Acetabulum Fracture: Difference between revisions
Scott Buxton (talk | contribs) mNo edit summary |
(Ref to video) |
||
| (19 intermediate revisions by 10 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor '''- [[User:Lise | '''Original Editor '''- [[User:Lise Delagrange|Lise Delagrange]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
= | == Introduction == | ||
[[File:Bony-pelvis-illustrations.jpeg|right|frameless|Bony-pelvis-illustration]] | |||
The acetabulum is the large cup-shaped cavity on the anterolateral aspect of the [[pelvis]] that articulates with the head of the [[femur]] to form the [[hip]] joint. Acetabular fractures (a type of [[Pelvic Fractures|pelvic fracture]]), possibly involving the [[ilium]], [[ischium]] or [[pubis]] depending on fracture configuration.<ref name=":0">Radiopaedia. Acetabular fracture Available from:https://radiopaedia.org/articles/acetabular-fracture?lang=gb [accessed 17/10/2023]</ref> | |||
== Aetiology == | |||
Possible mechanisms of injury: | |||
The | # '''High-energy trauma''': axial loading of the femur: fall from height; motor vehicle collision; crush injury. | ||
# '''Low-energy trauma''' with abnormal bone: insufficiency fracture e.g. [[Osteoporosis]] makes the bone vulnerable and can cause an acetabulum fracture from a simple low fall. <ref>Kanakaris NK, Davidson A. [https://linkinghub.elsevier.com/retrieve/pii/S1877132722000197 Classification of acetabular fractures: how to apply and relevance today.] Orthopaedics and Trauma. 2022 Apr 1;36(2):61-6.</ref> | |||
== Epidemiology == | |||
Acetabular fractures are uncommon. The reported incidence is approximately 3 per 100,000 per year.<ref name=":0" /> Most patients with an acetabular fracture are elderly (> 70 years), of male sex, and the fracture most commonly occurs after a simple, low-energy fall.<ref name=":1">Albrektsson M, Möller M, Wolf O, Wennergren D, Sundfeldt M. [https://pubmed.ncbi.nlm.nih.gov/37652452/ Acetabular fractures: Epidemiology and mortality based on 2,132 fractures from the Swedish Fracture Register.] Bone Jt Open. 2023 Sep 1;4(9):652-658.</ref> Those aged > 70 years, present with a 30-day mortality of 8% and one-year mortality 24%. For patients aged ≤ 70 years, the 30-day mortality is reported to be 0.2% and the one-year mortality 2%. <ref name=":1" /> | |||
== Fracture patterns == | |||
[[File:Hip-joint-illustrations.jpeg|right|frameless|Hip joint]]There are various fracture patterns in the acetabulum. For the classification of these fractures, the Judet-Letournel classification is the most accepted system. The five most common fractures, representative for 90% of all, are: <ref name="p3">Durkee NJ, Jacobson J, Jamadar D, Karunakar MA, Morag Y, Hayes C. [https://pubmed.ncbi.nlm.nih.gov/16985135/ Classification of common acetabular fractures: radiographic and CT appearances.] AJR Am J Roentgenol. 2006 Oct 1;187(4):915-25.</ref> | |||
= | # '<nowiki/>''Both''' '''column''': This is a fracture that involves the anterior and posterior column and extends through the obturator ring. The characteristic for this fracture is the spur sign. It is a sign that represents the displacement of the fracture involving sciatic buttress. When this is present, the acetabulum can no longer carry the weight of the upper body. | ||
