Rhizarthrosis: Difference between revisions
No edit summary |
No edit summary |
||
| (80 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
= | <div class="editorbox"> '''Original Editor '''- [[User:Jona Van den Broeck|Jona Van den Broeck]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== Introduction == | |||
Trapeziometacarpal (TMC) arthritis ( also known as Rhizarthrosis ) is [[arthritis]] of the first carpometacarpal (CMC) joint of the thumb. The CMC joint of the thumb, or TMC joint plays a critical role in the normal [[Hand Function|functioning]] of the thumb. It is the most important joint connecting the [[Wrist and Hand|wrist]] to the metacarpus. [[Osteoarthritis]] of the TMC is a severely disabling condition; it is up to twenty times more common among elderly women than on average.<ref>Wikipedia. [https://en.wikipedia.org/wiki/Carpometacarpal_joint CMC joint]. Accessed 30.09.22</ref> | |||
[[File:Osteoarthritis of the CMC joint.png|alt=an xray image of OA of the first CMC joint|frame|316x316px|left]] | |||
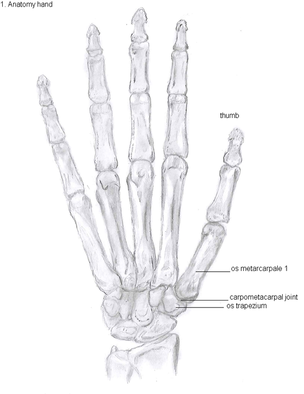
[[File:Anatomy of the hand.png|394x394px|Carpometacarpal Joint of the hand|thumb|center]] | |||
'''Ligaments of the TMC Joint and their functions''' | |||
== | The main ligaments of the TMC Joint are as follows: <ref name=":2" /> <ref name=":4">Lin JD, Karl JW, Strauch RJ. [https://pubmed.ncbi.nlm.nih.gov/23456188/ Trapeziometacarpal joint stability: the evolving importance of the dorsal ligaments]. Clinical Orthopaedics and Related Research®. 2014 Apr 1; 472(4):1138-45. Accessed 30.09.22. </ref> <ref>Imaeda T, An KN, Cooney III WP, Linscheid R. [https://pubmed.ncbi.nlm.nih.gov/8463585/ Anatomy of trapeziometacarpal ligaments]. The Journal of hand surgery. 1993 Mar 1; 18(2):226-31. Accessed 30.09.22. </ref> | ||
* The dorsoradial ligaments (DRL) | |||
* The superficial anterior oblique ligament (AOL) | |||
* The deep anterior oblique ligament (AOL) | |||
* The intermetacarpal ligament (IML) | |||
* The ulnar collateral ligament | |||
* The posterior obique ligament | |||
= | '''Table 1. The Functions of the ligaments (table adapted from Blige & Karalezli 2015''' <ref name=":2" /> | ||
{| class="wikitable" | |||
!Ligament | |||
! | |||
!Function | |||
|- | |||
|'''Dorsoradial''' | |||
! | |||
|Shortest and thickest ligament. Primary stabilizers against dorsal translation of the joint | |||
|- | |||
|'''Anterior oblique''' | |||
!'''Superficial''' | |||
|Stabilization against volar joint subluxation | |||
|- | |||
|'''Anterior oblique''' | |||
!Deep | |||
|It is also known as beak ligament. It acts as a pivot primary joint stabilizer against dorsal translation | |||
|- | |||
|'''Posterior oblique''' | |||
| | |||
|Stabilization of rotation | |||
|- | |||
|'''Intermetacarpal''' | |||
| | |||
|Stabilization during radiovolar translation | |||
|- | |||
|'''Ulnar collateral''' | |||
| | |||
|Helps to stabilize against the volar joint subluxation | |||
|} | |||
< | Although there is a controversy about the primary stabilizers of the TMC Joint, several studies concluded the DRL to be the primary stabilizers <ref>Ripoll G, Glumcher D, Fossati G 2019 [https://medcraveonline.com/MOJAP/anatomical-considerations-of-the-thumb-carpo-metacarpal-joint-ligaments-based-on-a-case-report-of-isolated-joint-dislocation.html Anatomical considerations of the thumb carpometacarpal joint ligaments, based on a case report of isolated joint dislocation] (Accessed 30.09.22) | ||
</ref> <ref name=":4" /> | |||
<sup></sup>{{#ev:youtube|https://www.youtube.com/watch?v=iVbOPCu5Ius|width}}<ref>Mayo clinic. [https://www.youtube.com/watch?v=iVbOPCu5Ius Causes remedies for thumb arthritis.] Accessed 30.09.22</ref> | |||
