Ethical Considerations in the Child and Adolescent Athlete: Difference between revisions
(table of clinical case scenarios) |
No edit summary |
||
| (29 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Wanda van Niekerk|Wanda van Niekerk]] based on the course by [https://members.physio-pedia.com/instructor/bridey-lee-momberg/ Bridey-Lee Momberg] | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
Providing care to the child and adolescent athlete brings unique ethical dilemmas. When facing these issues, the sports clinician needs to consider a wide range of factors such as autonomy, informed consent, competency and the maturity of the young athlete, as well as the involvement of other stakeholders such as parents and coaches. The clinician's ethical framework will help guide decision-making when managing the child and adolescent athlete. | |||
== Ethical Approaches == | == Ethical Approaches == | ||
Ethical approaches in medicine can be classified into these areas<ref name=":0">Devitt BM. Fundamental ethical principles in sports medicine. Clinics in sports medicine. 2016 Apr 1;35(2):195-204.</ref>: | [[Ethics|Ethical approaches]] in medicine can be classified into these areas<ref name=":0">Devitt BM. Fundamental ethical principles in sports medicine. Clinics in sports medicine. 2016 Apr 1;35(2):195-204.</ref>: | ||
* Virtuous Practice | * Virtuous Practice | ||
| Line 18: | Line 14: | ||
* Principles Approach | * Principles Approach | ||
No single approach will provide the solution to every ethical concern | No single approach will provide the solution to every ethical concern. However, in sports medicine, these approaches are useful to provide a framework to help with decision-making and ethical practice.<ref name=":0" /> | ||
=== Virtuous Practice === | === Virtuous Practice === | ||
Virtuous practice encompasses the following<ref name=":0" />: | Virtuous practice encompasses the following<ref name=":0" />: | ||
* Virtue ethics places importance on the medical professional's/clinician's character (or moral agent) | * Virtue ethics places importance on the medical professional's/clinician's character (or moral agent) | ||
* Virtuous practice argues that morality | * "Virtuous practice argues that morality stems from an individual's character or identity, rather than being a reflection of the actions of the individual"<ref name=":0" /> | ||
* The | * The five virtues that apply to a medical professional are<ref>Beauchamp T.L., Childress J.F.: Principles of biomedical ethics.7th edition2013.Oxford University PressNew Yorkpp. xvi. 459</ref>: | ||
** | ** Trustworthiness | ||
** | ** Integrity | ||
** | ** Discernment | ||
** | ** Compassion | ||
** | ** Conscientiousness | ||
* Another valuable virtue is discipline | * Another valuable virtue is discipline | ||
* Good judgement comes from good character | * Good judgement comes from good character | ||
* In virtuous practice the motivation of the clinician is paramount | * In virtuous practice, the motivation of the clinician is paramount | ||
* Ethical decision making is based on the character of the clinician | * Ethical decision making is based on the character of the clinician | ||
* The virtuous sports medicine clinician's role is first and foremost the welfare of the athlete | * The virtuous sports medicine clinician's role is first and foremost the welfare of the athlete | ||
* Virtuous ethics allows for the adaptation of choices in specific scenarios and the people involved | * Virtuous ethics allows for the adaptation of choices in specific scenarios and the people involved | ||
** This flexibility encourages creative thinking and problem solving | ** This flexibility encourages creative thinking and problem-solving | ||
*'''''"A virtuous person perceives a situation, judges what is right, and then wants to act accordingly because it is their disposition to act well | *'''''"A virtuous person perceives a situation, judges what is right, and then wants to act accordingly because it is their disposition to act well"'''''<ref name=":1">Momberg, B. Ethical consideration in the Child and Adolescent Athlete Course. Plus. 2022</ref> | ||
=== Deontology === | === Deontology === | ||
| Line 46: | Line 42: | ||
* Do the right thing because it is the right thing to do | * Do the right thing because it is the right thing to do | ||
* When deciding what you should do in certain situations ask yourself: "Would it be acceptable if everyone took this type of action?" | * When deciding what you should do in certain situations ask yourself: "Would it be acceptable if everyone took this type of action?" | ||
* Clinical | * Clinical scenario<ref name=":0" />: | ||
** An athlete with concussion wants to continue playing | ** An athlete with concussion wants to continue playing | ||
** Ask yourself: "Would it be acceptable if every athlete with concussion is allowed to continue playing?" | ** Ask yourself: "Would it be acceptable if every athlete with a concussion is allowed to continue playing?" | ||
** The clear answer in this scenario is no | ** The clear answer in this scenario is no because athletes would be put at unacceptable risk and this is morally wrong | ||
* The athlete is seen as the end and not the means | * Deontological ethics are patient-centered.<ref>Tseng PE, Wang YH. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8391290/pdf/ijerph-18-08565.pdf Deontological or Utilitarian? An Eternal Ethical Dilemma in ''Outbreak''.] Int J Environ Res Public Health. 2021 Aug 13;18(16):8565. </ref> The athlete is seen as the end and not the means | ||
* The success of the team is never more important than the welfare of the individual athlete<ref name=":0" /> | * The success of the team is never more important than the welfare of the individual athlete<ref name=":0" /> | ||
* The core teaching of deontology is that people have the duty to do the right thing, irrespective of good or bad consequences | * The core teaching of deontology is that people have the duty to do the right thing, irrespective of good or bad consequences<ref name=":0" /> | ||
** Thus, a decision or action cannot be justified because it had a good outcome or condemned because it had a bad outcome | ** Thus, a decision or action cannot be justified because it had a good outcome or condemned because it had a bad outcome | ||
* The issue with deontology is that it yields absolutes and allows for no grey areas in decision-making<ref name=":1" /> | * The issue with deontology is that it yields absolutes and allows for no grey areas in decision-making<ref name=":1" /> | ||
=== Utilitarianism === | === Utilitarianism === | ||
The Utilitarianism approach entails<ref name=":0" />: | The Utilitarianism approach entails<ref name=":0" /><ref>Vearrier L, Henderson CM. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7809094/pdf/10730_2020_Article_9431.pdf Utilitarian Principlism as a Framework for Crisis Healthcare Ethics]. HEC Forum. 2021 Jun;33(1-2):45-60. </ref>: | ||
* The principle of utilitarianism promotes consequentialism | * The principle of utilitarianism promotes consequentialism | ||
* The rightness or wrongness of a decision or action is judged by its consequences<ref name=":0" /> | * The rightness or wrongness of a decision or action is judged by its consequences<ref name=":0" /> | ||
* The concept of putting the team before the individual athlete is at the forefront of this approach: "There is no 'I' in team" | * The concept of putting the team before the individual athlete is at the forefront of this approach: "There is no 'I' in team" | ||
* The goal is to create the greatest happiness for the greatest amount of individuals | * The goal is to create the greatest happiness for the greatest amount of individuals (in a sports context this will imply the team) | ||
* The action or decision can be justified if the benefits outweigh the actual or potential harm (for example sporting organisations want to do what is right for the sporting organisation) | * The action or decision can be justified if the benefits outweigh the actual or potential harm (for example sporting organisations want to do what is right for the sporting organisation) | ||
