /><ref name=":9" /> | |||
[[File:Rathleff plantar fascia thickness.jpg|none|thumb|400x400px|'''Figure 7'''. Changes in Plantar Fascia Thickness with a stretch and strengthening program <ref name=":0" /><ref name=":9" />]] | [[File:Rathleff plantar fascia thickness.jpg|none|thumb|400x400px|'''Figure 7'''. Changes in Plantar Fascia Thickness with a stretch and strengthening program <ref name=":0" /><ref name=":9" />]] | ||
| Line 59: | Line 63: | ||
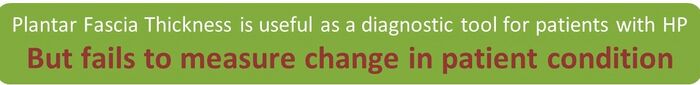
[[File:Plantar fascia thickness asessement2.jpg|frameless|700x700px]] | [[File:Plantar fascia thickness asessement2.jpg|frameless|700x700px]] | ||
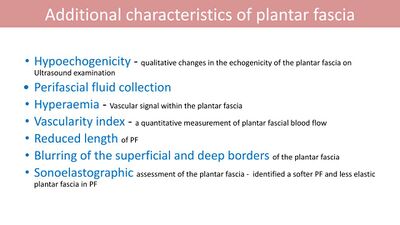
Additional imaging findings related to the plantar fascia can be found in Figure 8 <ref name=":2" /><ref name=":0" /><ref name=":0" /><ref name=":7" /> | Additional imaging findings related to the plantar fascia can be found in Figure 8.<ref name=":2" /><ref name=":0" /><ref name=":0" /><ref name=":7" /> | ||
[[File:Additional characteristics of PF on imaging.jpg|frameless|400x400px]] | [[File:Additional characteristics of PF on imaging.jpg|frameless|400x400px]] | ||
| Line 67: | Line 71: | ||
'''<u>Imaging of other structures in the foot</u>''' | '''<u>Imaging of other structures in the foot</u>''' | ||
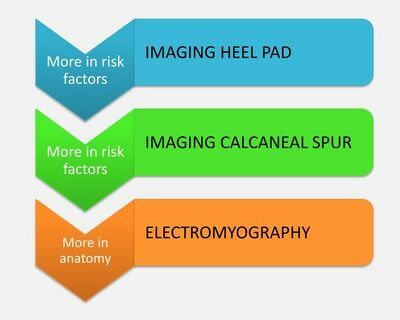
Besides plantar fascia thickness, heel pads and calcaneal spurs are also evident on imaging, but, as | Besides plantar fascia thickness, [[Heel Fat Pad Syndrome|heel pads]] and [[Calcaneal Spurs|calcaneal spurs]] are also evident on imaging, but, as discussed [[Risk Factors for the Development of Plantar Heel Pain Syndrome - A Literature Review|here]], are not significant in PHPS. The influence of electromyography will be discussed in more depth in the anatomy course (Figure 9). | ||
[[File:Imaging in PHPS.jpg|frameless|400x400px]] | [[File:Imaging in PHPS.jpg|frameless|400x400px]] | ||
| Line 73: | Line 77: | ||
'''Figure 9'''. Imaging of other structures of the foot <ref name=":0" /> | '''Figure 9'''. Imaging of other structures of the foot <ref name=":0" /> | ||
Even though medical imaging studies can be useful in detecting abnormalities in the feet of individuals with heel pain, there is still | Even though medical imaging studies can be useful in detecting abnormalities in the feet of individuals with heel pain, there is still controversy about its ability to identify individuals with PHPS and to reflect meaningful changes in the condition of the patient. It is also not commonly available to many clinicians for the on-site assessment of patients.<ref name=":1" /> | ||
[[File:Imaging assessment and PHPS2.jpg|frameless|700x700px]] | [[File:Imaging assessment and PHPS2.jpg|frameless|700x700px]] | ||
| Line 79: | Line 83: | ||
==== Tinel’s Tarsal Tunnel Test ==== | ==== Tinel’s Tarsal Tunnel Test ==== | ||
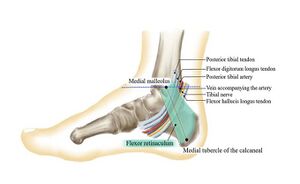
[[File:Tarsal tunnel.jpg|thumb|'''Figure 10'''. Structures in the tarsal tunnel]] | [[File:Tarsal tunnel.jpg|thumb|'''Figure 10'''. Structures in the tarsal tunnel]] | ||
