Back and Upper Leg Regional Pain and Gait Deviations: Difference between revisions
No edit summary |
(added three updated references) |
||
| (24 intermediate revisions by 5 users not shown) | |||
| Line 4: | Line 4: | ||
== Introduction == | == Introduction == | ||
Gait deviations are likely related to the development of and / or associated with musculoskeletal pain syndromes. It is often the complaint of pain that will lead a patient to physiotherapy. It is the role of the physiotherapist to educate the patient on the aetiology of their pain while treating and correcting the noted gait deviation.<ref name=":0">Howell, D, Back and Upper Leg Regional Pain and Gait Deviations. Gait Analysis. | Gait deviations are likely related to the development of and / or associated with musculoskeletal pain syndromes. It is often the complaint of pain that will lead a patient to physiotherapy. It is the role of the physiotherapist to educate the patient on the aetiology of their pain while treating and correcting the noted gait deviation.<ref name=":0">Howell, D, Back and Upper Leg Regional Pain and Gait Deviations. Gait Analysis. Plus. 2022</ref><blockquote>"The '''kinesiopathologic model''' was designed specifically to describe the mechanically related processes proposed to contribute to the development and course of low back pain (LBP). The basic premise is that LBP results from the repeated use of direction-specific (flexion, extension, rotation, lateral bending, or a combination of these) stereotypic movement and alignment patterns in the lumbar spine. The model proposes that the patterns begin as the result of adaptations of the musculoskeletal and neural systems due to repeated use of specific movements and alignments during daily activities. The nature and rate of the adaptations can be modified by intrinsic and extrinsic characteristics of the individual, for example, sex, anthropometrics, or typical activities of the person. The typical pattern is one in which, during performance of a movement (eg, forward bending) or assumption of a posture (eg, sitting), the lumbar spine moves into its available range in a specific direction more readily than other joints, such as the knees, hips, or thoracic spine."<ref>Cholewicki J, Breen A, Popovich Jr JM, Reeves NP, Sahrmann SA, Van Dillen LR, Vleeming A, Hodges PW. [https://www.jospt.org/doi/pdf/10.2519/jospt.2019.8825 Can biomechanics research lead to more effective treatment of low back pain? A point-counterpoint debate]. journal of orthopaedic & sports physical therapy. 2019 Jun;49(6):425-36.</ref> </blockquote> | ||
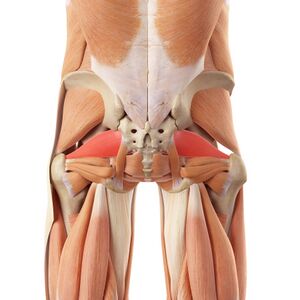
[[File:Posterior muscles of back and hips, piriformis.jpeg|thumb|Note the interconnected nature of the | [[File:Posterior muscles of back and hips, piriformis.jpeg|thumb|Note the interconnected nature of the back, posterior hip and upper leg musculature.]] | ||
With the patient's pain as a guide, a goal of musculoskeletal physiotherapy is to identify the anatomical structures associated with the reported pain. | With the patient's pain as a guide, a goal of musculoskeletal physiotherapy is to identify the anatomical structures associated with the reported pain. Physiotherapists utilise orthopaedic tests to assist in symptom source identification. However, these clinical tests are often inconsistent in their ability to accurately identify the anatomical source of the patient's symptoms. Additionally, there is a poor correlation between imaging results and symptom source identification in the absence of trauma or pathology. These two statements suggest that musculoskeletal pain may often be anatomically and structurally indeterminable. The kinesiopathological approach is an alternative to these more traditional methods of diagnosis. This method calls for clinical practice to be guided by the identification and modification of kinematic or motor control impairments within a musculoskeletal function.<ref>Tabatabaei Molazi F, Mahdian SR, Rajabi R, Karimizadeh Ardakani M. [http://ijmpp.modares.ac.ir/files/ijmpp/user_files_749497/fatemehtabatabaei-A-10-70089-1-ed9ced7.pdf Reliability of Corrective Exercise Specialist Raters Assessing Movement System Impairment Approach Items in Transient Low Back Pain Developers During Prolonged Standing]. International Journal of Musculoskeletal Pain Prevention. 