* The issue with this approach is that it disparages the interest and welfare of the individual athlete in favour of the team's success | * The issue with this approach is that it disparages the interest and welfare of the individual athlete in favour of the team's success | ||
* This can never be the approach of a team clinician/medical professional | * This can never be the approach of a team clinician/medical professional | ||
* Clinical scenario<ref name=":0" />: | * Clinical scenario<ref name=":0" />: | ||
** There are certain team environment scenarios where | ** There are certain team environment scenarios where a utilitarian approach may be appropriate | ||
** Touring team scenario - an athlete on tour is injured | ** Touring team scenario - an athlete on tour is injured | ||
** The athlete requires focus, time and resources from the team clinician for treatment and rehabilitation that are so demanding that it can potentially negatively affect the rest of the team and the medical services available for the rest of the team | ** The athlete requires focus, time and resources from the team clinician for treatment and rehabilitation that are so demanding that it can potentially negatively affect the rest of the team and the medical services available for the rest of the team | ||
** In this scenario a decision may be made to rather send the athlete home for further treatment and rehabilitation | ** In this scenario, a decision may be made to rather send the athlete home for further treatment and rehabilitation | ||
=== Principles Approach === | === Principles Approach === | ||
| Line 77: | Line 73: | ||
* Most well-known and useful practical, ethical approach | * Most well-known and useful practical, ethical approach | ||
* Regarded as the most appropriate approach in medical ethical situations | * Regarded as the most appropriate approach in medical ethical situations | ||
* Four pillars of [https://www.physio-pedia.com/Ethics,_Principles_and_Values?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal#Four_Principles_of_Medical_Ethics Principles ethics] are: | * Four pillars of [https://www.physio-pedia.com/Ethics,_Principles_and_Values?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal#Four_Principles_of_Medical_Ethics Principles ethics] are:<ref>Varkey B. Principles of clinical ethics and their application to practice. Medical Principles and Practice. 2021;30(1):17-28.</ref> | ||
** Autonomy | ** Autonomy | ||
** Beneficence | ** Beneficence | ||
** | ** Non-maleficence | ||
** Justice | ** Justice | ||
| Line 88: | Line 84: | ||
* Autonomy is the capacity of a competent individual to make an informed, uncoerced decision<ref name=":1" /> | * Autonomy is the capacity of a competent individual to make an informed, uncoerced decision<ref name=":1" /> | ||
* Knowledge is an imperative part of autonomy and is central to [[Informed Consent|informed consent]] | * Knowledge is an imperative part of autonomy and is central to [[Informed Consent|informed consent]] | ||
* In sports medicine, an athlete with an injury who needs to make a decision on treatment choices | * In sports medicine, an athlete with an injury who needs to make a decision on treatment choices needs to understand the injury, comprehend the risks and benefits of all treatment options and be aware of the future prognosis<ref name=":0" /> | ||
* Even though the decision will not only influence the athlete, but perhaps the team as well, the team clinician's primary obligation remains with the individual athlete! | * Even though the decision will not only influence the athlete, but perhaps the team as well, the team clinician's primary obligation remains with the individual athlete! | ||
* Other factors that can influence decision-making are<ref name=":1" />: | * Other factors that can influence decision-making are<ref name=":1" />: | ||
** Pressure from other parties | ** Pressure from other parties | ||
** Goals of athlete | ** Goals of the athlete | ||
** Financial implications | ** Financial implications | ||
* Clinical | * Clinical scenario<ref name=":0" /> | ||
** Athlete with an in-season meniscal injury | ** Athlete with an in-season meniscal injury | ||
** The meniscal tear is repairable but the athlete has two options | ** The meniscal tear is repairable, but the athlete has two options: | ||
*** Option A: Arthroscopic meniscectomy and a fast return to play | *** Option A: Arthroscopic meniscectomy and a fast return to play | ||
*** Option B: Meniscal repair and potentially out for the rest of the season | *** Option B: Meniscal repair and potentially out for the rest of the season | ||
*** Both options have short and long-term consequences | *** Both options have short and long-term consequences: | ||
**** Short term consequences: With option A a quicker return to play, whereas with option B a lengthier rehabilitation period and potentially misses out on the entire season | **** Short term consequences: With option A a quicker return to play, whereas with option B a lengthier rehabilitation period and potentially misses out on the entire season | ||
**** Long-term consequences: With option A there is an increased risk of developing degeneration in the knee later on, whereas with option B there is a reduced risk of long-term risks and degeneration to the knee | **** Long-term consequences: With option A there is an increased risk of developing degeneration in the knee later on, whereas with option B there is a reduced risk of long-term risks and degeneration to the knee | ||
*** In the principle of autonomy the athlete needs to be aware of all these options in their entirety, understand the injury, the risks and benefits of all treatment options and the future prognosis. This is the only way an athlete will be able to make an informed, uncoerced decision. | *** In the principle of autonomy, the athlete needs to be aware of all these options in their entirety, understand the injury, the risks and benefits of all treatment options and the future prognosis. This is the only way an athlete will be able to make an informed, uncoerced decision. | ||
*** Read more: [[Informed Consent]] | *** Read more: [[Informed Consent]] | ||
| Line 108: | Line 104: | ||
* This principle governs that a medical professional/clinician should "do good" and promote the interest of the patient<ref name=":0" /> | * This principle governs that a medical professional/clinician should "do good" and promote the interest of the patient<ref name=":0" /> | ||
* Sports medicine professionals can "do good" for the athlete by treating any injuries and | * Sports medicine professionals can "do good" for the athlete by treating any injuries and preventing further harm | ||
* Beneficence goes hand in hand with | * Beneficence goes hand in hand with non-maleficence | ||
==== Non-maleficence ==== | ==== Non-maleficence ==== | ||
| Line 115: | Line 111: | ||
* First, do no harm<ref name=":0" /> | * First, do no harm<ref name=":0" /> | ||
* In sport, athletes are aware that injury and harm is a risk, but it remains the sports medical professional's role to minimise further harm and try to limit risk as much as possible<ref name=":0" /> | * In sport, athletes are aware that injury and harm is a risk, but it remains the sports medical professional's role to minimise further harm and try to limit risk as much as possible<ref name=":0" /> | ||
* Clinical | * Clinical scenario<ref name=":0" />: | ||