Tarsal tunnel syndrome | [[Tarsal Tunnel Syndrome|Tarsal tunnel syndrome]] is an entrapment of the tibial nerve or its branches in the fibrous tarsal tunnel. It has also been proposed as a cause of plantar heel pain (Figure 10).<ref>Rose B, Singh D. [https://www.researchgate.net/profile/Barry-Rose-2/publication/338010233_Inferior_heel_pain/links/6019eb1892851c4ed545dc70/Inferior-heel-pain.pdf Inferior heel pain]. Orthopaedics and Trauma. 2020 Feb 1;34(1):10-6. </ref><ref name=":10">Rinkel WD, Cabezas MC, Birnie E, Coert JH. [https://sci-hub.se/10.1097/PRS.0000000000004839 The natural history of tarsal tunnel syndrome in diabetic subjects]. Journal of Plastic, Reconstructive & Aesthetic Surgery. 2020 Aug 1;73(8):1482-9. </ref> [[Tinel’s Test|Tinel’s tarsal tunnel test]], which involves tapping on the tibial nerve at the tarsal tunnel to elicit pain/tingling in the heel, has therefore been suggested as an assessment for PHPS (Figure 10).<ref name=":0" /><ref name=":10" /> There is, however, currently no evidence to support the use of Tinel’s tarsal tunnel test in PHPS. | ||
[[File:Tinel's test and PHPS.jpg|frameless|700x700px]] | [[File:Tinel's test and PHPS.jpg|frameless|700x700px]] | ||
==== Patient Reported Outcomes ==== | ==== Patient Reported Outcomes ==== | ||
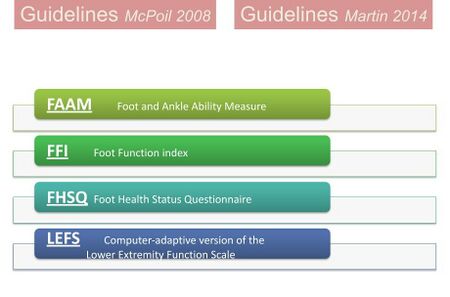
Following the lack of objective measures to assess PHPS, many studies have used patient reported outcomes | "Patient Reported Outcomes (PRO) is directly reported by the patient without interpretation of the patient’s response by a clinician or anyone else and pertains to the patient’s health, quality of life, or functional status associated with health care or treatment". <ref>Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.4 (updated August 2023). Cochrane, 2023. Available from https://training.cochrane.org/handbook [last access 22.10.2023]</ref> Following the lack of objective measures to assess PHPS, many studies have used [[Outcome Measures|patient reported outcomes]] as a way to gauge the efficacy of treatment modalities in individuals with PHPS.<ref name=":1" /> Both clinical guidelines on heel pain by the American Physical Therapy Association <ref name=":6" /><ref name=":11">McPoil TG, Martin RL, Cornwall MW, Wukich DK, Irrgang JJ, Godges JJ. [https://www.jospt.org/doi/pdf/10.2519/jospt.2008.0302 Heel pain—plantar fasciitis]. journal of orthopaedic & sports physical therapy. 2008 Apr;38(4):A1-8. </ref> recommended the use of four different PROs in the assessment of PHPS (Figure 11). | ||
[[File:Guidelines for PROs for PHPS.jpg|frameless|450x450px]] | [[File:Guidelines for PROs for PHPS.jpg|frameless|450x450px]] | ||
| Line 90: | Line 94: | ||
'''Figure 11'''. Patient reported outcomes recommended by the Clinical Guidelines of the American Physical Therapy Association <ref name=":0" /><ref name=":6" /><ref name=":11" /> | '''Figure 11'''. Patient reported outcomes recommended by the Clinical Guidelines of the American Physical Therapy Association <ref name=":0" /><ref name=":6" /><ref name=":11" /> | ||