== Stages of CMC == | |||
= | The CMC stages are usually classified according to the Eaton-Litter Classification which is obtained through radiological procedures or arthroscopy <ref name=":2">Bilge O, Karalezli N. [https://www.wjgnet.com/2220-3214/full/v5/i2/90.htm Current review of trapeziometacarpal osteoarthritis (rhizarthrosis)]. World Journal of Rheumatology. 2015 Jul 12; 5(2):90-5. Accessed 30.09.22 </ref>. It's a staging protocol with four different stages based on synovitis, joint space, and the laxity of the capsule <ref>Wikipedia. [https://en.wikipedia.org/wiki/Trapeziometacarpal_osteoarthritis Trapeziometacarpal osteoarthriti]s. [Accessed, 30.09.22] | ||
</ref>. | |||
< | Here are the four stages of '''Eaton-Litter Classification''' <ref name=":3">Thumb CMC Joint Arthroplasty. Available from:https://www.touchsurgery.com/simulations/thumb-cmc-joint-arthroplasty (Accessed 15 October 2020)</ref>: | ||
''Stage I: Synovitis Phase'' | |||
* Articular contours are normal | |||
* Possible widening of TMC joint that suggests joint effusion or ligament laxity | |||
* No osteophyte formation | |||
''Stage II: Significant Capsular Laxity'' | |||
* Narrowing of CMC joint | |||
* Small osteophyte formation at the ulnar side of the distal trapezial articular surface | |||
* No or 1/3rd CMC joint subluxation | |||
''Stage III: Significant Joint Destruction'' | |||
* Further joint space narrowing with cystic changes and sclerotic bone | |||
* Prominent osteophytes at the ulnar border of distal trapezium | |||
* Moderate subluxation radially and dorsally at the base of the first metacarpal | |||
* Mild arthrosis of the scaphotrapezial joint | |||
==== < | ''Stage IV: Pantrapezial Arthritis'' | ||
* Major subluxation of the joint | |||
* Narrowing of the joint space as in stage 3 | |||
* Cystic and sclerotic subchondral bone changes | |||
* Significant erosion and destruction of scaphotrapezial joint | |||
<section> | |||
Stage 2: Significant Capsular Laxity | |||
* Narrowing of CMC Joint | |||
* Mild Subchondral sclerotic changes | |||
* Small ( < 2mm) osteophyte formation commonly at the distal trapezial articular surface | |||
* No or < 1/3 CMC joint sbluxation in any projection | |||
</section> | |||
== Etiology == | |||
Causes of TMC arthritis are: | |||
* Excessive repetitive use of the CMC joint of the thumb | |||
* Subluxation | |||
* Lesion of the ligaments or a fracture. | |||
* Laxity of the CMC joint can be hereditary, increased risk for ligament injuries, a primary stimulus in the development of arthritis. Also causes hyperextension, which is another primary stimulus for the development of arthritis.<ref>Wolf JM, Schreier S, Tomsick S, Williams A, Petersen B. [https://www.jhandsurg.org/article/S0363-5023(11)00353-4/abstract Radiographic laxity of the trapeziometacarpal joint is correlated with generalized joint hypermobility.] The Journal of hand surgery. 2011 Jul 1;36(7):1165-9. Available from: https://www.jhandsurg.org/article/S0363-5023(11)00353-4/abstract (last accessed 14.4.2019)</ref> | |||
* Weakness of the cross links of the fingers (ligament oblique anterior). These ligaments are the most important stabilizers of the fingers. <ref>A. Gondim Teixeira, Pedro & Omoumi, Patrick & J Trudell, Debra & Ward, Samuel & Blum, Alain & L Resnick, Donald. (2010). High-resolution ultrasound evaluation of the trapeziometacarpal joint with emphasis on the anterior oblique ligament (beak ligament). Skeletal radiology. 40. 897-904. 10.1007/s00256-010-1068-0. Available from: https://www.researchgate.net/publication/49647832_High-resolution_ultrasound_evaluation_of_the_trapeziometacarpal_joint_with_emphasis_on_the_anterior_oblique_ligament_beak_ligament</ref> | |||