** Athlete requesting an injection of local anaesthetic from the team doctor to allow the athlete to continue playing or to compete again | ** Athlete requesting an injection of local anaesthetic from the team doctor to allow the athlete to continue playing or to compete again | ||
*** Option A: | *** Option A: The doctor provides the injection and the athlete can continue (short-term gain) but potentially risk further injury and/or long-term risk and damage | ||
*** Option B: | *** Option B: The doctor does not provide the injection and the athlete cannot continue play, but this allows for a more thorough assessment of the injury. The athlete will however lose out on possible sporting success and the team may also be impacted. | ||
*** [https://www.world.rugby/the-game/player-welfare/guidelines/ World Rugby] has an [https://resources.world.rugby/worldrugby/document/2021/04/20/d57d0766-9982-4f4b-8545-2243b3df1869/Anaesthetics_Guideline_EN-2-.pdf anaesthetics guideline] clarifying that "a player may not receive local anaesthetics on match day unless it is for the suturing of bleeding wounds or for dental treatment administered by an appropriately qualified medical or dental practitioner." | *** [https://www.world.rugby/the-game/player-welfare/guidelines/ World Rugby] has an [https://resources.world.rugby/worldrugby/document/2021/04/20/d57d0766-9982-4f4b-8545-2243b3df1869/Anaesthetics_Guideline_EN-2-.pdf anaesthetics guideline] clarifying that "a player may not receive local anaesthetics on match day unless it is for the suturing of bleeding wounds or for dental treatment administered by an appropriately qualified medical or dental practitioner." | ||
| Line 124: | Line 120: | ||
===== Beneficence vs Non-maleficence ===== | ===== Beneficence vs Non-maleficence ===== | ||
Athletes may sometimes show risky | Athletes may sometimes show risky behaviours towards their own career and welfare and this can cause difficult situations. As already stated, athletes are aware of the risk and the sports clinician's role is to minimise further harm and try to limit risk. The athlete is not obliged to follow the advice or recommended plan suggested by the clinician, but athletes should be aware of the risk and consequences of the decisions that they make. The sports clinician should also respect an athlete's decision even if it is not aligned with the clinician's opinion. Sporting organisations can help with this by providing guidelines on controversial treatment.<ref name=":0" /> | ||
==== Justice ==== | ==== Justice ==== | ||
| Line 131: | Line 127: | ||
* Justice = to act fairly when the interest of different individuals are in competition with each other | * Justice = to act fairly when the interest of different individuals are in competition with each other | ||
* Three categories of obligations of justice: | * Three categories of obligations of justice: | ||
** Distributive justice - fair distribution of scant resources | ** Distributive justice - the fair distribution of scant resources | ||
*** Scarce resources should be distributed equally based on need and not on the basis of star players getting preferential treatment | *** Scarce resources should be distributed equally based on need and not on the basis of star players getting preferential treatment | ||
** Rights-based justice - respect for people's rights | ** Rights-based justice - respect for people's rights | ||
| Line 140: | Line 136: | ||
[https://www.fims.org/ The International Federation of Sports Medicine (FIMS)] has a Code of Ethics that can be read [https://www.fims.org/about/code-ethics/#:~:text=Sports%20medicine%20physicians%20should%20oppose,they%20participate%20in%20sport%20activities. here]. <ref>International Federation of Sports Medicine. [https://www.fims.org/about/code-ethics/#:~:text=Sports%20medicine%20physicians%20should%20oppose,they%20participate%20in%20sport%20activities. Code of Ethics.]</ref> | [https://www.fims.org/ The International Federation of Sports Medicine (FIMS)] has a Code of Ethics that can be read [https://www.fims.org/about/code-ethics/#:~:text=Sports%20medicine%20physicians%20should%20oppose,they%20participate%20in%20sport%20activities. here]. <ref>International Federation of Sports Medicine. [https://www.fims.org/about/code-ethics/#:~:text=Sports%20medicine%20physicians%20should%20oppose,they%20participate%20in%20sport%20activities. Code of Ethics.]</ref> | ||
The International Federation of Sports Physical Therapists (IFSPT) also has Code of Ethics based on the International Federation of Sports Medicine (FIMS) [https://www.fims.org/about/code-ethics/ Code of Ethics] and the WCPTs [https://world.physio/sites/default/files/2022-03/PS-2022-Ethical_responsibilities_principles_Eng.pdf ethical principles]. You can read the IFSPT Code of Ethics [http://ifspt.org/wp-content/uploads/2014/12/Code-of-Ethics-BNAN-March-2014.pdf here]. | The International Federation of Sports Physical Therapists (IFSPT) also has a Code of Ethics based on the International Federation of Sports Medicine (FIMS) [https://www.fims.org/about/code-ethics/ Code of Ethics] and the WCPTs [https://world.physio/sites/default/files/2022-03/PS-2022-Ethical_responsibilities_principles_Eng.pdf ethical principles]. You can read the IFSPT Code of Ethics [http://ifspt.org/wp-content/uploads/2014/12/Code-of-Ethics-BNAN-March-2014.pdf here]. | ||
== Uniqueness of Sports Medicine == | == Uniqueness of Sports Medicine == | ||
Some of the unique challenges clinicians face when managing athletes include<ref name=":2">Vargas-Mendoza N, Fregoso-Aguilar T, Madrigal-Santillán E, Morales-González Á, Morales-González JA. Ethical concerns in sport: when the will to win exceed the spirit of sport. Behavioral Sciences. 2018 Sep;8(9):78.</ref>: | Some of the unique challenges clinicians face when managing athletes include<ref name=":2">Vargas-Mendoza N, Fregoso-Aguilar T, Madrigal-Santillán E, Morales-González Á, Morales-González JA. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6162520/pdf/behavsci-08-00078.pdf Ethical concerns in sport: when the will to win exceed the spirit of sport.] Behavioral Sciences. 2018 Sep;8(9):78.</ref>: | ||
* Pressure from coaching staff, team management and athletes themselves to return to sport as early as physically possible | * Pressure from coaching staff, team management and athletes themselves to return to sport as early as physically possible | ||
* Athletes experience pressure to earn their | * Athletes experience pressure to earn their teammates' respect, as well as financial implications if injured | ||
* Inaccurate reporting of an injury and the severity thereof by athletes out of fear of missing training or match time | * Inaccurate reporting of an injury and the severity thereof by athletes out of fear of missing training or match time | ||
* Maintaining confidentiality of information | * Maintaining confidentiality of information in the clinician-patient relationship is often a clinician-patient-coach triad with third parties involved such as a coach or team manager | ||
* Athletes are forever striving to improve their performance. Certain tools that athletes will use to achieve this may include: | * Athletes are forever striving to improve their performance.<ref name=":6">Silva TT. [https://www.scielo.br/j/bioet/a/TsZhY5GkgKtYM5KRMNj4K3R/?format=pdf&lang=en Ethical issues in the practice of sports medicine in the contemporary world.] Revista Bioética. 2019 Feb 21;27:62-6.</ref> Certain tools that athletes will use to achieve this may include<ref name=":6" />: | ||
** | ** Dietary supplements | ||
** | ** Medication such as mismanagement or overuse of analgesics | ||
** | ** Doping with prohibited substances and performance-enhancing drugs | ||
*** | *** Find the Word Anti-Doping Code International Standard Prohibited List 2022 [https://www.wada-ama.org/sites/default/files/resources/files/2022list_final_en.pdf here] | ||
** | ** Excessive training by athletes that increases risk | ||
* Read more: [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6162520/pdf/behavsci-08-00078.pdf Ethical concerns in sport: when the will to win exceed the spirit of sport]<ref name=":2" /> | * Read more: [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6162520/pdf/behavsci-08-00078.pdf Ethical concerns in sport: when the will to win exceed the spirit of sport]<ref name=":2" /> | ||
== Role of the Clinician in Sports == | == Role of the Clinician in Sports == | ||
* The health and safety of the individual athlete | * The health and safety of the individual athlete are paramount | ||