Martin et al <ref name=":12">Martin RL, Irrgang JJ. [https://www.jospt.org/doi/pdf/10.2519/jospt.2007.2403 A survey of self-reported outcome instruments for the foot and ankle]. Journal of Orthopaedic & Sports Physical Therapy. 2007 Feb;37(2):72-84. </ref> proposed that in order to properly interpret their scores, outcome measures for the foot and ankle should possess four distinct qualities | Martin et al. <ref name=":12">Martin RL, Irrgang JJ. [https://www.jospt.org/doi/pdf/10.2519/jospt.2007.2403 A survey of self-reported outcome instruments for the foot and ankle]. Journal of Orthopaedic & Sports Physical Therapy. 2007 Feb;37(2):72-84. </ref> proposed that in order to properly interpret their scores, outcome measures for the foot and ankle should possess four distinct qualities. These qualities should be considered by clinicians when selecting and using an outcome measure (Figure 12). | ||
[[File:Four categories of evidence for PRO.jpg|frameless|450x450px]] | [[File:Four categories of evidence for PRO.jpg|frameless|450x450px]] | ||
| Line 96: | Line 100: | ||
'''Figure 12'''. Categories of evidence for PROs <ref name=":0" /><ref name=":12" /> | '''Figure 12'''. Categories of evidence for PROs <ref name=":0" /><ref name=":12" /> | ||
Following this, Martin et al <ref name=":12" /> recommended the use of | Following this, Martin et al. <ref name=":12" /> recommended the use of five instruments in individuals with foot and ankle-related pathology, four of which also coincided with those proposed by the Clinical Guidelines of the American Physical Therapy Association (Figure 13).<ref name=":6" /><ref name=":11" /> | ||
[[File:Self reported outcome measures for the foot and ankle Martin 2007.jpg|frameless|450x450px]] | [[File:Self reported outcome measures for the foot and ankle Martin 2007.jpg|frameless|450x450px]] | ||
| Line 102: | Line 106: | ||
'''Figure 13'''. Self-reported outcome measures for the foot and ankle <ref name=":0" /><ref name=":6" /> <ref name=":11" /><ref name=":12" /> | '''Figure 13'''. Self-reported outcome measures for the foot and ankle <ref name=":0" /><ref name=":6" /> <ref name=":11" /><ref name=":12" /> | ||
In a meta-analysis study of the foot and ankle literature from 2002-2011, Hunt et al <ref name=":13">Hunt KJ, Hurwit D. [https://journals.lww.com/jbjsjournal/Abstract/2013/08210/Use_of_Patient_Reported_Outcome_Measures_in_Foot.20.aspx Use of patient-reported outcome measures in foot and ankle research]. JBJS. 2013 Aug 21;95(16):e118. </ref> identified 139 different questionnaires for foot pain. The five most popular | In a meta-analysis study of the foot and ankle literature from 2002-2011, Hunt et al. <ref name=":13">Hunt KJ, Hurwit D. [https://journals.lww.com/jbjsjournal/Abstract/2013/08210/Use_of_Patient_Reported_Outcome_Measures_in_Foot.20.aspx Use of patient-reported outcome measures in foot and ankle research]. JBJS. 2013 Aug 21;95(16):e118. </ref> identified 139 different questionnaires for foot pain. The five most popular PROs used included the [[Foot Function Index (FFI)|Foot Function Index]] (FFI), which was also included in the Clinical Guidelines (Figure 14).<ref name=":6" /><ref name=":11" /><ref name=":13" /> | ||
| Line 108: | Line 113: | ||
[[File:Most popular PROs Hunt 2013.jpg|frameless|450x450px]] | [[File:Most popular PROs Hunt 2013.jpg|frameless|450x450px]] | ||