2022 Jul 10;7(3):750-8.</ref> By correcting deviant movement patterns to a more idealised movement pattern unique to a particular individual, subjective pain can be improved and function can be reestablished.<ref>Lehman GJ. [https://www.jospt.org/doi/pdf/10.2519/jospt.2018.0608 The role and value of symptom-modification approaches in musculoskeletal practice]. journal of orthopaedic & sports physical therapy. 2018 Jun;48(6):430-5.</ref> | ||
== Back Regional Pain == | == Back Regional Pain == | ||
| Line 14: | Line 14: | ||
# Shortened step length<ref name=":1" /> | # Shortened step length<ref name=":1" /> | ||
# Slow gait cadence | # Slow gait cadence | ||
# Stiff counter rotation between the thoracic spine and the lumbar spine<ref name=":1" /> | # Stiff counter-rotation between the thoracic spine and the lumbar spine<ref name=":1" /> | ||
# Changes in expected vertical oscillation of centre of mass (COM) | # Changes in expected vertical oscillation of centre of mass (COM) | ||
# Loud foot strike | # Loud foot strike | ||
# Can demonstrate either an increased or decreased pelvic tilt | # Can demonstrate either an increased or decreased [[Pelvic Tilt|pelvic tilt]] | ||
# Can demonstrate either increased or decreased hip extension during terminal stance | # Can demonstrate either increased or decreased hip extension during terminal stance | ||
# Decrease in big toe dorsiflexion, resulting in a functional hallux limitus | # Decrease in big toe dorsiflexion, resulting in a functional [[Hallux Rigidus|hallux limitus]] | ||
</blockquote> | </blockquote> | ||
| Line 31: | Line 31: | ||
|'''Hip Region''' | |'''Hip Region''' | ||
| | | | ||
* Osteoarthritis<ref name=":2">Harris-Hayes M, Steger-May K, Bove AM, Foster SN, Mueller MJ, Clohisy JC, Fitzgerald GK. [https://bmjopensem.bmj.com/content/bmjosem/6/1/e000707.full.pdf Movement pattern training compared with standard strengthening and flexibility among patients with hip-related groin pain: results of a pilot multicentre randomised clinical trial]. BMJ open sport & exercise medicine. 2020 Mar 1;6(1):e000707.</ref><ref>Harris-Hayes M, Czuppon S, Van Dillen LR, Steger-May K, Sahrmann S, Schootman M, Salsich GB, Clohisy JC, Mueller MJ. [https://www.jospt.org/doi/full/10.2519/jospt.2016.6279 Movement-pattern training to improve function in people with chronic hip joint pain: a feasibility randomized clinical tria]l. journal of orthopaedic & sports physical therapy. 2016 Jun;46(6):452-61.</ref> | * [[Osteoarthritis]]<ref name=":2">Harris-Hayes M, Steger-May K, Bove AM, Foster SN, Mueller MJ, Clohisy JC, Fitzgerald GK. [https://bmjopensem.bmj.com/content/bmjosem/6/1/e000707.full.pdf Movement pattern training compared with standard strengthening and flexibility among patients with hip-related groin pain: results of a pilot multicentre randomised clinical trial]. BMJ open sport & exercise medicine. 2020 Mar 1;6(1):e000707.</ref><ref>Harris-Hayes M, Czuppon S, Van Dillen LR, Steger-May K, Sahrmann S, Schootman M, Salsich GB, Clohisy JC, Mueller MJ. [https://www.jospt.org/doi/full/10.2519/jospt.2016.6279 Movement-pattern training to improve function in people with chronic hip joint pain: a feasibility randomized clinical tria]l. journal of orthopaedic & sports physical therapy. 2016 Jun;46(6):452-61.</ref> | ||
* Can continue status post total joint | * Can continue status post-[[Total Hip Replacement|total joint arthroplasty]] | ||
| | | | ||
* Decreased cadence | * Decreased cadence | ||
| Line 49: | Line 49: | ||
|'''Lateral Hip''' | |'''Lateral Hip''' | ||
| | | | ||
* Gluteal tendinopathy | * [[Gluteal Tendinopathy|Gluteal tendinopathy]] | ||
* Piriformis syndrome | * [[Piriformis Syndrome|Piriformis syndrome]] | ||
* Complaint of "buttock pain" | * Complaint of "buttock pain" | ||
| | | | ||
| Line 67: | Line 67: | ||
|'''Anterior Hip''' | |'''Anterior Hip''' | ||
| | | | ||