* Athletes must have the right to make their own informed decision | * Athletes must have the right to make their own informed decision | ||
** Keep in mind that in a highly charged game environment informed consent is trickier | ** Keep in mind that in a highly charged game environment informed consent is trickier | ||
* The responsibility lies with the clinician to determine if continued training or participation by the athlete is appropriate | * The responsibility lies with the clinician to determine if continued training or participation by the athlete is appropriate | ||
* Maintain a degree of professional distance from the management team | * Maintain a degree of professional distance from the management team | ||
* Clinician first | * Clinician first, team clinician second | ||
* Never abdicate your responsibility to the individual player | * Never abdicate your responsibility to the individual player | ||
| Line 171: | Line 167: | ||
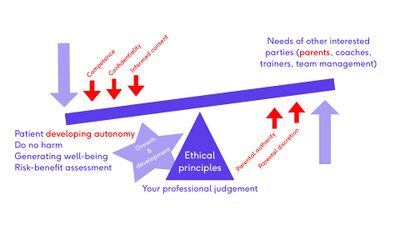
* Ethical approaches and principles are a framework, used as a reference for decision making | * Ethical approaches and principles are a framework, used as a reference for decision making | ||
* Clinical decision-making is centred around the clinician's professional judgement | * Clinical decision-making is centred around the clinician's professional judgement | ||
* Professional judgment always seeks balance - balance between ethical principles such as patient autonomy, avoiding doing harm, generating | * Professional judgment always seeks balance - the balance between ethical principles such as patient autonomy, avoiding doing harm, generating well-being and assessing risks and benefits - while at the same time trying to satisfy the needs and interests of other parties such as coaches, the team management and the team | ||
== The Principles Approach in the Child and Adolescent Athlete == | == The Principles Approach in the Child and Adolescent Athlete == | ||
| Line 179: | Line 175: | ||
** The three concepts that drive the application of autonomy in the child and adolescent athlete are<ref name=":3">Michaud PA, Berg-Kelly K, Macfarlane A, Benaroyo L. Ethics and adolescent care: an international perspective. Current opinion in pediatrics. 2010 Aug 1;22(4):418-22.</ref>: | ** The three concepts that drive the application of autonomy in the child and adolescent athlete are<ref name=":3">Michaud PA, Berg-Kelly K, Macfarlane A, Benaroyo L. Ethics and adolescent care: an international perspective. Current opinion in pediatrics. 2010 Aug 1;22(4):418-22.</ref>: | ||
*** Competence | *** Competence | ||
**** | **** The ability to understand the information needed to make a decision | ||
**** | **** Dependent on the legal system of a country | ||
*** Confidentiality | *** Confidentiality | ||
**** | **** A competent person's right to restrict the divulging of information without their consent | ||
*** Informed Consent | *** Informed Consent | ||
**** | **** A competent person's right to make decisions based on information | ||
**** | **** Three components are necessary for informed consent: | ||
***** | ***** Decision-making capacity, thus competent | ||
***** | ***** Full discussion about risks, benefits, outcomes and prognosis of all treatment options | ||
***** | ***** Sufficient understanding - consider the language used, amount of information and maturity of the athlete | ||
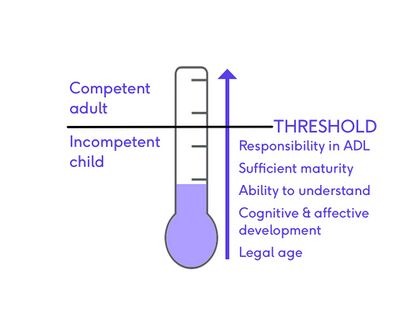
** The assessment and development of Autonomy in the child and adolescent athlete is dependent on a few factors. These include<ref name=":3" />: | ** [[File:Developing autonomy - slide 6.jpg|thumb|400x400px|alt=|Developing Autonomy]]The assessment and development of Autonomy in the child and adolescent athlete is dependent on a few factors. These include<ref name=":3" />: | ||
*** | *** Legal age | ||
*** | *** Cognitive and affective developmental stage of child or adolescent | ||
*** | *** Ability to understand and decide | ||
*** Sufficient maturity and intelligence | *** Sufficient maturity and intelligence | ||
*** Responsibility in activities of daily living (ADL) | *** Responsibility in activities of daily living (ADL) | ||
** Deciding where the threshold is that separates the incompetent child from the competent adult is difficult. One should accept a competent person's decision even if | ** Deciding where the threshold is that separates the incompetent child from the competent adult is difficult. One should accept a competent person's decision even if others believe that the choice is wrong. Children need time to develop these abilities. Responsibility and decision-making should be encouraged in the child and adolescent and, as clinicians, it is crucial that we encourage the development of autonomy in children, protect this developing autonomy and also respect the child's future autonomy.<ref name=":1" /> | ||
* | *''Beneficence and non-maleficence'' considerations<ref name=":4" /> | ||
** | ** Competent adults make decisions on what they think will make their lives go well. but incompetent children cannot make such decisions | ||
** | ** What is the best interest of the child or adolescent and who decides what the standards are to which decisions should be made? | ||
** | ** If the best interest standard is too demanding, should the focus then rather be on not acting against the child or adolescent's interest? | ||
** Consider the child or adolescent's overall needs and not just medical best interests | ** Consider the child or adolescent's overall needs and not just medical best interests | ||
* '''Parental | * '''Parental authority'''<ref name=":4" /> | ||
** Parental authority should be in the interest of the child | ** Parental authority should be in the interest of the child | ||
** It should not extend to causing the child long-lasting harm | ** It should not extend to causing the child long-lasting harm | ||
| Line 208: | Line 204: | ||
== Clinical Case Study == | == Clinical Case Study == | ||
Each case clinicians encounter is different and unique and there is no uniform outcome in all cases. For this reason, it is crucial to consider a shared decision-making process between the child or adolescent athlete, the parents or family and the clinicians involved.<ref name=":8">Ganley TJ. Pediatric [https://journals.sagepub.com/doi/10.1177/0363546520935087?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed Anterior Cruciate Ligament Injury: Advocating for the Next Generation.] The American Journal of Sports Medicine. 2020 Jul;48(8):1809-11.</ref> Clinicians should provide all information and current knowledge on risks and benefits, possible outcomes and prognosis.<ref name=":8" /> | |||
Two | "Eleven-year-old Martin is a promising football academy player with an acute [[Anterior Cruciate Ligament (ACL)|anterior cruciate ligament]] (ACL) tear. There are no other knee structures involved, nor does he have any dynamic instability. Generally, Martin is well. He can run, change direction, kick and jump with no problem."<ref name=":5">Ardern CL, Grindem H, Ekås GR, Seil R, McNamee M. Applying ethical standards to guide shared decision-making with youth athletes. British Journal of Sports Medicine. 2018 Oct 1;52(20):1289-90.</ref> | ||
Two scenarios in the management of Martin's injury: | |||
{| class="wikitable" | {| class="wikitable" | ||
|+ | |+ | ||
| Line 218: | Line 216: | ||
|- | |- | ||
| | | | ||
* Medical team | * Medical team advise ACL reconstruction, parents do not consent to surgery | ||
* Medical team rationale: | * Medical team rationale: | ||
** | ** High knee-demand sport | ||
** | ** High-level athlete | ||
* Possible conflict of interest: | * Possible conflict of interest: | ||
** Medical team works closely with the club | ** Medical team works closely with the club | ||
| Line 230: | Line 228: | ||
** Previous experience of complications from surgery with another sibling | ** Previous experience of complications from surgery with another sibling | ||
| | | | ||