# '''Transverse''': This fracture involves both anterior and posterior column. This means that the iliopectineal and ilioischial lines of the pelvis are discontinued. | |||
# '''T-shaped''': Similar to the transverse fractures, the difference is that the T-shaped also extends inferiorly into the obturator ring. What differentiates it from the both column fracture is that the fracture doesn’t involve the extension to the iliac wing. | |||
# ''''''Trans'''''<b>verse' with posterior wall</b>: This is a transverse fracture only there is also a comminution of the posterior wall. | |||
# ''<i><nowiki/>'Isolated '<nowiki/></i>posterior '<nowiki/>'''''wall''': One of the most common acetabulum fractures with a preponderance of 27%. The posterior wall in this fracture is comminuted. The iliopectineal line is not disrupted but the ilioischial line may be. <ref name="p3" /><ref name="p2">Tile M, Helfet DL, Kellam JF, Vrahas M. [https://www.academia.edu/31826728/Smith_Fractures_of_the_Pelvis_and_Acetabulum Fractures of the pelvis and acetabulum]. Third edition. Baltimore: Williams & Wilkins; 2011.</ref> <ref name="p8">Liu X, Xu S, Zhang C, Su J, Yu B. [https://pubmed.ncbi.nlm.nih.gov/20012433/ Application of a shape-memory alloy internal fixator for treatment of acetabular fractures with a follow-up of two to nine years in China.] Int Orthop. 2010 Oct;34(7):1033-40.</ref> | |||
{{#ev:youtube|d4_R7y-c7LU}}<ref>Ebraheim N. Acetabular fractures. All you need to know. Available from: https://www.youtube.com/watch?time_continue=33&v=d4_R7y-c7LU&embeds_referring_euri=https%3A%2F%2Fwww.physio-pedia.com%2F&source_ve_path=Mjg2NjQsMjg2NjY&feature=emb_logo [accessed 17/10/2023]</ref> | |||
== Diagnosis == | |||
<br> | CT has revolutionised the diagnosis, enabling precise delineation of the fracture configuration and assessment of any articular surface disruption.<ref name=":0" /><br>The radiograph gives a clear view of all the essential fundamental landmarks of the acetabulum.<br>On a CT-scan, you can see full 3D- reconstruction of the acetabulum, which facilitates the visualization of the fracture, the degree of the fracture and the associated fractures.<ref name="p9">Balendra G, Bassett JW, Acharya M. [https://www.sciencedirect.com/science/article/abs/pii/S1877132722000276 The ABC management of the acetabular fracture patient.] Orthopaedics and Trauma. 2022 Mar 25.</ref> | ||
= | == Medical Management == | ||
Treatment depends on several factors including both patient factors and fracture characteristics. Treatment, whether operative or non-operative will usually be followed by a period of non-weight bearing on the affected side (or both). Close radiographic follow-up is required. <ref name=":0" /> | |||
If the displacement of the fragment is greater than 3mm, operation is primarily suggested.<ref name="p2" /> Non-operative management may be indicated in the setting of a minimally displaced fracture. This strategy is more common in developing countries. <ref name=":0" /> Acetabulum fractures often require an open reduction internal fixation (ORIF) to restore joint congruency and stabilisation. For the operation, they use screws and plates to fix the bone to prevent further displacement. <ref name="p8" /><ref name="p4">Stilger VG, Alt JM, Hubbard DF. [https://pubmed.ncbi.nlm.nih.gov/16558600/ Traumatic acetabular fracture in an intercollegiate football player: a case report.] J Athl Train. 2000 Jan;35(1):103-7.</ref> With elderly patients, ORIF may not always be the best option because of possible osteoporosis. ORIF can be the solution to the fracture if the femoral head is still weight bearing and when the patient factors are no immediate cause to any complication. Patient factors include degree of underlying osteoporosis, comorbid medical conditions, preexisting degenerative joint disease (DJD), premorbid activity level, and baseline mental function. <ref name="p7">Pagenkopf E, Grose A, Partal G, Helfet DL. [https://pubmed.ncbi.nlm.nih.gov/18751831/ Acetabular fractures in the elderly: treatment recommendations.] HSS J. 2006 Sep;2(2):161-71.</ref> In general, [[Total Hip Replacement|total hip replacement]] (THR) will provide the best functional outcome in elderly patients with severe acetabulum fracture and osteoporosis. <ref name="p5">Cornell CN. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2504130/ Management of acetabular fractures in the elderly patient.] HSS J. 2005 Sep;1(1):25-30.</ref> THR promotes quicker mobilisation and rehabilitation as well as symptomatic relief of elderly patients, when compared to ORIF or non-operative treatment. <ref>Ebrahimi HDN, Wu CH, Karczewski D, Amini DA, Dahne M, Bäcker HC. [https://pubmed.ncbi.nlm.nih.gov/37543998/ Total hip arthroplasty in acute acetabulum fractures: a systematic review.] Arch Orthop Trauma Surg. 2023 Nov;143(11):6665-6673.</ref> | |||
== Physiotherapy Management == | |||
Nonoperative treatment is usually recommended for patients with no displacement or minimal displacement like low anterior column or low transverse fractures, so the superior part of the acetabulum must be intact. <ref name="p0">Cochu G, Mabit C, Gougam T, Fiorenza F, Baertich C, Charissoux JL, Arnaud JP. [https://pubmed.ncbi.nlm.nih.gov/18166954/ Total hip arthroplasty for treatment of acute acetabular fracture in elderly patients.] Rev Chir Orthop Reparatrice Appar Mot. 2007 Dec 1;93(8):818-27. [Article in French]</ref><br>Early mobilisation is necessary because prolonged recumbency can be life- threatening.<ref name="p7" /> Conservative treatment may include pain control, functional physical therapy and radiographic follow-up. <ref name="p7" /> Physiotherapy may aso involve gait training, stabilisation exercises and mobility training. | |||
< | Patients who underwent an operation have to start with passive ROM exercises followed by active non-weight bearing such as a series of flexion/extension. Partial weight-bearing with stepwise progression usually starts at 6 weeks postoperatively and full weight bearing is eventually allowed at 10 weeks. <ref name="p2" /> <ref name="p1">Kristan A, Mavcic B, Cimerman M, Iglic A, Tonin M, Slivnik T, Kralj-Iglic V, Daniel M. [https://www.researchgate.net/publication/3430812_Acetabular_Loading_in_Active_Abduction Acetabular loading in active abduction.] IEEE Transactions on Neural Systems and Rehabilitation Engineering. 2007 Jun 18;15(2):252-7.</ref> However, compliance to the generally accepted weight-bearing limits is reported to be low. <ref name=":2">Braun BJ, Histing T, Rollmann MFR, Menger MM, Osche D, Orth M, Pohlemann T, Herath SC. [https://pubmed.ncbi.nlm.nih.gov/35621406/ Weight-Bearing Restrictions after Acetabular Fracture, Necessity or False Hope? A Brief Observational Study.] Acta Chir Orthop Traumatol Cech. 2022;89(2):146-9.</ref> Nevertheless, non-compliance does not seem to influence the radiographic outcome. <ref name=":2" /> | ||
= | == References == | ||
<references /> | |||
[[Category:Musculoskeletal/Orthopaedics|Orthopaedics]] | |||
[[Category:Hip]] | |||
[[Category:Conditions]] | |||
[[Category:Hip - Conditions]] | |||
[[Category:Fractures]] | |||
[[Category:Injury]] | |||
[[Category: | |||
Latest revision as of 21:02, 17 October 2023
Original Editor - Lise Delagrange
Top Contributors - Scott Buxton, Lauren Lopez, Lucinda hampton, Angeliki Chorti, 127.0.0.1, Lise Delagrange, Candace Goh, Tony Lowe, Kim Jackson, Admin, Didzis Rozenbergs, Sweta Christian and WikiSysop
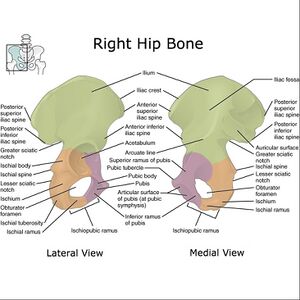
Introduction[edit | edit source]
The acetabulum is the large cup-shaped cavity on the anterolateral aspect of the pelvis that articulates with the head of the femur to form the hip joint. Acetabular fractures (a type of pelvic fracture), possibly involving the ilium, ischium or pubis depending on fracture configuration.[1]
Aetiology[edit | edit source]
Possible mechanisms of injury:
- High-energy trauma: axial loading of the femur: fall from height; motor vehicle collision; crush injury.