'''Figure 14'''. The five most popular | '''Figure 14'''. The five most popular PROs for ankle and foot pain <ref name=":0" /><ref name=":13" /> | ||
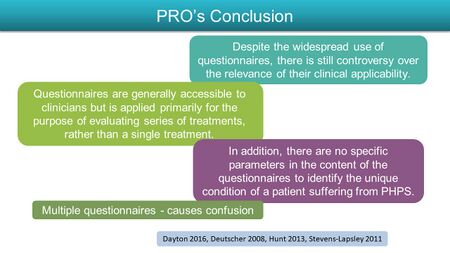
Figure 15 contains a few concluding points that should be considered when using PROs.<ref name=":0" /> | |||
[[File:Conclusion on PROs.jpg|frameless|450x450px]] | [[File:Conclusion on PROs.jpg|frameless|450x450px]] | ||
'''Figure 15'''. Conclusion on | '''Figure 15'''. Conclusion on PROs <ref name=":0" /> | ||
PROs might be ideal for determining the patient’s perception of their abilities, but fail to fully capture the extent of the patient’s functioning.<ref name=":1" /> PROs are therefore more useful for assessing a series of treatments rather than individual treatments.<ref name=":1" /> | |||
[[File:PROs and PHPS.jpg|frameless|700x700px]] | [[File:PROs and PHPS.jpg|frameless|700x700px]] | ||
== What do Physiotherapists do? == | == What do Physiotherapists do? == | ||
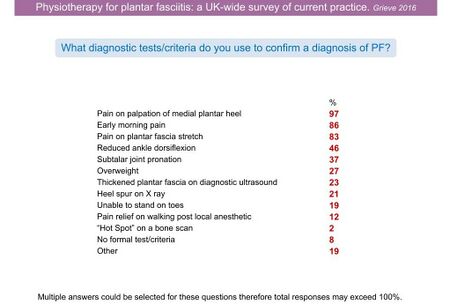
Because there is a lack of objective measures for assessing PHPS, Grieve and Palmer <ref name=":14">Grieve R, Palmer S. [https://uwe-repository.worktribe.com/OutputFile/886548 Physiotherapy for plantar fasciitis: a UK-wide survey of current practice]. Physiotherapy. 2017 Jun 1;103(2):193-200. </ref> conducted an online survey by UK physiotherapists on the current approach to plantar fasciitis. They received 257 completed questionnaires in response to their survey. A summary of their findings is displayed in Figure 16. <ref name=":0" /><ref name=":14" /> | |||
[[File:Current PT practice for dx PF.jpg|frameless|450x450px]] | [[File:Current PT practice for dx PF.jpg|frameless|450x450px]] | ||
| Line 127: | Line 132: | ||
'''Figure 16'''. Current Practice of Physiotherapists for diagnosing plantar fasciitis <ref name=":0" /><ref name=":14" /> | '''Figure 16'''. Current Practice of Physiotherapists for diagnosing plantar fasciitis <ref name=":0" /><ref name=":14" /> | ||
However, each of these factors can be faulted based on a lack of supporting evidence, as discussed [[Risk Factors for the Development of Plantar Heel Pain Syndrome - A Literature Review|here]]. This reiterates that there is a lack of evidence for physical examination tests to be used in the clinical assessment of patients with PHPS and brings us to the aim of this course series - the [[A New Protocol for Plantar Heel Pain|introduction of a new protocol for PHPS]]. Saban and Masharawi<ref name=":1" /> have identified three clinical tests that can provoke the relevant heel pain in individuals with PHPS and, therefore, be useful in assessing PHPS. These tests are as follows: | |||
* Single-leg static stance | |||
* Single-leg half squat | |||
* Single-leg heel raise | |||
== Conclusion == | |||
Based on the review of available literature, the following are assessment recommendations for plantar heel pain: | |||