* Medical team advocating for conservative management ( | * Medical team advocating for conservative management (advise against ACL reconstruction), parents keen for surgery to go ahead and want the club to pay for the surgery | ||
* Medical team rationale: | * Medical team rationale: | ||
** | ** Isolated ACL tear with no dynamic instability | ||
** | ** Want to try rehabilitation first | ||
* Parents want surgery and may be invested in Martin's future financial potential | * Parents want surgery and may be invested in Martin's future financial potential | ||
* Unknown if a club will offer a professional contract to someone who has sustained a serious injury, whether conservatively or surgically managed | * Unknown if a club will offer a professional contract to someone who has sustained a serious injury, whether conservatively or surgically managed | ||
|} | |} | ||
=== Decision-Making in Clinical Case Study === | |||
* | |||
Two approaches available in the literature will be applied and combined to illustrate the steps to take in deciding on Martin's (case study) care.<ref name=":1" /> | |||
Approach as set out by Ardern et al.<ref name=":5" /> in applying ethical standards to guide shared decision-making with youth athletes: | |||
* Synthesising the information<ref name=":5" /> | |||
** Gather the relevant facts | |||
*** Fact 1: Unknown if youth athletes with an ACL injury, with or without ACL reconstruction, can have a successful professional/elite sporting career | |||
*** Fact 2: Acceptable treatments for youth athletes with ACL injury include both high-quality rehabilitation alone or in combination with ACL reconstruction<ref>Ardern CL, Ekås GR, Grindem H, Moksnes H, Anderson AF, Chotel F, Cohen M, Forssblad M, Ganley TJ, Feller JA, Karlsson J. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5865521/ 2018 International Olympic Committee consensus statement on prevention, diagnosis and management of paediatric anterior cruciate ligament (ACL) injuries.] British Journal of Sports Medicine. 2018 Apr 1;52(7):422-38.</ref> | |||
** What are the uncertainties? | |||
*** Uncertainty 1: What are Martin's chances of reaching the highest level in his sport with non-surgical management? | |||
*** Uncertainty 2: Can Martin cope through the next few years and onto professional sport with an ACL-deficient knee if surgery is delayed | |||
*** Uncertainty 3: Will the club keep Martin in the football academy if he undergoes an ACL reconstruction? | |||
The second approach is applying a deliberative approach as outlined by Michaud et al.<ref name=":3" /> This approach poses six questions to guide the clinician in the ethical decision-making process. | |||
{| class="wikitable" | |||
|+ | |||
! colspan="2" |'''Deliberative Approach as outlined by Michaud et al.<ref name=":3" />''' | |||
|- | |||
|What? Who? | |||
|What is the main ethical issue? | |||
Who are the stakeholders? | |||
|- | |||
|Competent | |||
|Can the child/adolescent be considered competent? | |||
|- | |||
|Legal standing | |||
|Differs country by country | |||
Age of consent? | |||
Age for informing parents? | |||
Age for the right to confidentiality | |||
|- | |||
|Medical and psychological consequences of each treatment? | |||
|Short- and long-term consequences | |||
|- | |||
|Involving other stakeholders? | |||
|Involving other stakeholders such as parents, coaches, the team | |||
|- | |||
|Balancing the pros and cons of a decision | |||
|Bearing in mind the ethical pillars | |||
Best interests of the child/adolescent | |||
Considering autonomy | |||
Considering the possible vulnerabilities | |||
|} | |||
In the table below, the deliberative approach is applied to the specific case study of Martin with the ACL injury. | |||
{| class="wikitable" | |||
|+ | |||
! colspan="2" |'''Applying a deliberative approach to Martin's case study<ref name=":1" />''' | |||
|- | |||
|'''What? Who?''' | |||
|The main issue is to determine the best management for Martin | |||
A reconstruction now or conservative rehabilitation and a possibility of delayed surgery? | |||
Martin, Martin's parents and the academy, the management team and the coach | |||
|- | |||
|'''Competent?''' | |||
|Martin is only eleven, but what we don't know is: | |||
== | * Does he have sufficient maturity? | ||
* What are his responsibilities in ADLs? | |||
* Does he possess the ability to understand? | |||
* What are his cognitive and affective development like? | |||
|- | |||
|'''Legal standing''' | |||
|Legal age of consent? | |||
|- | |||
|'''Medical and psychological consequences of each treatment''' | |||
|Scenario 1: Do the reconstruction immediately | |||
* Low risk of medical harm? | |||
* Possible growth disruption? | |||
* Absence from football - loses out on 9 - 12 months | |||
* Will he be allowed to stay in the academy? | |||
* Improve chances of adult athletic success and possible future injuries? | |||
** Evidence lacking to be confident in this benefit | |||
|- | |||
|'''Involving other stakeholders''' | |||
|Parents and club management, coach, team | |||
|- | |||
|'''Balancing the pros and cons of a decision''' | |||
| | |||
* Child and parent autonomy | |||
* Facts and vulnerabilities | |||
* What is in Martin's best overall interest? | |||
** ACCEPT PARENTAL DISCRETION | |||
** Conservative management now; delayed surgery | |||
|} | |||
== Approaching Ethical Dilemmas in the Child and Adolescent Athlete == | |||
A summary of the approach clinicians should take in the management of the child and adolescent athlete<ref name=":1" />:[[File:Approaching ethical dilemmas - slide 20.jpg|thumb|alt=|400x400px|Approaching Ethical Dilemmas in the Child and Adolescent Athlete]] | |||
* Clinicians use ethical principles as a framework for decision-making | |||
* Seek balance between the needs and interests of the child and adolescent and the needs and interests of other stakeholders, particularly parents | |||
* Special consideration should be given to developing autonomy in the child, respecting concepts such as competence, informed consent and confidentiality | |||
* Clinicians should be advocates for developing safeguards to protect children and adolescents in sport and oppose any sport or physical activity that is not appropriate for the stage of growth, the development, the general condition and health, and the level of training of children and adolescents<ref name=":7">Mountjoy M, Rhind DJ, Tiivas A, Leglise M. [https://www.researchgate.net/publication/278791974_Safeguarding_the_child_athlete_in_sport_A_review_a_framework_and_recommendations_for_the_IOC_youth_athlete_development_model Safeguarding the child athlete in sport: a review, a framework and recommendations for the IOC youth athlete development model.] British Journal of Sports Medicine. 2015 Jul 1;49(13):883-6.</ref> | |||
* Clinicians should always act in the best overall interest of the child and adolescent athlete and give consideration to parental authority and discretion, especially in the welfare of the incompetent child<ref name=":7" /> | |||
== Resources == | |||
{{#ev:youtube|P-tFvghXqjw|300}}<ref>WiSH - Wits Sport and Health. WiSH Webinar "Ethics in Sport Medicine". Available from: https://www.youtube.com/watch?v=P-tFvghXqjw&t=2387s [last accessed 04/05/2022]</ref> | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Ethics]] | |||
[[Category:Sports Medicine]] | |||
[[Category:Course Pages]] | |||
[[Category:Plus Content]] | |||
Latest revision as of 20:43, 22 January 2023
Top Contributors - Wanda van Niekerk, Kim Jackson, Jess Bell and Ewa Jaraczewska
Introduction[edit | edit source]
Providing care to the child and adolescent athlete brings unique ethical dilemmas. When facing these issues, the sports clinician needs to consider a wide range of factors such as autonomy, informed consent, competency and the maturity of the young athlete, as well as the involvement of other stakeholders such as parents and coaches. The clinician's ethical framework will help guide decision-making when managing the child and adolescent athlete.