* Femoroacetabular impingement (FAI) syndrome<ref name=":2" /><ref>Ranawat AS, Gaudiani MA, Slullitel PA, Satalich J, Rebolledo BJ. [https://scholar.google.com/scholar?output=instlink&q=info:eFiXQn7dw4MJ:scholar.google.com/&hl=en&as_sdt=0,44&scillfp=16151773003627380027&oi=lle Foot progression angle walking test: a dynamic diagnostic assessment for femoroacetabular impingement and hip instability]. Orthopaedic Journal of Sports Medicine. 2017 Jan 10;5(1):2325967116679641.</ref> | * [[Femoroacetabular Impingement|Femoroacetabular impingement (FAI) syndrome]]<ref name=":2" /><ref>Ranawat AS, Gaudiani MA, Slullitel PA, Satalich J, Rebolledo BJ. [https://scholar.google.com/scholar?output=instlink&q=info:eFiXQn7dw4MJ:scholar.google.com/&hl=en&as_sdt=0,44&scillfp=16151773003627380027&oi=lle Foot progression angle walking test: a dynamic diagnostic assessment for femoroacetabular impingement and hip instability]. Orthopaedic Journal of Sports Medicine. 2017 Jan 10;5(1):2325967116679641.</ref> | ||
* Acetabular labral tear<ref name=":2" /> | * Acetabular labral tear<ref name=":2" /> | ||
* Status post repair of the acetabular labrum | * Status post repair of the acetabular labrum | ||
| Line 75: | Line 75: | ||
|} | |} | ||
== Knee | == Knee Regional Pain == | ||
{| class="wikitable" | {| class="wikitable" | ||
|+ | |+ | ||
| Line 85: | Line 85: | ||
| | | | ||
* Osteoarthritis | * Osteoarthritis | ||
* Can continue status post total joint | * Can continue status post-total joint arthroplasty | ||
| | | | ||
* Increased lateral trunk lean | * Increased lateral trunk lean | ||
| Line 94: | Line 94: | ||
|- | |- | ||
|'''Anterior Knee''' | |'''Anterior Knee''' | ||
|Patellofemoral arthralgia | |[[Patellofemoral Pain Syndrome|Patellofemoral arthralgia]] | ||
| | | | ||
* Too long a step | * Too long a step | ||
| Line 107: | Line 107: | ||
|- | |- | ||
|'''Lateral Knee''' | |'''Lateral Knee''' | ||
|Iliotibial (IT) band syndrome | |[[Iliotibial Band Syndrome|Iliotibial (IT) band syndrome]] | ||
| | | | ||
* Too long a step | * Too long a step | ||
| Line 114: | Line 114: | ||
* Increased knee extension at foot strike or heel rocker | * Increased knee extension at foot strike or heel rocker | ||
* Loud foot strike | * Loud foot strike | ||
* Insufficient daylight | * Insufficient daylight or insufficient separation between the knees | ||
* Foot crossing the midline | * Foot crossing the midline | ||
* Oblique popliteal skin crease (excessive medial femoral rotation) | * Oblique popliteal skin crease (excessive medial femoral rotation) | ||
| Line 124: | Line 124: | ||
== Back and Upper Leg Region Special Topics == | == Back and Upper Leg Region Special Topics == | ||
=== Lumbar Stenosis Gait Deviation === | |||
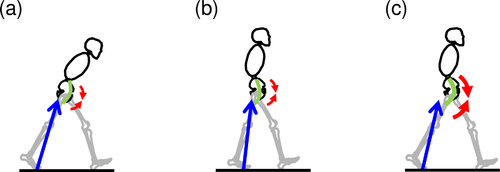
[[Lumbar Spinal Stenosis|Lumbar stenosis]] is a common back pain diagnosis in the elderly population. A patient with lumbar stenosis does not stand or ambulate with upright posture, and tends to avoid lumbar extension to decrease and / or avoid pain.<ref>Nüesch C, Mandelli F, Przybilla P, Schären S, Mündermann A, Netzer C. [https://www.sciencedirect.com/science/article/pii/S0966636222006191 Kinematics and paraspinal muscle activation patterns during walking differ between patients with lumbar spinal stenosis and controls]. Gait & Posture. 2023 Jan 1;99:44-50.</ref> They may present with a tendency to walk bent over, and lean on their grocery cart or walker. They will likely demonstrate one of two gait deviations to alleviate symptoms associated with lumbar spinal stenosis:<ref name=":3">Igawa T, Katsuhira J, Hosaka A, Uchikoshi K, Ishihara S, Matsudaira K. [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0197228 Kinetic and kinematic variables affecting trunk flexion during level walking in patients with lumbar spinal stenosis]. PLoS One. 2018 May 10;13(5):e0197228.</ref> | |||
#Figure A: Trunk flexion posture with an increased step length and hip extension angle,<ref name=":3" /> and an absent lumbar joint moment into extension.<ref name=":0" /> | |||
#Figure B: Trunk upright posture with a decreased step length and hip extension angle,<ref name=":3" /> and an absent lumbar joint moment into extension.<ref name=":0" /> | |||