# The Windlass test is not sensitive enough for diagnosis of PHPS | |||
# Palpation and Pressure Point Threshold are not recommended for PHPS assessment | |||
# Imaging of plantar fascia assessing tissue thickness is useful as a diagnostic tool for patients with plantar heel pain. However, it does not measure the change in patients' condition. | |||
# No evidence supports Tinel's Tarsal Tunnel Test as an assessment tool for PHPS. | |||
# Patient Reported Outcomes (PROs) can be used to evaluate an entire series of treatments. PROs are commonly used for research purposes. | |||
== References == | == References == | ||
| Line 135: | Line 153: | ||
[[Category:Foot - Assessment and Examination]] | [[Category:Foot - Assessment and Examination]] | ||
[[Category:Foot - Conditions]] | [[Category:Foot - Conditions]] | ||
[[Category: | [[Category:Plus Content]] | ||
Latest revision as of 10:09, 22 October 2023
Original Editor - Merinda Rodseth based on the course by
Bernice Saban
Top Contributors - Merinda Rodseth, Jess Bell, Kim Jackson, Ewa Jaraczewska and Olajumoke Ogunleye
Introduction[edit | edit source]
The diagnosis of plantar heel pain syndrome (PHPS) is predominantly based on the symptoms of the patient together with manual palpation of the painful heel.[1][2] Validation of this diagnosis through the use of a reliable clinical test is, however, still elusive. This is significant as valid assessment tools are necessary to ensure optimal management. These tools not only ensure health professionals can assess the status of the patient, but they also highlight the efficacy of treatment and guide which treatment methods to use.
This article will provide an analysis of the available literature on the assessment of PHPS.
Assessment Tools for PHPS[edit | edit source]
A variety of tests have been proposed for the assessment and diagnosis of PHPS, but none have been accepted as the “gold standard”.[1] This necessitates an analysis of the available research to identify which of the proposed tests are reliable and valid for assessing PHPS (Figure 1).
Figure 1. Assessment tools for PHPS [3]
Windlass Test[edit | edit source]
The “windlass mechanism” describes the way in which the plantar fascia supports the foot during weight-bearing activities while providing information about the biomechanical stresses placed on the plantar fascia.[4] Hicks[5] originally described the foot and its ligaments as an “arch-like triangular structure” with the plantar fascia forming the base/tie-rod that runs from the calcaneus to the phalanges.[4] In the propulsive phase of gait, the plantar fascia is wound around the head of the first metatarsal during ankle and hallux dorsiflexion. This shortens the distance between the calcaneus and the metatarsals. The shortening of the plantar fascia that results from dorsiflexion of the big toe simulates the “windlass” (tightening rope/cable) mechanism.[4]
The Windlass Test, therefore, induces strain on the plantar fascia through forced dorsiflexion of the great toe. This strain is associated with increased pain at the site of the insertion of the plantar fascia in patients with plantar fasciitis.[6] However, when De Garceau et al. [6] studied the association between the diagnosis of plantar fasciitis and the results of the windlass test, they found that even though the test is specific for PHPS, it has a low rate of sensitivity which limits its value in clinical evaluation (Figure 2).