* Using thumb in occupation, For example, Work-related thumb pain in physiotherapists is a prevalent problem among physiotherapists who administer manual techniques. Factors that appear to be associated with thumb pain include CMC mobility and thumb strength<ref>Snodgrass SJ, Riyett DA, Chiarelli P, Bates AM, Rowe LJ. [https://www.sciencedirect.com/science/article/pii/S0004951414601409 Factors related to thumb pain in physiotherapists]. Australian Journal of Physiotherapy. 2003 Jan 1;49(4):243-50. Available from:https://www.sciencedirect.com/science/article/pii/S0004951414601409 (last accessed 10.4.2020)</ref>. | |||
< | == <sup> </sup>Signs and Symptoms == | ||
The first signs of arthritis in the thumb are | |||
* pain, tenderness, and stiffness at the base of your thumb. This occurs with gripping, pinching, or clasping something between the thumb and index fingers or when a mild force, such as when you twist a key in a lock or turn a door handle. An ache after activity can also be a feature. | |||
* Decreased strength and range of motion, For example, opening jars or doing up buttons may become difficult. | |||
< | * Appearance. The joint may become swollen or develop a bony bump. The joint may appear squarish and enlarged.<ref>Healthline. [https://www.healthline.com/health/basal-joint-arthritis#symptoms Basal joint arthritis.] Available from: https://www.healthline.com/health/basal-joint-arthritis#symptoms (last accessed 14.4.2019)</ref> | ||
[[File:Grip_.jpg|right|frameless]] | |||
== '''Diagnosis''' == | |||
* Medical and family history | |||
* Noticeable lumps or swelling on the first CMC joint | |||
* [[Thumb CMC Grind Test|Thumb CMC grind test]] | |||
* [[X-Rays|Plain radiograph]]<nowiki/>s showing degenerative changes (bone spurs, thinning of cartilage, loss of joint space) in affected joints are usually diagnostic.<ref name=":1">Mayo clinic. [https://www.mayoclinic.org/diseases-conditions/thumb-arthritis/diagnosis-treatment/drc-20378344 Thumb arthritis.] Available from: https://www.mayoclinic.org/diseases-conditions/thumb-arthritis/diagnosis-treatment/drc-20378344 (last accessed 14.4.2019)</ref> | |||
==== < | == Differential Diagnosis == | ||
The differential diagnosis of Rhizarthrosis includes: <ref name=":2" /> | |||
* [[De Quervain's Tenosynovitis|De Quervain's disease]] | |||
* [[Trigger Finger|Trigger thumb]] | |||
* Scaphoid fracture | |||
* Flexor Carpi Radialis (FCR) tenosynovitis | |||
* Scaphotrapezial arthritis | |||
* [[Wrist and Hand Osteoarthritis|Wrist arthritis]] | |||
* Subsesamoid arthritis | |||
== Treatment == | |||
Conservative measures are the first options for CMC arthritis and can ameliorate symptoms in most cases. These include | |||
< | === Behaviour modification === | ||
For example, try to avoid: clenching your hands when carrying things; repetitive movements that involve pinching or twisting | |||
=== Physiotherapy === | |||
Techniques include | |||
* range-of-motion and stretching exercises to improve thumb motion. | |||
{{#ev:youtube|https://www.youtube.com/watch?v=wCIA1_tksjA&feature=youtu.be|width}}<ref>Healing hands rehab. CMC arthritis. Available from: https://www.youtube.com/watch?v=wCIA1_tksjA&feature=youtu.be (last accessed 14.4.2019) </ref> | |||
* Advance to include strength exercise for the intrinsic and extrinsic muscles of the thumb and muscles of the fingers. | |||
{{#ev:youtube|https://www.youtube.com/watch?v=rf4R7udarNg&feature=youtu.be|width}}<ref>LB hand therapy. Thumb stability exercises. Available from: https://www.youtube.com/watch?v=rf4R7udarNg&feature=youtu.be</ref> | |||