#Figure C: Ideal walking posture of healthy people<ref name=":3" />[[File:Lumbar stenosis gait deviation.png|alt=|thumb|500x500px|Blue arrows indicate the ground reaction force vector, red arrow is the hip flexion moment, and green arc is the psoas major. |center]] | |||
=== Dropped Head Syndrome === | |||
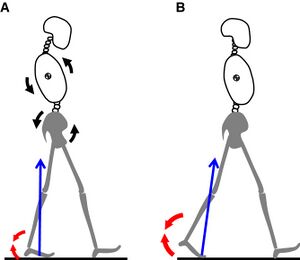
Dropped head syndrome (DHS) is a relatively rare cervical kyphotic deformity with symptoms that include: neck pain, restrictions to ambulation, and impaired horizontal gaze.<ref>Igawa T, Ishii K, Urata R, Suzuki A, Ui H, Ideura K, Isogai N, Sasao Y, Funao H. [https://www.mdpi.com/1648-9144/58/4/465/pdf Association between the Horizontal Gaze Ability and Physical Characteristics of Patients with Dropped Head Syndrome]. Medicina. 2022 Mar 23;58(4):465.</ref> Due to the interconnected nature of the spine, the relationship between cervical alignment and other parts of the spinal column can have an effect on the pelvis and lower limbs during dynamic activities. Patients with DHS demonstrate altered kinematics and kinematics of the lower limbs during walking due to changes in the inclination of the head and trunk. This may cause deviant gait features and altered motor control compared to healthy individuals. Similar findings have been reported in individuals using smartphones while walking. The increased cervical flexion angle affects: cervical loading, walking speed, and muscle activity of the lower limbs.<ref name=":4">Igawa T, Ishii K, Suzuki A, Ui H, Urata R, Isogai N, Sasao Y, Nishiyama M, Funao H. [https://www.nature.com/articles/s41598-021-97329-w Dynamic alignment changes during level walking in patients with dropped head syndrome: Analyses using a three-dimensional motion analysis system]. Scientific reports. 2021 Sep 14;11(1):1-0.</ref> | |||
# Figure A represents an individual with DHS: backward leaning posture of the thorax, increased ankle-joint dorsiflexion angle, and relatively shorter stride length. <ref name=":4" /> | |||
# Figure B is ideal walking posture: upright erect posture with decreased ankle dorsiflexion angle allowing for more movement coming from the ankle to propel forward and up. <ref name=":4" /> | |||
[[File:Dropped head posture.jpeg|alt=|thumb|Black arrows indicate the backward tilted thorax and pelvis. Blue arrows are the ground reaction force vector. Red arrow is the ankle plantarflexion moment.|center]] | |||
=== Geriatric gait === | |||
At self-selected walking speeds, elderly adults generate decreased joint torques and power in their lower extremities than young adults. These differences are due to the biomechanical and physiological consequences of aging resulting from changes in the underlying neuromuscular components of motor performance and reduction in motor abilities.<ref name=":5">DeVita P, Hortobagyi T. [https://scholar.google.com/scholar?output=instlink&q=info:sEC0gJIDE2EJ:scholar.google.com/&hl=en&as_sdt=0,44&scillfp=10103153512704345450&oi=lle Age causes a redistribution of joint torques and powers during gait]. Journal of applied physiology. 2000 May 1;88(5):1804-11.</ref> Pain may also be a factor.<ref name=":0" /><blockquote>'''The spatiotemporal changes that occur in geriatric gait:'''<ref name=":0" /> | |||
# Decreased walking speed, less than 1-1.4 metres per second | |||
# Shorter step length | |||
# Slower gait cadence | |||
# Late or a prolonged heel contact | |||
# Decreased vertical oscillation of COM | |||
# Could have decreased hip extension | |||
# Could have increased forward trunk flexion | |||
# Could have decreased arm swing | |||
# Elderly people tend to use hip joint moments more than ankle moments, whereas young people use the ankle to propel forward<ref name=":5" /> | |||
</blockquote> | |||
=== Osteoarthritis and Total Joint Replacements === | |||
Oftentimes patients with knee or hip osteoarthritis develop gait deviations which continue due to "habit" after undergoing total joint replacements.<ref name=":0" /> Patients who undergo post-operative rehabilitation report improved joint pain and stiffness but commonly demonstrate incomplete recovery of gait function.<ref>Bączkowicz D, Skiba G, Czerner M, Majorczyk E. Gait and functional status analysis before and after total knee arthroplasty. The Knee. 2018 Oct 1;25(5):888-96.</ref> | |||