Figure 2. The association between the diagnosis of plantar fasciitis and the windlass test results [3][6]
The strain induced with first metatarsal extension was also not limited to the plantar fascia alone, but included various structures in the foot, including the tibial nerve and the medial plantar nerve.[7]
Palpation of the Painful Heel Area[edit | edit source]
Manual palpation of the heel by thumb pressure is a common tool used by clinicians to locate the exact site of pain. It has been proposed that this can aid with both diagnosis and the prescription of treatment in patients with PHPS.[3][8][9][10] No study has, however, quantified the mechanical pressure needed to elicit pain in patients with PHPS and no clinical trials exist to support it as a valid assessment tool for PHPS.[3][8]
Saban and Masharawi[8] used pain pressure threshold (PPT) to assess the area and extent of pain sensitivity in individuals with and without heel pain (Figure 3). They identified the anterior medial heel as the most sensitive location in the heel, but no significant differences were found between those with and without heel pain (Figure 4). This means the test is not sensitive enough for PHPS and is, therefore, not a diagnostic tool for heel pain. [8]
Imaging[edit | edit source]
Imaging is generally useful for acquiring accurate diagnoses, prompting appropriate treatment and determining prognosis.[2] Various imaging methods, including conventional radiograph, ultrasound and magnetic resonance imaging (MRI), have been used to assess various structures implicated in plantar heel pain (Figure 5).[1][2][3][11][12][13]
Figure 5. Imaging modalities and tissues examined [3]
Imaging of the plantar fascia
Individuals with PHPS were found to be 105 times more likely to present with a thickened plantar fascia measuring more than 4.0 mm compared to those without making it a reliable sign of PHPS.[2][12]
Following this, Mahowald et al. [14] investigated the correlation between plantar fascia thickness and symptoms of plantar fasciitis as a way to gauge the efficacy of treatment modalities. They found that a reduction in pain correlated strongly with a reduction in plantar fascia thickness. The thickness of the plantar fascia, however, remained above 4 mm, which would still be indicative of PHPS (Figure 6).[3][14]
Rathleff et al. [15] used thickness of the plantar fascia as an outcome measure to assess the efficacy of shoe inserts and plantar fascia specific stretching vs shoe inserts and high-load strength training in patients with plantar fasciitis. They also reported a reduction in plantar fascia thickness in both groups, but similarly the plantar fascia thickness remained more than 4 mm (Figure 7).[3][15]
Additional imaging findings related to the plantar fascia can be found in Figure 8.[2][3][3][12]
Figure 8. Additional characteristics of the plantar fascia as evident with imaging [3]
Imaging of other structures in the foot
Besides plantar fascia thickness, heel pads and calcaneal spurs are also evident on imaging, but, as discussed here, are not significant in PHPS. The influence of electromyography will be discussed in more depth in the anatomy course (Figure 9).
Figure 9. Imaging of other structures of the foot [3]
Even though medical imaging studies can be useful in detecting abnormalities in the feet of individuals with heel pain, there is still controversy about its ability to identify individuals with PHPS and to reflect meaningful changes in the condition of the patient. It is also not commonly available to many clinicians for the on-site assessment of patients.[1]
Tinel’s Tarsal Tunnel Test[edit | edit source]
Tarsal tunnel syndrome is an entrapment of the tibial nerve or its branches in the fibrous tarsal tunnel. It has also been proposed as a cause of plantar heel pain (Figure 10).[16][17] Tinel’s tarsal tunnel test, which involves tapping on the tibial nerve at the tarsal tunnel to elicit pain/tingling in the heel, has therefore been suggested as an assessment for PHPS (Figure 10).[3][17] There is, however, currently no evidence to support the use of Tinel’s tarsal tunnel test in PHPS.
Patient Reported Outcomes[edit | edit source]
"Patient Reported Outcomes (PRO) is directly reported by the patient without interpretation of the patient’s response by a clinician or anyone else and pertains to the patient’s health, quality of life, or functional status associated with health care or treatment". [18] Following the lack of objective measures to assess PHPS, many studies have used patient reported outcomes as a way to gauge the efficacy of treatment modalities in individuals with PHPS.[1] Both clinical guidelines on heel pain by the American Physical Therapy Association [9][19] recommended the use of four different PROs in the assessment of PHPS (Figure 11).
Figure 11. Patient reported outcomes recommended by the Clinical Guidelines of the American Physical Therapy Association [3][9][19]
Martin et al. [20] proposed that in order to properly interpret their scores, outcome measures for the foot and ankle should possess four distinct qualities. These qualities should be considered by clinicians when selecting and using an outcome measure (Figure 12).