* [[Dexterity Tests|Dexterity]] and fine motor exercises for the hand and thumb. <ref name=":0">Central physiotherapy. [https://www.centralphysicaltherapy.com/Injuries-Conditions/Hand/Hand-Issues/Arthritis-of-the-Thumb/a~282/article.html Arthritis of the thumb.] Available from: https://www.centralphysicaltherapy.com/Injuries-Conditions/Hand/Hand-Issues/Arthritis-of-the-Thumb/a~282/article.html (last accessed 14.4.2019)</ref> | |||
* Application of therapeutic [[Thermotherapy|heat]] or [[Cryotherapy|cold]] | |||
* Application of electrotherapeutic techniques, For example, Therapeutic Ultrasound, [[Transcutaneous Electrical Nerve Stimulation (TENS)|TENS]]. Ultrasound has been found to have the ability to evoke a broad range of therapeutically beneficial such as improved pain and functional [[Outcome Measures|outcome]]<nowiki/>s, positive [[cartilage]] healing properties, and positive phonophoresis for hyaluronan. <ref>Srbely JZ. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2258240/ Ultrasound in the management of osteoarthritis: part I: a review of the current literature.] The Journal of the Canadian Chiropractic Association. 2008 Mar;52(1):30. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2258240/ (last accessed 15.4.2019)</ref> | |||
* [[Acupuncture]]. May work in pain relief for some people.<ref>Arthritis Foundation. [https://www.arthritis.org/living-with-arthritis/treatments/natural/other-therapies/mind-body-pain-relief/oa-acupuncture.php Acupuncture and osteoarthritis.] Available from: https://www.arthritis.org/living-with-arthritis/treatments/natural/other-therapies/mind-body-pain-relief/oa-acupuncture.php (last accessed 15.4.2019)</ref> | |||
* Clinical trials have provided evidence that a combination of joint mobilization, [[Neurodynamics|neural mobilization,]] and exercise helps with CMC joint pain.<ref>Jospt. | |||
= | [https://www.jospt.org/doi/full/10.2519/jospt.2013.4524 The Effectiveness of a Manual Therapy and Exercise Protocol in Patients With Thumb Carpometacarpal Osteoarthritis: A Randomized Controlled Trial]. Available from: https://www.jospt.org/doi/full/10.2519/jospt.2013.4524 (last accessed 14.4.2019) | ||
</ref> | |||
* Splinting, designed to help reduce pain, prevent deformity, or prevent deformity from getting worse. To wear at night, during flare-ups, and when doing heavy work with hand.<ref name=":0" /> | |||
[[File:Rhizarthrosis splint.png|thumb|360x360px|Rhizarthrosis splint|center]] | |||
=== Pain relief === | |||
Options include | |||
* Topical medications, such as capsaicin or diclofenac, which are applied to the skin over the joint | |||
* Over-the-counter [[Pain Medications|pain relievers]], such as acetaminophen, ibuprofen or naproxen sodium | |||
* Prescription [[Pain Medications|pain relievers,]] such as celecoxib (Celebrex) or tramadol (Conzip, Ultram) | |||
* Injections. [[Therapeutic Corticosteroid Injection|Corticosteroid injections]] can offer temporary pain relief and reduce inflammation.<ref name=":1" /><sup></sup> | |||
=== Surgery === | |||
If the diagnosis of ‘rhizarthrosis’ is determined too late, none of the above treatments will be helpful. Because of severe pain and movement restriction, surgery could be inevitable. The following options are usually offered for surgery: <ref>Rhizarthrosis. Available from: | |||
http://www.baur-fromberg.de/rhizarthrosis.php (Accessed 19 October 2020) | |||
</ref> | |||
* Arthroscopy: resecting a part of the trapezium bone | |||
* Arthrodesis to fuse the first metacarpal bone and the trapezium bone | |||