Ethical Approaches[edit | edit source]
Ethical approaches in medicine can be classified into these areas[1]:
- Virtuous Practice
- Deontology
- Utilitarianism
- Principles Approach
No single approach will provide the solution to every ethical concern. However, in sports medicine, these approaches are useful to provide a framework to help with decision-making and ethical practice.[1]
Virtuous Practice[edit | edit source]
Virtuous practice encompasses the following[1]:
- Virtue ethics places importance on the medical professional's/clinician's character (or moral agent)
- "Virtuous practice argues that morality stems from an individual's character or identity, rather than being a reflection of the actions of the individual"[1]
- The five virtues that apply to a medical professional are[2]:
- Trustworthiness
- Integrity
- Discernment
- Compassion
- Conscientiousness
- Another valuable virtue is discipline
- Good judgement comes from good character
- In virtuous practice, the motivation of the clinician is paramount
- Ethical decision making is based on the character of the clinician
- The virtuous sports medicine clinician's role is first and foremost the welfare of the athlete
- Virtuous ethics allows for the adaptation of choices in specific scenarios and the people involved
- This flexibility encourages creative thinking and problem-solving
- "A virtuous person perceives a situation, judges what is right, and then wants to act accordingly because it is their disposition to act well"[3]
Deontology[edit | edit source]
The Deontology approach can be summarised as follows[1]:
- Duty-based ethics
- Do the right thing because it is the right thing to do
- When deciding what you should do in certain situations ask yourself: "Would it be acceptable if everyone took this type of action?"
- Clinical scenario[1]:
- An athlete with concussion wants to continue playing
- Ask yourself: "Would it be acceptable if every athlete with a concussion is allowed to continue playing?"
- The clear answer in this scenario is no because athletes would be put at unacceptable risk and this is morally wrong
- Deontological ethics are patient-centered.[4] The athlete is seen as the end and not the means
- The success of the team is never more important than the welfare of the individual athlete[1]
- The core teaching of deontology is that people have the duty to do the right thing, irrespective of good or bad consequences[1]
- Thus, a decision or action cannot be justified because it had a good outcome or condemned because it had a bad outcome
- The issue with deontology is that it yields absolutes and allows for no grey areas in decision-making[3]
Utilitarianism[edit | edit source]
The Utilitarianism approach entails[1][5]:
- The principle of utilitarianism promotes consequentialism
- The rightness or wrongness of a decision or action is judged by its consequences[1]
- The concept of putting the team before the individual athlete is at the forefront of this approach: "There is no 'I' in team"
- The goal is to create the greatest happiness for the greatest amount of individuals (in a sports context this will imply the team)
- The action or decision can be justified if the benefits outweigh the actual or potential harm (for example sporting organisations want to do what is right for the sporting organisation)
- The issue with this approach is that it disparages the interest and welfare of the individual athlete in favour of the team's success
- This can never be the approach of a team clinician/medical professional
- Clinical scenario[1]:
- There are certain team environment scenarios where a utilitarian approach may be appropriate
- Touring team scenario - an athlete on tour is injured
- The athlete requires focus, time and resources from the team clinician for treatment and rehabilitation that are so demanding that it can potentially negatively affect the rest of the team and the medical services available for the rest of the team
- In this scenario, a decision may be made to rather send the athlete home for further treatment and rehabilitation
Principles Approach[edit | edit source]
Principles ethics involve the following[1]:
- Most well-known and useful practical, ethical approach
- Regarded as the most appropriate approach in medical ethical situations
- Four pillars of Principles ethics are:[6]
- Autonomy
- Beneficence
- Non-maleficence
- Justice
Autonomy[edit | edit source]
- A fundamental ethical principle is respect for an individual's autonomy[1]
- Autonomy is the capacity of a competent individual to make an informed, uncoerced decision[3]
- Knowledge is an imperative part of autonomy and is central to informed consent
- In sports medicine, an athlete with an injury who needs to make a decision on treatment choices needs to understand the injury, comprehend the risks and benefits of all treatment options and be aware of the future prognosis[1]
- Even though the decision will not only influence the athlete, but perhaps the team as well, the team clinician's primary obligation remains with the individual athlete!
- Other factors that can influence decision-making are[3]:
- Pressure from other parties
- Goals of the athlete
- Financial implications
- Clinical scenario[1]
- Athlete with an in-season meniscal injury
- The meniscal tear is repairable, but the athlete has two options:
- Option A: Arthroscopic meniscectomy and a fast return to play
- Option B: Meniscal repair and potentially out for the rest of the season
- Both options have short and long-term consequences:
- Short term consequences: With option A a quicker return to play, whereas with option B a lengthier rehabilitation period and potentially misses out on the entire season
- Long-term consequences: With option A there is an increased risk of developing degeneration in the knee later on, whereas with option B there is a reduced risk of long-term risks and degeneration to the knee
- In the principle of autonomy, the athlete needs to be aware of all these options in their entirety, understand the injury, the risks and benefits of all treatment options and the future prognosis. This is the only way an athlete will be able to make an informed, uncoerced decision.