- Low-energy trauma with abnormal bone: insufficiency fracture e.g. Osteoporosis makes the bone vulnerable and can cause an acetabulum fracture from a simple low fall. [2]
Epidemiology[edit | edit source]
Acetabular fractures are uncommon. The reported incidence is approximately 3 per 100,000 per year.[1] Most patients with an acetabular fracture are elderly (> 70 years), of male sex, and the fracture most commonly occurs after a simple, low-energy fall.[3] Those aged > 70 years, present with a 30-day mortality of 8% and one-year mortality 24%. For patients aged ≤ 70 years, the 30-day mortality is reported to be 0.2% and the one-year mortality 2%. [3]
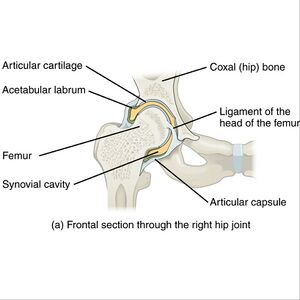
Fracture patterns[edit | edit source]
There are various fracture patterns in the acetabulum. For the classification of these fractures, the Judet-Letournel classification is the most accepted system. The five most common fractures, representative for 90% of all, are: [4]
- 'Both' column: This is a fracture that involves the anterior and posterior column and extends through the obturator ring. The characteristic for this fracture is the spur sign. It is a sign that represents the displacement of the fracture involving sciatic buttress. When this is present, the acetabulum can no longer carry the weight of the upper body.
- Transverse: This fracture involves both anterior and posterior column. This means that the iliopectineal and ilioischial lines of the pelvis are discontinued.
- T-shaped: Similar to the transverse fractures, the difference is that the T-shaped also extends inferiorly into the obturator ring. What differentiates it from the both column fracture is that the fracture doesn’t involve the extension to the iliac wing.
- 'Transverse' with posterior wall: This is a transverse fracture only there is also a comminution of the posterior wall.
- 'Isolated 'posterior 'wall: One of the most common acetabulum fractures with a preponderance of 27%. The posterior wall in this fracture is comminuted. The iliopectineal line is not disrupted but the ilioischial line may be. [4][5] [6]
Diagnosis[edit | edit source]
CT has revolutionised the diagnosis, enabling precise delineation of the fracture configuration and assessment of any articular surface disruption.[1]
The radiograph gives a clear view of all the essential fundamental landmarks of the acetabulum.
On a CT-scan, you can see full 3D- reconstruction of the acetabulum, which facilitates the visualization of the fracture, the degree of the fracture and the associated fractures.[8]
Medical Management[edit | edit source]
Treatment depends on several factors including both patient factors and fracture characteristics. Treatment, whether operative or non-operative will usually be followed by a period of non-weight bearing on the affected side (or both). Close radiographic follow-up is required. [1]
If the displacement of the fragment is greater than 3mm, operation is primarily suggested.[5] Non-operative management may be indicated in the setting of a minimally displaced fracture. This strategy is more common in developing countries. [1] Acetabulum fractures often require an open reduction internal fixation (ORIF) to restore joint congruency and stabilisation. For the operation, they use screws and plates to fix the bone to prevent further displacement. [6][9] With elderly patients, ORIF may not always be the best option because of possible osteoporosis. ORIF can be the solution to the fracture if the femoral head is still weight bearing and when the patient factors are no immediate cause to any complication. Patient factors include degree of underlying osteoporosis, comorbid medical conditions, preexisting degenerative joint disease (DJD), premorbid activity level, and baseline mental function. [10] In general, total hip replacement (THR) will provide the best functional outcome in elderly patients with severe acetabulum fracture and osteoporosis. [11] THR promotes quicker mobilisation and rehabilitation as well as symptomatic relief of elderly patients, when compared to ORIF or non-operative treatment. [12]
Physiotherapy Management[edit | edit source]
Nonoperative treatment is usually recommended for patients with no displacement or minimal displacement like low anterior column or low transverse fractures, so the superior part of the acetabulum must be intact. [13]
Early mobilisation is necessary because prolonged recumbency can be life- threatening.[10] Conservative treatment may include pain control, functional physical therapy and radiographic follow-up. [10] Physiotherapy may aso involve gait training, stabilisation exercises and mobility training.