* Arthroplasty to reconstruct the joint by the use of a prosthesis such as Swanson’s trapezium implant arthroplasty <ref>Ruettermann M. Changing surgical treatments of thumb carpometacarpal osteoarthritis. Journal of Hand Surgery (European Volume). 2020 Jun; 45(5):533-5. </ref> or the Artelon spacer. <ref>Gillis J, Calder K, Williams J. Review of thumb carpometacarpal arthritis classification, treatment and outcomes. Canadian Journal of Plastic Surgery. 2011 Dec; 19(4):134-8.</ref> | |||
Other treatment techniques may also include: <ref>Rhizarthrosis. Available from: https://www.topdoctors.co.uk/medical-dictionary/rhizarthrosis (Accessed 19 October 2020)</ref> | |||
* Denervation of the TMC joint | |||
* Reconstruction of the volar beak ligament | |||
* Suture button suspensionplasty | |||
{{#ev:youtube|https://www.youtube.com/watch?v=iSA1BSSQLPA|width}}<ref>Dartmouth-Hitchcock. Basal joint arthritis. Available from: https://www.youtube.com/watch?v=iSA1BSSQLPA (last accessed 15.4.2019)</ref> | |||
== '''Complications''' == | |||
Complications that may arise after surgery include:<ref name=":3" /> | |||
==== '''Common complications'''<sup></sup> ==== | |||
* Swelling | |||
* Bruising | |||
* Incision tenderness | |||
* Joint Stiffness | |||
* Mild metacarpal subsidence | |||
==== '''2. Uncommon Complications''' ==== | |||
* Hematoma | |||
* Infection | |||
* Nerve irritation/numbness | |||
* Recurrent pain | |||
* Tendon anchovy extrusion | |||
* Tendon adhesions or ruptures | |||
* [[Deep Vein Thrombosis|Deep vein thrombosis]] | |||
* [[Pulmonary Embolism|Pulmonary embolus]] | |||
* [[Myocardial Infarction|Myocardial infarction]] | |||
* Death | |||
* Mild metacarpal subsidence | |||
== References == | |||
<references /> | |||
[[Category:Hand - Conditions]] | |||
[[Category:Osteoarthritis]] | |||
[[Category:Rheumatology]] | |||
Latest revision as of 07:40, 3 September 2023
Introduction[edit | edit source]
Trapeziometacarpal (TMC) arthritis ( also known as Rhizarthrosis ) is arthritis of the first carpometacarpal (CMC) joint of the thumb. The CMC joint of the thumb, or TMC joint plays a critical role in the normal functioning of the thumb. It is the most important joint connecting the wrist to the metacarpus. Osteoarthritis of the TMC is a severely disabling condition; it is up to twenty times more common among elderly women than on average.[1]
Ligaments of the TMC Joint and their functions
The main ligaments of the TMC Joint are as follows: [2] [3] [4]
- The dorsoradial ligaments (DRL)
- The superficial anterior oblique ligament (AOL)
- The deep anterior oblique ligament (AOL)
- The intermetacarpal ligament (IML)
- The ulnar collateral ligament
- The posterior obique ligament
Table 1. The Functions of the ligaments (table adapted from Blige & Karalezli 2015 [2]
| Ligament | Function | |
|---|---|---|
| Dorsoradial | Shortest and thickest ligament. Primary stabilizers against dorsal translation of the joint | |
| Anterior oblique | Superficial | Stabilization against volar joint subluxation |
| Anterior oblique | Deep | It is also known as beak ligament. It acts as a pivot primary joint stabilizer against dorsal translation |
| Posterior oblique | Stabilization of rotation | |
| Intermetacarpal | Stabilization during radiovolar translation | |
| Ulnar collateral | Helps to stabilize against the volar joint subluxation |
Although there is a controversy about the primary stabilizers of the TMC Joint, several studies concluded the DRL to be the primary stabilizers [5] [3]
Stages of CMC[edit | edit source]
The CMC stages are usually classified according to the Eaton-Litter Classification which is obtained through radiological procedures or arthroscopy [2]. It's a staging protocol with four different stages based on synovitis, joint space, and the laxity of the capsule [7].