Figure 12. Categories of evidence for PROs [3][20]
Following this, Martin et al. [20] recommended the use of five instruments in individuals with foot and ankle-related pathology, four of which also coincided with those proposed by the Clinical Guidelines of the American Physical Therapy Association (Figure 13).[9][19]
Figure 13. Self-reported outcome measures for the foot and ankle [3][9] [19][20]
In a meta-analysis study of the foot and ankle literature from 2002-2011, Hunt et al. [21] identified 139 different questionnaires for foot pain. The five most popular PROs used included the Foot Function Index (FFI), which was also included in the Clinical Guidelines (Figure 14).[9][19][21]
Figure 14. The five most popular PROs for ankle and foot pain [3][21]
Figure 15 contains a few concluding points that should be considered when using PROs.[3]
Figure 15. Conclusion on PROs [3]
PROs might be ideal for determining the patient’s perception of their abilities, but fail to fully capture the extent of the patient’s functioning.[1] PROs are therefore more useful for assessing a series of treatments rather than individual treatments.[1]
What do Physiotherapists do?[edit | edit source]
Because there is a lack of objective measures for assessing PHPS, Grieve and Palmer [22] conducted an online survey by UK physiotherapists on the current approach to plantar fasciitis. They received 257 completed questionnaires in response to their survey. A summary of their findings is displayed in Figure 16. [3][22]
Figure 16. Current Practice of Physiotherapists for diagnosing plantar fasciitis [3][22]
However, each of these factors can be faulted based on a lack of supporting evidence, as discussed here. This reiterates that there is a lack of evidence for physical examination tests to be used in the clinical assessment of patients with PHPS and brings us to the aim of this course series - the introduction of a new protocol for PHPS. Saban and Masharawi[1] have identified three clinical tests that can provoke the relevant heel pain in individuals with PHPS and, therefore, be useful in assessing PHPS. These tests are as follows:
- Single-leg static stance
- Single-leg half squat
- Single-leg heel raise
Conclusion[edit | edit source]
Based on the review of available literature, the following are assessment recommendations for plantar heel pain:
- The Windlass test is not sensitive enough for diagnosis of PHPS
- Palpation and Pressure Point Threshold are not recommended for PHPS assessment
- Imaging of plantar fascia assessing tissue thickness is useful as a diagnostic tool for patients with plantar heel pain. However, it does not measure the change in patients' condition.
- No evidence supports Tinel's Tarsal Tunnel Test as an assessment tool for PHPS.
- Patient Reported Outcomes (PROs) can be used to evaluate an entire series of treatments. PROs are commonly used for research purposes.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Saban B, Masharawi Y. Three single leg standing tests for clinical assessment of chronic plantar heel pain syndrome: static stance, half-squat and heel rise. Physiotherapy. 2017 Jun 1;103(2):237-44.
- ↑ 2.0 2.1 2.2 2.3 2.4 Draghi F, Gitto S, Bortolotto C, Draghi AG, Belometti GO. Imaging of plantar fascia disorders: findings on plain radiography, ultrasound and magnetic resonance imaging. Insights into imaging. 2017 Feb;8(1):69-78.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 3.17 3.18 3.19 3.20 3.21 3.22 3.23 3.24 Bernice Saban 2021. Assessment of Plantar Heel Pain - A Literature Review. Plus Course. 2021
- ↑ 4.0 4.1 4.2 Bolgla LA, Malone TR. Plantar fasciitis and the windlass mechanism: a biomechanical link to clinical practice. Journal of athletic training. 2004 Jan;39(1):77.
- ↑ Hicks JH. The mechanics of the foot: II. The plantar aponeurosis and the arch. Journal of anatomy. 1954 Jan;88(Pt 1):25.
- ↑ 6.0 6.1 6.2 De Garceau D, Dean D, Requejo SM, Thordarson DB. The association between diagnosis of plantar fasciitis and Windlass test results. Foot & ankle international. 2003 Mar;24(3):251-5.