== Resources == | == Resources == | ||
| Line 133: | Line 157: | ||
*Harris-Hayes M, Czuppon S, Van Dillen LR, Steger-May K, Sahrmann S, Schootman M, Salsich GB, Clohisy JC, Mueller MJ. [https://scholar.google.com/scholar?output=instlink&q=info:lmbr9GuHh5YJ:scholar.google.com/&hl=en&as_sdt=0,44&scillfp=10556444198263071018&oi=lle Movement-pattern training to improve function in people with chronic hip joint pain: a feasibility randomized clinical trial]. journal of orthopaedic & sports physical therapy. 2016 Jun;46(6):452-61. | *Harris-Hayes M, Czuppon S, Van Dillen LR, Steger-May K, Sahrmann S, Schootman M, Salsich GB, Clohisy JC, Mueller MJ. [https://scholar.google.com/scholar?output=instlink&q=info:lmbr9GuHh5YJ:scholar.google.com/&hl=en&as_sdt=0,44&scillfp=10556444198263071018&oi=lle Movement-pattern training to improve function in people with chronic hip joint pain: a feasibility randomized clinical trial]. journal of orthopaedic & sports physical therapy. 2016 Jun;46(6):452-61. | ||
*Harris-Hayes M, Steger-May K, Bove AM, Foster SN, Mueller MJ, Clohisy JC, Fitzgerald GK. [https://scholar.google.com/scholar?output=instlink&q=info:OgubXlaNkrQJ:scholar.google.com/&hl=en&as_sdt=0,44&scillfp=17838916680716325201&oi=lle Movement pattern training compared with standard strengthening and flexibility among patients with hip-related groin pain: results of a pilot multicentre randomised clinical trial]. BMJ open sport & exercise medicine. 2020 Mar 1;6(1):e000707. | *Harris-Hayes M, Steger-May K, Bove AM, Foster SN, Mueller MJ, Clohisy JC, Fitzgerald GK. [https://scholar.google.com/scholar?output=instlink&q=info:OgubXlaNkrQJ:scholar.google.com/&hl=en&as_sdt=0,44&scillfp=17838916680716325201&oi=lle Movement pattern training compared with standard strengthening and flexibility among patients with hip-related groin pain: results of a pilot multicentre randomised clinical trial]. BMJ open sport & exercise medicine. 2020 Mar 1;6(1):e000707. | ||
*Igawa T, Katsuhira J, Hosaka A, Uchikoshi K, Ishihara S, Matsudaira K. [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0197228 Kinetic and kinematic variables affecting trunk flexion during level walking in patients with lumbar spinal stenosis]. PLoS One. 2018 May 10;13(5):e0197228. | |||
*Igawa T, Ishii K, Suzuki A, Ui H, Urata R, Isogai N, Sasao Y, Nishiyama M, Funao H. [https://www.nature.com/articles/s41598-021-97329-w Dynamic alignment changes during level walking in patients with dropped head syndrome: Analyses using a three-dimensional motion analysis system]. Scientific reports. 2021 Sep 14;11(1):1-0. | |||
*Lamoth CJ, Meijer OG, Daffertshofer A, Wuisman PI, Beek PJ. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3454567/ Effects of chronic low back pain on trunk coordination and back muscle activity during walking: changes in motor control]. European Spine Journal. 2006 Feb;15(1):23-40. | *Lamoth CJ, Meijer OG, Daffertshofer A, Wuisman PI, Beek PJ. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3454567/ Effects of chronic low back pain on trunk coordination and back muscle activity during walking: changes in motor control]. European Spine Journal. 2006 Feb;15(1):23-40. | ||
| Line 138: | Line 164: | ||
'''Clinical Outcome Measures:''' | '''Clinical Outcome Measures:''' | ||
* [[Hip Disability | * [[Hip Disability and Osteoarthritis Outcome Score]] (HOOS) [http://www.koos.nu/HOOSEng.pdf Download PDF here] | ||
* Please view the following short video for an overview of the [[FABER Test|FABER test]] used in the assessment of pathologies at the hip, lumbar and sacroiliac region. | * Please view the following short video for an overview of the [[FABER Test|FABER test]] used in the assessment of pathologies at the hip, lumbar and sacroiliac region. | ||
| Line 146: | Line 172: | ||
<references /> | <references /> | ||
[[Category:Plus Content]] | |||
[[Category:Course Pages]] | |||
Latest revision as of 04:54, 30 January 2023
Top Contributors - Stacy Schiurring, Kim Jackson, Jess Bell, Lucinda hampton and Nupur Smit Shah
Introduction[edit | edit source]