Here are the four stages of Eaton-Litter Classification [8]:
Stage I: Synovitis Phase
- Articular contours are normal
- Possible widening of TMC joint that suggests joint effusion or ligament laxity
- No osteophyte formation
Stage II: Significant Capsular Laxity
- Narrowing of CMC joint
- Small osteophyte formation at the ulnar side of the distal trapezial articular surface
- No or 1/3rd CMC joint subluxation
Stage III: Significant Joint Destruction
- Further joint space narrowing with cystic changes and sclerotic bone
- Prominent osteophytes at the ulnar border of distal trapezium
- Moderate subluxation radially and dorsally at the base of the first metacarpal
- Mild arthrosis of the scaphotrapezial joint
Stage IV: Pantrapezial Arthritis
- Major subluxation of the joint
- Narrowing of the joint space as in stage 3
- Cystic and sclerotic subchondral bone changes
- Significant erosion and destruction of scaphotrapezial joint
<section> Stage 2: Significant Capsular Laxity
- Narrowing of CMC Joint
- Mild Subchondral sclerotic changes
- Small ( < 2mm) osteophyte formation commonly at the distal trapezial articular surface
- No or < 1/3 CMC joint sbluxation in any projection
</section>
Etiology[edit | edit source]
Causes of TMC arthritis are:
- Excessive repetitive use of the CMC joint of the thumb
- Subluxation
- Lesion of the ligaments or a fracture.
- Laxity of the CMC joint can be hereditary, increased risk for ligament injuries, a primary stimulus in the development of arthritis. Also causes hyperextension, which is another primary stimulus for the development of arthritis.[9]
- Weakness of the cross links of the fingers (ligament oblique anterior). These ligaments are the most important stabilizers of the fingers. [10]
- Using thumb in occupation, For example, Work-related thumb pain in physiotherapists is a prevalent problem among physiotherapists who administer manual techniques. Factors that appear to be associated with thumb pain include CMC mobility and thumb strength[11].
Signs and Symptoms[edit | edit source]
The first signs of arthritis in the thumb are
- pain, tenderness, and stiffness at the base of your thumb. This occurs with gripping, pinching, or clasping something between the thumb and index fingers or when a mild force, such as when you twist a key in a lock or turn a door handle. An ache after activity can also be a feature.
- Decreased strength and range of motion, For example, opening jars or doing up buttons may become difficult.
- Appearance. The joint may become swollen or develop a bony bump. The joint may appear squarish and enlarged.[12]
Diagnosis[edit | edit source]
- Medical and family history
- Noticeable lumps or swelling on the first CMC joint
- Thumb CMC grind test
- Plain radiographs showing degenerative changes (bone spurs, thinning of cartilage, loss of joint space) in affected joints are usually diagnostic.[13]
Differential Diagnosis[edit | edit source]
The differential diagnosis of Rhizarthrosis includes: [2]
- De Quervain's disease
- Trigger thumb
- Scaphoid fracture
- Flexor Carpi Radialis (FCR) tenosynovitis
- Scaphotrapezial arthritis
- Wrist arthritis
- Subsesamoid arthritis
Treatment[edit | edit source]
Conservative measures are the first options for CMC arthritis and can ameliorate symptoms in most cases. These include
Behaviour modification[edit | edit source]
For example, try to avoid: clenching your hands when carrying things; repetitive movements that involve pinching or twisting
Physiotherapy[edit | edit source]
Techniques include
- range-of-motion and stretching exercises to improve thumb motion.