- Read more: Informed Consent
Beneficence[edit | edit source]
- This principle governs that a medical professional/clinician should "do good" and promote the interest of the patient[1]
- Sports medicine professionals can "do good" for the athlete by treating any injuries and preventing further harm
- Beneficence goes hand in hand with non-maleficence
Non-maleficence[edit | edit source]
- First, do no harm[1]
- In sport, athletes are aware that injury and harm is a risk, but it remains the sports medical professional's role to minimise further harm and try to limit risk as much as possible[1]
- Clinical scenario[1]:
- Athlete requesting an injection of local anaesthetic from the team doctor to allow the athlete to continue playing or to compete again
- Option A: The doctor provides the injection and the athlete can continue (short-term gain) but potentially risk further injury and/or long-term risk and damage
- Option B: The doctor does not provide the injection and the athlete cannot continue play, but this allows for a more thorough assessment of the injury. The athlete will however lose out on possible sporting success and the team may also be impacted.
- World Rugby has an anaesthetics guideline clarifying that "a player may not receive local anaesthetics on match day unless it is for the suturing of bleeding wounds or for dental treatment administered by an appropriately qualified medical or dental practitioner."
- Athlete requesting an injection of local anaesthetic from the team doctor to allow the athlete to continue playing or to compete again
Beneficence vs Non-maleficence[edit | edit source]
Athletes may sometimes show risky behaviours towards their own career and welfare and this can cause difficult situations. As already stated, athletes are aware of the risk and the sports clinician's role is to minimise further harm and try to limit risk. The athlete is not obliged to follow the advice or recommended plan suggested by the clinician, but athletes should be aware of the risk and consequences of the decisions that they make. The sports clinician should also respect an athlete's decision even if it is not aligned with the clinician's opinion. Sporting organisations can help with this by providing guidelines on controversial treatment.[1]
Justice[edit | edit source]
The fourth pillar of Principles ethics is justice and includes the following:[1]
- Justice = to act fairly when the interest of different individuals are in competition with each other
- Three categories of obligations of justice:
- Distributive justice - the fair distribution of scant resources
- Scarce resources should be distributed equally based on need and not on the basis of star players getting preferential treatment
- Rights-based justice - respect for people's rights
- Clinicians should respect each athlete's right to treatment and may not fail to treat because of bias or contrary beliefs
- Legal justice - respect for morally acceptable laws
- Clinicians should wilfully do no harm to any athlete in their care
- Clinicians should wilfully do no harm to any athlete in their care
- Distributive justice - the fair distribution of scant resources
Code of Ethics[edit | edit source]
The International Federation of Sports Medicine (FIMS) has a Code of Ethics that can be read here. [7]
The International Federation of Sports Physical Therapists (IFSPT) also has a Code of Ethics based on the International Federation of Sports Medicine (FIMS) Code of Ethics and the WCPTs ethical principles. You can read the IFSPT Code of Ethics here.
Uniqueness of Sports Medicine[edit | edit source]
Some of the unique challenges clinicians face when managing athletes include[8]:
- Pressure from coaching staff, team management and athletes themselves to return to sport as early as physically possible
- Athletes experience pressure to earn their teammates' respect, as well as financial implications if injured
- Inaccurate reporting of an injury and the severity thereof by athletes out of fear of missing training or match time
- Maintaining confidentiality of information in the clinician-patient relationship is often a clinician-patient-coach triad with third parties involved such as a coach or team manager
- Athletes are forever striving to improve their performance.[9] Certain tools that athletes will use to achieve this may include[9]:
- Dietary supplements
- Medication such as mismanagement or overuse of analgesics
- Doping with prohibited substances and performance-enhancing drugs
- Find the Word Anti-Doping Code International Standard Prohibited List 2022 here
- Excessive training by athletes that increases risk
- Read more: Ethical concerns in sport: when the will to win exceed the spirit of sport[8]
Role of the Clinician in Sports[edit | edit source]
- The health and safety of the individual athlete are paramount
- Athletes must have the right to make their own informed decision
- Keep in mind that in a highly charged game environment informed consent is trickier
- The responsibility lies with the clinician to determine if continued training or participation by the athlete is appropriate
- Maintain a degree of professional distance from the management team
- Clinician first, team clinician second
- Never abdicate your responsibility to the individual player
Approaching Ethical Dilemmas[edit | edit source]
- Ethical approaches and principles are a framework, used as a reference for decision making
- Clinical decision-making is centred around the clinician's professional judgement
- Professional judgment always seeks balance - the balance between ethical principles such as patient autonomy, avoiding doing harm, generating well-being and assessing risks and benefits - while at the same time trying to satisfy the needs and interests of other parties such as coaches, the team management and the team
The Principles Approach in the Child and Adolescent Athlete[edit | edit source]
Applying the principles approach to a child is dependent on competence.[10] Competence forms part of autonomy.
- Autonomy
- The three concepts that drive the application of autonomy in the child and adolescent athlete are[11]:
- Competence
- The ability to understand the information needed to make a decision
- Dependent on the legal system of a country
- Confidentiality
- A competent person's right to restrict the divulging of information without their consent
- Informed Consent
- A competent person's right to make decisions based on information
- Three components are necessary for informed consent:
- Decision-making capacity, thus competent
- Full discussion about risks, benefits, outcomes and prognosis of all treatment options
- Sufficient understanding - consider the language used, amount of information and maturity of the athlete
- Competence
- The assessment and development of Autonomy in the child and adolescent athlete is dependent on a few factors. These include[11]:
- Legal age
- Cognitive and affective developmental stage of child or adolescent
- Ability to understand and decide
- Sufficient maturity and intelligence
- Responsibility in activities of daily living (ADL)
- Deciding where the threshold is that separates the incompetent child from the competent adult is difficult. One should accept a competent person's decision even if others believe that the choice is wrong. Children need time to develop these abilities. Responsibility and decision-making should be encouraged in the child and adolescent and, as clinicians, it is crucial that we encourage the development of autonomy in children, protect this developing autonomy and also respect the child's future autonomy.[3]
- The three concepts that drive the application of autonomy in the child and adolescent athlete are[11]:
- Beneficence and non-maleficence considerations[10]
- Competent adults make decisions on what they think will make their lives go well. but incompetent children cannot make such decisions
- What is the best interest of the child or adolescent and who decides what the standards are to which decisions should be made?
- If the best interest standard is too demanding, should the focus then rather be on not acting against the child or adolescent's interest?