Gait deviations are likely related to the development of and / or associated with musculoskeletal pain syndromes. It is often the complaint of pain that will lead a patient to physiotherapy. It is the role of the physiotherapist to educate the patient on the aetiology of their pain while treating and correcting the noted gait deviation.[1]
"The kinesiopathologic model was designed specifically to describe the mechanically related processes proposed to contribute to the development and course of low back pain (LBP). The basic premise is that LBP results from the repeated use of direction-specific (flexion, extension, rotation, lateral bending, or a combination of these) stereotypic movement and alignment patterns in the lumbar spine. The model proposes that the patterns begin as the result of adaptations of the musculoskeletal and neural systems due to repeated use of specific movements and alignments during daily activities. The nature and rate of the adaptations can be modified by intrinsic and extrinsic characteristics of the individual, for example, sex, anthropometrics, or typical activities of the person. The typical pattern is one in which, during performance of a movement (eg, forward bending) or assumption of a posture (eg, sitting), the lumbar spine moves into its available range in a specific direction more readily than other joints, such as the knees, hips, or thoracic spine."[2]
With the patient's pain as a guide, a goal of musculoskeletal physiotherapy is to identify the anatomical structures associated with the reported pain. Physiotherapists utilise orthopaedic tests to assist in symptom source identification. However, these clinical tests are often inconsistent in their ability to accurately identify the anatomical source of the patient's symptoms. Additionally, there is a poor correlation between imaging results and symptom source identification in the absence of trauma or pathology. These two statements suggest that musculoskeletal pain may often be anatomically and structurally indeterminable. The kinesiopathological approach is an alternative to these more traditional methods of diagnosis. This method calls for clinical practice to be guided by the identification and modification of kinematic or motor control impairments within a musculoskeletal function.[3] By correcting deviant movement patterns to a more idealised movement pattern unique to a particular individual, subjective pain can be improved and function can be reestablished.[4]
Back Regional Pain[edit | edit source]
Potential gait deviations associated with LBP:[1]
- Decreased gait velocity, less than 1-1.4 metres per second[5]
- Shortened step length[5]
- Slow gait cadence
- Stiff counter-rotation between the thoracic spine and the lumbar spine[5]
- Changes in expected vertical oscillation of centre of mass (COM)
- Loud foot strike
- Can demonstrate either an increased or decreased pelvic tilt
- Can demonstrate either increased or decreased hip extension during terminal stance
- Decrease in big toe dorsiflexion, resulting in a functional hallux limitus
Hip Regional Pain[edit | edit source]
| Region of Pain | Relavent Diagnoses | Expected Gait Deviations |
|---|---|---|
| Hip Region |
|
|
| Lateral Hip |
|
|
| Anterior Hip |
|
Knee Regional Pain[edit | edit source]
| Region of Pain | Relavent Diagnoses | Expected Gait Deviations |
|---|---|---|
| Knee Region |
|
|
| Anterior Knee | Patellofemoral arthralgia |
|
| Lateral Knee | Iliotibial (IT) band syndrome |
|
Back and Upper Leg Region Special Topics[edit | edit source]
Lumbar Stenosis Gait Deviation[edit | edit source]
Lumbar stenosis is a common back pain diagnosis in the elderly population. A patient with lumbar stenosis does not stand or ambulate with upright posture, and tends to avoid lumbar extension to decrease and / or avoid pain.[10] They may present with a tendency to walk bent over, and lean on their grocery cart or walker. They will likely demonstrate one of two gait deviations to alleviate symptoms associated with lumbar spinal stenosis:[11]
- Figure A: Trunk flexion posture with an increased step length and hip extension angle,[11] and an absent lumbar joint moment into extension.[1]