- Advance to include strength exercise for the intrinsic and extrinsic muscles of the thumb and muscles of the fingers.
- Dexterity and fine motor exercises for the hand and thumb. [16]
- Application of therapeutic heat or cold
- Application of electrotherapeutic techniques, For example, Therapeutic Ultrasound, TENS. Ultrasound has been found to have the ability to evoke a broad range of therapeutically beneficial such as improved pain and functional outcomes, positive cartilage healing properties, and positive phonophoresis for hyaluronan. [17]
- Acupuncture. May work in pain relief for some people.[18]
- Clinical trials have provided evidence that a combination of joint mobilization, neural mobilization, and exercise helps with CMC joint pain.[19]
- Splinting, designed to help reduce pain, prevent deformity, or prevent deformity from getting worse. To wear at night, during flare-ups, and when doing heavy work with hand.[16]
Pain relief[edit | edit source]
Options include
- Topical medications, such as capsaicin or diclofenac, which are applied to the skin over the joint
- Over-the-counter pain relievers, such as acetaminophen, ibuprofen or naproxen sodium
- Prescription pain relievers, such as celecoxib (Celebrex) or tramadol (Conzip, Ultram)
- Injections. Corticosteroid injections can offer temporary pain relief and reduce inflammation.[13]
Surgery[edit | edit source]
If the diagnosis of ‘rhizarthrosis’ is determined too late, none of the above treatments will be helpful. Because of severe pain and movement restriction, surgery could be inevitable. The following options are usually offered for surgery: [20]
- Arthroscopy: resecting a part of the trapezium bone
- Arthrodesis to fuse the first metacarpal bone and the trapezium bone
- Arthroplasty to reconstruct the joint by the use of a prosthesis such as Swanson’s trapezium implant arthroplasty [21] or the Artelon spacer. [22]
Other treatment techniques may also include: [23]
- Denervation of the TMC joint
- Reconstruction of the volar beak ligament
- Suture button suspensionplasty
Complications[edit | edit source]
Complications that may arise after surgery include:[8]
Common complications[edit | edit source]
- Swelling
- Bruising
- Incision tenderness
- Joint Stiffness
- Mild metacarpal subsidence
2. Uncommon Complications[edit | edit source]
- Hematoma
- Infection
- Nerve irritation/numbness
- Recurrent pain
- Tendon anchovy extrusion
- Tendon adhesions or ruptures
- Deep vein thrombosis
- Pulmonary embolus
- Myocardial infarction
- Death
- Mild metacarpal subsidence
References[edit | edit source]
- ↑ Wikipedia. CMC joint. Accessed 30.09.22
- ↑ 2.0 2.1 2.2 2.3 Bilge O, Karalezli N. Current review of trapeziometacarpal osteoarthritis (rhizarthrosis). World Journal of Rheumatology. 2015 Jul 12; 5(2):90-5. Accessed 30.09.22
- ↑ 3.0 3.1 Lin JD, Karl JW, Strauch RJ. Trapeziometacarpal joint stability: the evolving importance of the dorsal ligaments. Clinical Orthopaedics and Related Research®. 2014 Apr 1; 472(4):1138-45. Accessed 30.09.22.
- ↑ Imaeda T, An KN, Cooney III WP, Linscheid R. Anatomy of trapeziometacarpal ligaments. The Journal of hand surgery. 1993 Mar 1; 18(2):226-31. Accessed 30.09.22.