Patients who underwent an operation have to start with passive ROM exercises followed by active non-weight bearing such as a series of flexion/extension. Partial weight-bearing with stepwise progression usually starts at 6 weeks postoperatively and full weight bearing is eventually allowed at 10 weeks. [5] [14] However, compliance to the generally accepted weight-bearing limits is reported to be low. [15] Nevertheless, non-compliance does not seem to influence the radiographic outcome. [15]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Radiopaedia. Acetabular fracture Available from:https://radiopaedia.org/articles/acetabular-fracture?lang=gb [accessed 17/10/2023]
- ↑ Kanakaris NK, Davidson A. Classification of acetabular fractures: how to apply and relevance today. Orthopaedics and Trauma. 2022 Apr 1;36(2):61-6.
- ↑ 3.0 3.1 Albrektsson M, Möller M, Wolf O, Wennergren D, Sundfeldt M. Acetabular fractures: Epidemiology and mortality based on 2,132 fractures from the Swedish Fracture Register. Bone Jt Open. 2023 Sep 1;4(9):652-658.
- ↑ 4.0 4.1 Durkee NJ, Jacobson J, Jamadar D, Karunakar MA, Morag Y, Hayes C. Classification of common acetabular fractures: radiographic and CT appearances. AJR Am J Roentgenol. 2006 Oct 1;187(4):915-25.
- ↑ 5.0 5.1 5.2 Tile M, Helfet DL, Kellam JF, Vrahas M. Fractures of the pelvis and acetabulum. Third edition. Baltimore: Williams & Wilkins; 2011.
- ↑ 6.0 6.1 Liu X, Xu S, Zhang C, Su J, Yu B. Application of a shape-memory alloy internal fixator for treatment of acetabular fractures with a follow-up of two to nine years in China. Int Orthop. 2010 Oct;34(7):1033-40.
- ↑ Ebraheim N. Acetabular fractures. All you need to know. Available from: https://www.youtube.com/watch?time_continue=33&v=d4_R7y-c7LU&embeds_referring_euri=https%3A%2F%2Fwww.physio-pedia.com%2F&source_ve_path=Mjg2NjQsMjg2NjY&feature=emb_logo [accessed 17/10/2023]
- ↑ Balendra G, Bassett JW, Acharya M. The ABC management of the acetabular fracture patient. Orthopaedics and Trauma. 2022 Mar 25.
- ↑ Stilger VG, Alt JM, Hubbard DF. Traumatic acetabular fracture in an intercollegiate football player: a case report. J Athl Train. 2000 Jan;35(1):103-7.
- ↑ 10.0 10.1 10.2 Pagenkopf E, Grose A, Partal G, Helfet DL. Acetabular fractures in the elderly: treatment recommendations. HSS J. 2006 Sep;2(2):161-71.
- ↑ Cornell CN. Management of acetabular fractures in the elderly patient. HSS J. 2005 Sep;1(1):25-30.
- ↑ Ebrahimi HDN, Wu CH, Karczewski D, Amini DA, Dahne M, Bäcker HC. Total hip arthroplasty in acute acetabulum fractures: a systematic review. Arch Orthop Trauma Surg. 2023 Nov;143(11):6665-6673.
- ↑ Cochu G, Mabit C, Gougam T, Fiorenza F, Baertich C, Charissoux JL, Arnaud JP. Total hip arthroplasty for treatment of acute acetabular fracture in elderly patients. Rev Chir Orthop Reparatrice Appar Mot. 2007 Dec 1;93(8):818-27. [Article in French]
- ↑ Kristan A, Mavcic B, Cimerman M, Iglic A, Tonin M, Slivnik T, Kralj-Iglic V, Daniel M. Acetabular loading in active abduction. IEEE Transactions on Neural Systems and Rehabilitation Engineering. 2007 Jun 18;15(2):252-7.
- ↑ 15.0 15.1 Braun BJ, Histing T, Rollmann MFR, Menger MM, Osche D, Orth M, Pohlemann T, Herath SC. Weight-Bearing Restrictions after Acetabular Fracture, Necessity or False Hope? A Brief Observational Study. Acta Chir Orthop Traumatol Cech. 2022;89(2):146-9.