- Figure B: Trunk upright posture with a decreased step length and hip extension angle,[11] and an absent lumbar joint moment into extension.[1]
- Figure C: Ideal walking posture of healthy people[11]
Dropped Head Syndrome[edit | edit source]
Dropped head syndrome (DHS) is a relatively rare cervical kyphotic deformity with symptoms that include: neck pain, restrictions to ambulation, and impaired horizontal gaze.[12] Due to the interconnected nature of the spine, the relationship between cervical alignment and other parts of the spinal column can have an effect on the pelvis and lower limbs during dynamic activities. Patients with DHS demonstrate altered kinematics and kinematics of the lower limbs during walking due to changes in the inclination of the head and trunk. This may cause deviant gait features and altered motor control compared to healthy individuals. Similar findings have been reported in individuals using smartphones while walking. The increased cervical flexion angle affects: cervical loading, walking speed, and muscle activity of the lower limbs.[13]
- Figure A represents an individual with DHS: backward leaning posture of the thorax, increased ankle-joint dorsiflexion angle, and relatively shorter stride length. [13]
- Figure B is ideal walking posture: upright erect posture with decreased ankle dorsiflexion angle allowing for more movement coming from the ankle to propel forward and up. [13]
Geriatric gait[edit | edit source]
At self-selected walking speeds, elderly adults generate decreased joint torques and power in their lower extremities than young adults. These differences are due to the biomechanical and physiological consequences of aging resulting from changes in the underlying neuromuscular components of motor performance and reduction in motor abilities.[14] Pain may also be a factor.[1]
The spatiotemporal changes that occur in geriatric gait:[1]
- Decreased walking speed, less than 1-1.4 metres per second
- Shorter step length
- Slower gait cadence
- Late or a prolonged heel contact
- Decreased vertical oscillation of COM
- Could have decreased hip extension
- Could have increased forward trunk flexion
- Could have decreased arm swing
- Elderly people tend to use hip joint moments more than ankle moments, whereas young people use the ankle to propel forward[14]
Osteoarthritis and Total Joint Replacements[edit | edit source]
Oftentimes patients with knee or hip osteoarthritis develop gait deviations which continue due to "habit" after undergoing total joint replacements.[1] Patients who undergo post-operative rehabilitation report improved joint pain and stiffness but commonly demonstrate incomplete recovery of gait function.[15]
Resources[edit | edit source]
Optional Recommended Reading:
- Harris-Hayes M, Czuppon S, Van Dillen LR, Steger-May K, Sahrmann S, Schootman M, Salsich GB, Clohisy JC, Mueller MJ. Movement-pattern training to improve function in people with chronic hip joint pain: a feasibility randomized clinical trial. journal of orthopaedic & sports physical therapy. 2016 Jun;46(6):452-61.
- Harris-Hayes M, Steger-May K, Bove AM, Foster SN, Mueller MJ, Clohisy JC, Fitzgerald GK. Movement pattern training compared with standard strengthening and flexibility among patients with hip-related groin pain: results of a pilot multicentre randomised clinical trial. BMJ open sport & exercise medicine. 2020 Mar 1;6(1):e000707.
- Igawa T, Katsuhira J, Hosaka A, Uchikoshi K, Ishihara S, Matsudaira K. Kinetic and kinematic variables affecting trunk flexion during level walking in patients with lumbar spinal stenosis. PLoS One. 2018 May 10;13(5):e0197228.
- Igawa T, Ishii K, Suzuki A, Ui H, Urata R, Isogai N, Sasao Y, Nishiyama M, Funao H. Dynamic alignment changes during level walking in patients with dropped head syndrome: Analyses using a three-dimensional motion analysis system. Scientific reports. 2021 Sep 14;11(1):1-0.
- Lamoth CJ, Meijer OG, Daffertshofer A, Wuisman PI, Beek PJ. Effects of chronic low back pain on trunk coordination and back muscle activity during walking: changes in motor control. European Spine Journal. 2006 Feb;15(1):23-40.