- ↑ Ripoll G, Glumcher D, Fossati G 2019 Anatomical considerations of the thumb carpometacarpal joint ligaments, based on a case report of isolated joint dislocation (Accessed 30.09.22)
- ↑ Mayo clinic. Causes remedies for thumb arthritis. Accessed 30.09.22
- ↑ Wikipedia. Trapeziometacarpal osteoarthritis. [Accessed, 30.09.22]
- ↑ 8.0 8.1 Thumb CMC Joint Arthroplasty. Available from:https://www.touchsurgery.com/simulations/thumb-cmc-joint-arthroplasty (Accessed 15 October 2020)
- ↑ Wolf JM, Schreier S, Tomsick S, Williams A, Petersen B. Radiographic laxity of the trapeziometacarpal joint is correlated with generalized joint hypermobility. The Journal of hand surgery. 2011 Jul 1;36(7):1165-9. Available from: https://www.jhandsurg.org/article/S0363-5023(11)00353-4/abstract (last accessed 14.4.2019)
- ↑ A. Gondim Teixeira, Pedro & Omoumi, Patrick & J Trudell, Debra & Ward, Samuel & Blum, Alain & L Resnick, Donald. (2010). High-resolution ultrasound evaluation of the trapeziometacarpal joint with emphasis on the anterior oblique ligament (beak ligament). Skeletal radiology. 40. 897-904. 10.1007/s00256-010-1068-0. Available from: https://www.researchgate.net/publication/49647832_High-resolution_ultrasound_evaluation_of_the_trapeziometacarpal_joint_with_emphasis_on_the_anterior_oblique_ligament_beak_ligament
- ↑ Snodgrass SJ, Riyett DA, Chiarelli P, Bates AM, Rowe LJ. Factors related to thumb pain in physiotherapists. Australian Journal of Physiotherapy. 2003 Jan 1;49(4):243-50. Available from:https://www.sciencedirect.com/science/article/pii/S0004951414601409 (last accessed 10.4.2020)
- ↑ Healthline. Basal joint arthritis. Available from: https://www.healthline.com/health/basal-joint-arthritis#symptoms (last accessed 14.4.2019)
- ↑ 13.0 13.1 Mayo clinic. Thumb arthritis. Available from: https://www.mayoclinic.org/diseases-conditions/thumb-arthritis/diagnosis-treatment/drc-20378344 (last accessed 14.4.2019)
- ↑ Healing hands rehab. CMC arthritis. Available from: https://www.youtube.com/watch?v=wCIA1_tksjA&feature=youtu.be (last accessed 14.4.2019)
- ↑ LB hand therapy. Thumb stability exercises. Available from: https://www.youtube.com/watch?v=rf4R7udarNg&feature=youtu.be
- ↑ 16.0 16.1 Central physiotherapy. Arthritis of the thumb. Available from: https://www.centralphysicaltherapy.com/Injuries-Conditions/Hand/Hand-Issues/Arthritis-of-the-Thumb/a~282/article.html (last accessed 14.4.2019)
- ↑ Srbely JZ. Ultrasound in the management of osteoarthritis: part I: a review of the current literature. The Journal of the Canadian Chiropractic Association. 2008 Mar;52(1):30. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2258240/ (last accessed 15.4.2019)
- ↑ Arthritis Foundation. Acupuncture and osteoarthritis. Available from: https://www.arthritis.org/living-with-arthritis/treatments/natural/other-therapies/mind-body-pain-relief/oa-acupuncture.php (last accessed 15.4.2019)
- ↑ Jospt. The Effectiveness of a Manual Therapy and Exercise Protocol in Patients With Thumb Carpometacarpal Osteoarthritis: A Randomized Controlled Trial. Available from: https://www.jospt.org/doi/full/10.2519/jospt.2013.4524 (last accessed 14.4.2019)
- ↑ Rhizarthrosis. Available from: http://www.baur-fromberg.de/rhizarthrosis.php (Accessed 19 October 2020)
- ↑ Ruettermann M. Changing surgical treatments of thumb carpometacarpal osteoarthritis. Journal of Hand Surgery (European Volume). 2020 Jun; 45(5):533-5.
- ↑ Gillis J, Calder K, Williams J. Review of thumb carpometacarpal arthritis classification, treatment and outcomes. Canadian Journal of Plastic Surgery. 2011 Dec; 19(4):134-8.
- ↑ Rhizarthrosis. Available from: https://www.topdoctors.co.uk/medical-dictionary/rhizarthrosis (Accessed 19 October 2020)
- ↑ Dartmouth-Hitchcock. Basal joint arthritis. Available from: https://www.youtube.com/watch?v=iSA1BSSQLPA (last accessed 15.4.2019)