- Consider the child or adolescent's overall needs and not just medical best interests
- Parental authority[10]
- Parental authority should be in the interest of the child
- It should not extend to causing the child long-lasting harm
- Parent's autonomy should also be respected, but there are limits to parental authority
- The focus should always be on the protection of the whole child and their overall interests
Clinical Case Study[edit | edit source]
Each case clinicians encounter is different and unique and there is no uniform outcome in all cases. For this reason, it is crucial to consider a shared decision-making process between the child or adolescent athlete, the parents or family and the clinicians involved.[12] Clinicians should provide all information and current knowledge on risks and benefits, possible outcomes and prognosis.[12]
"Eleven-year-old Martin is a promising football academy player with an acute anterior cruciate ligament (ACL) tear. There are no other knee structures involved, nor does he have any dynamic instability. Generally, Martin is well. He can run, change direction, kick and jump with no problem."[13]
Two scenarios in the management of Martin's injury:
| Scenario 1 | Scenario 2 |
|---|---|
|
|
Decision-Making in Clinical Case Study[edit | edit source]
Two approaches available in the literature will be applied and combined to illustrate the steps to take in deciding on Martin's (case study) care.[3]
Approach as set out by Ardern et al.[13] in applying ethical standards to guide shared decision-making with youth athletes:
- Synthesising the information[13]
- Gather the relevant facts
- Fact 1: Unknown if youth athletes with an ACL injury, with or without ACL reconstruction, can have a successful professional/elite sporting career
- Fact 2: Acceptable treatments for youth athletes with ACL injury include both high-quality rehabilitation alone or in combination with ACL reconstruction[14]
- What are the uncertainties?
- Uncertainty 1: What are Martin's chances of reaching the highest level in his sport with non-surgical management?
- Uncertainty 2: Can Martin cope through the next few years and onto professional sport with an ACL-deficient knee if surgery is delayed
- Uncertainty 3: Will the club keep Martin in the football academy if he undergoes an ACL reconstruction?
- Gather the relevant facts
The second approach is applying a deliberative approach as outlined by Michaud et al.[11] This approach poses six questions to guide the clinician in the ethical decision-making process.
| Deliberative Approach as outlined by Michaud et al.[11] | |
|---|---|
| What? Who? | What is the main ethical issue?
Who are the stakeholders? |
| Competent | Can the child/adolescent be considered competent? |
| Legal standing | Differs country by country
Age of consent? Age for informing parents? Age for the right to confidentiality |
| Medical and psychological consequences of each treatment? | Short- and long-term consequences |
| Involving other stakeholders? | Involving other stakeholders such as parents, coaches, the team |
| Balancing the pros and cons of a decision | Bearing in mind the ethical pillars
Best interests of the child/adolescent Considering autonomy Considering the possible vulnerabilities |
In the table below, the deliberative approach is applied to the specific case study of Martin with the ACL injury.
| Applying a deliberative approach to Martin's case study[3] | |
|---|---|
| What? Who? | The main issue is to determine the best management for Martin
A reconstruction now or conservative rehabilitation and a possibility of delayed surgery? Martin, Martin's parents and the academy, the management team and the coach |
| Competent? | Martin is only eleven, but what we don't know is:
|
| Legal standing | Legal age of consent? |
| Medical and psychological consequences of each treatment | Scenario 1: Do the reconstruction immediately
|
| Involving other stakeholders | Parents and club management, coach, team |
| Balancing the pros and cons of a decision |
|
Approaching Ethical Dilemmas in the Child and Adolescent Athlete[edit | edit source]
A summary of the approach clinicians should take in the management of the child and adolescent athlete[3]:
- Clinicians use ethical principles as a framework for decision-making
- Seek balance between the needs and interests of the child and adolescent and the needs and interests of other stakeholders, particularly parents
- Special consideration should be given to developing autonomy in the child, respecting concepts such as competence, informed consent and confidentiality
- Clinicians should be advocates for developing safeguards to protect children and adolescents in sport and oppose any sport or physical activity that is not appropriate for the stage of growth, the development, the general condition and health, and the level of training of children and adolescents[15]
- Clinicians should always act in the best overall interest of the child and adolescent athlete and give consideration to parental authority and discretion, especially in the welfare of the incompetent child[15]
Resources[edit | edit source]
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 Devitt BM. Fundamental ethical principles in sports medicine. Clinics in sports medicine. 2016 Apr 1;35(2):195-204.
- ↑ Beauchamp T.L., Childress J.F.: Principles of biomedical ethics.7th edition2013.Oxford University PressNew Yorkpp. xvi. 459
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 Momberg, B. Ethical consideration in the Child and Adolescent Athlete Course. Plus. 2022
- ↑ Tseng PE, Wang YH. Deontological or Utilitarian? An Eternal Ethical Dilemma in Outbreak. Int J Environ Res Public Health. 2021 Aug 13;18(16):8565.
- ↑ Vearrier L, Henderson CM. Utilitarian Principlism as a Framework for Crisis Healthcare Ethics. HEC Forum. 2021 Jun;33(1-2):45-60.
- ↑ Varkey B. Principles of clinical ethics and their application to practice. Medical Principles and Practice. 2021;30(1):17-28.
- ↑ International Federation of Sports Medicine. Code of Ethics.
- ↑ 8.0 8.1 Vargas-Mendoza N, Fregoso-Aguilar T, Madrigal-Santillán E, Morales-González Á, Morales-González JA. Ethical concerns in sport: when the will to win exceed the spirit of sport. Behavioral Sciences. 2018 Sep;8(9):78.
- ↑ 9.0 9.1 Silva TT. Ethical issues in the practice of sports medicine in the contemporary world. Revista Bioética. 2019 Feb 21;27:62-6.
- ↑ 10.0 10.1 10.2 Baines P. Medical ethics for children: applying the four principles to paediatrics. Journal of medical ethics. 2008 Mar 1;34(3):141-5.
- ↑ 11.0 11.1 11.2 11.3 Michaud PA, Berg-Kelly K, Macfarlane A, Benaroyo L. Ethics and adolescent care: an international perspective. Current opinion in pediatrics. 2010 Aug 1;22(4):418-22.
- ↑ 12.0 12.1 Ganley TJ. Pediatric Anterior Cruciate Ligament Injury: Advocating for the Next Generation. The American Journal of Sports Medicine. 2020 Jul;48(8):1809-11.
- ↑ 13.0 13.1 13.2 13.3 Ardern CL, Grindem H, Ekås GR, Seil R, McNamee M. Applying ethical standards to guide shared decision-making with youth athletes. British Journal of Sports Medicine. 2018 Oct 1;52(20):1289-90.
- ↑ Ardern CL, Ekås GR, Grindem H, Moksnes H, Anderson AF, Chotel F, Cohen M, Forssblad M, Ganley TJ, Feller JA, Karlsson J. 2018 International Olympic Committee consensus statement on prevention, diagnosis and management of paediatric anterior cruciate ligament (ACL) injuries. British Journal of Sports Medicine. 2018 Apr 1;52(7):422-38.
- ↑ 15.0 15.1 Mountjoy M, Rhind DJ, Tiivas A, Leglise M. Safeguarding the child athlete in sport: a review, a framework and recommendations for the IOC youth athlete development model. British Journal of Sports Medicine. 2015 Jul 1;49(13):883-6.
- ↑ WiSH - Wits Sport and Health. WiSH Webinar "Ethics in Sport Medicine". Available from: https://www.youtube.com/watch?v=P-tFvghXqjw&t=2387s [last accessed 04/05/2022]