- ↑ Alshami AM, Babri AS, Souvlis T, Coppieters MW. Biomechanical evaluation of two clinical tests for plantar heel pain: the dorsiflexion-eversion test for tarsal tunnel syndrome and the windlass test for plantar fasciitis. Foot & ankle international. 2007 Apr;28(4):499-505.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 Saban B, Masharawi Y. Pain threshold tests in patients with heel pain syndrome. Foot & ankle international. 2016 Jul;37(7):730-6.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 Martin RL, Davenport TE, Reischl SF, McPoil TG, Matheson JW, Wukich DK, McDonough CM, Altman RD, Beattie P, Cornwall M, Davis I. Heel pain—plantar fasciitis: revision 2014. Journal of Orthopaedic & Sports Physical Therapy. 2014 Nov;44(11):A1-33.
- ↑ Drake C, Mallows A, Littlewood C. Psychosocial variables and presence, severity and prognosis of plantar heel pain: A systematic review of cross‐sectional and prognostic associations. Musculoskeletal Care. 2018 Sep;16(3):329-38. DOI:10.1002/msc.1246
- ↑ Allam AE, Chang KV. Plantar Heel Pain. StatPearls [Internet]. 2021 Feb 5.
- ↑ 12.0 12.1 12.2 Riel H, Cotchett M, Delahunt E, Rathleff MS, Vicenzino B, Weir A, Landorf KB. Is ‘plantar heel pain’a more appropriate term than ‘plantar fasciitis’? Time to move on. Br J Sports Med.2017 Nov;51(22):1576-1577.
- ↑ Drake C, Whittaker GA, Kaminski MR, Chen J, Keenan AM, Rathleff MS, et al. Medical imaging for plantar heel pain: a systematic review and meta-analysis. J Foot Ankle Res. 2022 Jan 22;15(1):4.
- ↑ 14.0 14.1 14.2 Mahowald S, Legge BS, Grady JF. The correlation between plantar fascia thickness and symptoms of plantar fasciitis. Journal of the American Podiatric Medical Association. 2011 Sep;101(5):385-9.
- ↑ 15.0 15.1 15.2 Rathleff MS, Mølgaard CM, Fredberg U, Kaalund S, Andersen KB, Jensen TT, Aaskov S, Olesen JL. High‐load strength training improves outcome in patients with plantar fasciitis: A randomized controlled trial with 12‐month follow‐up. Scandinavian journal of medicine & science in sports. 2015 Jun;25(3):e292-300.
- ↑ Rose B, Singh D. Inferior heel pain. Orthopaedics and Trauma. 2020 Feb 1;34(1):10-6.
- ↑ 17.0 17.1 Rinkel WD, Cabezas MC, Birnie E, Coert JH. The natural history of tarsal tunnel syndrome in diabetic subjects. Journal of Plastic, Reconstructive & Aesthetic Surgery. 2020 Aug 1;73(8):1482-9.
- ↑ Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.4 (updated August 2023). Cochrane, 2023. Available from https://training.cochrane.org/handbook [last access 22.10.2023]
- ↑ 19.0 19.1 19.2 19.3 19.4 McPoil TG, Martin RL, Cornwall MW, Wukich DK, Irrgang JJ, Godges JJ. Heel pain—plantar fasciitis. journal of orthopaedic & sports physical therapy. 2008 Apr;38(4):A1-8.
- ↑ 20.0 20.1 20.2 20.3 Martin RL, Irrgang JJ. A survey of self-reported outcome instruments for the foot and ankle. Journal of Orthopaedic & Sports Physical Therapy. 2007 Feb;37(2):72-84.
- ↑ 21.0 21.1 21.2 Hunt KJ, Hurwit D. Use of patient-reported outcome measures in foot and ankle research. JBJS. 2013 Aug 21;95(16):e118.
- ↑ 22.0 22.1 22.2 Grieve R, Palmer S. Physiotherapy for plantar fasciitis: a UK-wide survey of current practice. Physiotherapy. 2017 Jun 1;103(2):193-200.