Clinical Outcome Measures:
- Hip Disability and Osteoarthritis Outcome Score (HOOS) Download PDF here
- Please view the following short video for an overview of the FABER test used in the assessment of pathologies at the hip, lumbar and sacroiliac region.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Howell, D, Back and Upper Leg Regional Pain and Gait Deviations. Gait Analysis. Plus. 2022
- ↑ Cholewicki J, Breen A, Popovich Jr JM, Reeves NP, Sahrmann SA, Van Dillen LR, Vleeming A, Hodges PW. Can biomechanics research lead to more effective treatment of low back pain? A point-counterpoint debate. journal of orthopaedic & sports physical therapy. 2019 Jun;49(6):425-36.
- ↑ Tabatabaei Molazi F, Mahdian SR, Rajabi R, Karimizadeh Ardakani M. Reliability of Corrective Exercise Specialist Raters Assessing Movement System Impairment Approach Items in Transient Low Back Pain Developers During Prolonged Standing. International Journal of Musculoskeletal Pain Prevention. 2022 Jul 10;7(3):750-8.
- ↑ Lehman GJ. The role and value of symptom-modification approaches in musculoskeletal practice. journal of orthopaedic & sports physical therapy. 2018 Jun;48(6):430-5.
- ↑ 5.0 5.1 5.2 Lamoth CJ, Meijer OG, Daffertshofer A, Wuisman PI, Beek PJ. Effects of chronic low back pain on trunk coordination and back muscle activity during walking: changes in motor control. European Spine Journal. 2006 Feb;15(1):23-40.
- ↑ 6.0 6.1 6.2 6.3 Harris-Hayes M, Steger-May K, Bove AM, Foster SN, Mueller MJ, Clohisy JC, Fitzgerald GK. Movement pattern training compared with standard strengthening and flexibility among patients with hip-related groin pain: results of a pilot multicentre randomised clinical trial. BMJ open sport & exercise medicine. 2020 Mar 1;6(1):e000707.
- ↑ Harris-Hayes M, Czuppon S, Van Dillen LR, Steger-May K, Sahrmann S, Schootman M, Salsich GB, Clohisy JC, Mueller MJ. Movement-pattern training to improve function in people with chronic hip joint pain: a feasibility randomized clinical trial. journal of orthopaedic & sports physical therapy. 2016 Jun;46(6):452-61.
- ↑ Ranawat AS, Gaudiani MA, Slullitel PA, Satalich J, Rebolledo BJ. Foot progression angle walking test: a dynamic diagnostic assessment for femoroacetabular impingement and hip instability. Orthopaedic Journal of Sports Medicine. 2017 Jan 10;5(1):2325967116679641.
- ↑ Lewis CL, Sahrmann SA, Moran DW. Effect of hip angle on anterior hip joint force during gait. Gait & posture. 2010 Oct 1;32(4):603-7.
- ↑ Nüesch C, Mandelli F, Przybilla P, Schären S, Mündermann A, Netzer C. Kinematics and paraspinal muscle activation patterns during walking differ between patients with lumbar spinal stenosis and controls. Gait & Posture. 2023 Jan 1;99:44-50.
- ↑ 11.0 11.1 11.2 11.3 Igawa T, Katsuhira J, Hosaka A, Uchikoshi K, Ishihara S, Matsudaira K. Kinetic and kinematic variables affecting trunk flexion during level walking in patients with lumbar spinal stenosis. PLoS One. 2018 May 10;13(5):e0197228.
- ↑ Igawa T, Ishii K, Urata R, Suzuki A, Ui H, Ideura K, Isogai N, Sasao Y, Funao H. Association between the Horizontal Gaze Ability and Physical Characteristics of Patients with Dropped Head Syndrome. Medicina. 2022 Mar 23;58(4):465.
- ↑ 13.0 13.1 13.2 Igawa T, Ishii K, Suzuki A, Ui H, Urata R, Isogai N, Sasao Y, Nishiyama M, Funao H. Dynamic alignment changes during level walking in patients with dropped head syndrome: Analyses using a three-dimensional motion analysis system. Scientific reports. 2021 Sep 14;11(1):1-0.
- ↑ 14.0 14.1 DeVita P, Hortobagyi T. Age causes a redistribution of joint torques and powers during gait. Journal of applied physiology. 2000 May 1;88(5):1804-11.
- ↑ Bączkowicz D, Skiba G, Czerner M, Majorczyk E. Gait and functional status analysis before and after total knee arthroplasty. The Knee. 2018 Oct 1;25(5):888-96.
- ↑ YouTube. Fabers Test Hip and SIJ | Clinical Physio Premium. Available from: https://www.youtube.com/watch?v=X6trjwpyjdM [last accessed 23/06/2022]