Application of the New Protocol for Plantar Heel Pain: Difference between revisions
No edit summary |
No edit summary |
||
| (14 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor '''- [[User:Merinda Rodseth|Merinda Rodseth]] based on the course by | '''Original Editor '''- [[User:Merinda Rodseth|Merinda Rodseth]] based on the course by | ||
[https://members.physio-pedia.com/course_tutor/bernice-saban Bernice Saban<br> | [https://members.physio-pedia.com/course_tutor/bernice-saban/ Bernice Saban]<br> | ||
| Line 7: | Line 7: | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
The application of the “new protocol” for Plantar Heel Pain (PHP) will be discussed in three distinct parts: | The application of the “new protocol” for [[Introduction to Plantar Heel Pain|plantar heel pain]] (PHP) will be discussed in three distinct parts: | ||
# Assessment of the patient | # Assessment of the patient | ||
| Line 14: | Line 14: | ||
== Patient Assessment == | == Patient Assessment == | ||
<blockquote>“Not only will a thorough subjective exam tell you what the problem(s) are, but also how to treat them” | <blockquote> “Not only will a thorough subjective exam tell you what the problem(s) are, but also how to treat them” - Geoff Maitland </blockquote> | ||
Communication plays an essential role in the process | Communication plays an essential role in the assessment process and effective, competent clinical communication skills are key to high-quality healthcare.<ref>Iversen ED, Wolderslund MO, Kofoed PE, Gulbrandsen P, Poulsen H, Cold S et al. [https://link.springer.com/content/pdf/10.1186/s12909-020-02050-3.pdf Codebook for rating clinical communication skills based on the Calgary-Cambridge Guide]. BMC Med Educ. 2020;20(1):140. </ref> Different communication techniques, such as motivational interviewing, also have positive effects on the outcomes of physiotherapy treatment.<ref>Hiller A, Delany C. [https://www.semanticscholar.org/paper/Communication-in-physiotherapy%3A-challenging-Hiller/6f7bf1de5ae21579737e0a7aeb9744981af29497 Communication in physiotherapy: Challenging established theoretical approaches]. Manipulating Practices: A Critical Physiotherapy Reader. 2018:308-33. </ref> Following the principles of [[Motivational Interviewing|motivational interviewing]], communication with the patient should include: <ref name=":0">Bernice Saban. Application of the New Protocol for Plantar Heel Pain. Plus Course. 2021</ref><ref>Norris M, Eva G, Fortune J, Frater T, Breckon J. [https://bmcmededuc.biomedcentral.com/track/pdf/10.1186/s12909-019-1560-8.pdf Educating undergraduate occupational therapy and physiotherapy students in motivational interviewing: the student perspective]. BMC medical education. 2019 Dec;19(1):1-7. </ref><ref>Pace BT, Dembe A, Soma CS, Baldwin SA, Atkins DC, Imel ZE. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6039097/pdf/nihms978010.pdf A multivariate meta-analysis of motivational interviewing process and outcome]. Psychology of Addictive Behaviors. 2017 Aug;31(5):524. </ref><ref>Hashim MJ. [https://www.aafp.org/afp/2017/0101/afp20170101p29.pdf Patient-centered communication: basic skills]. American family physician. 2017 Jan 1;95(1):29-34. </ref><ref>Diener I. Physiotherapy support for self-management of persisting musculoskeletal pain disorders. South African Journal of Physiotherapy. 2021 Oct 29;77(1):1564.</ref> | ||
* Open questions | * Open questions | ||
| Line 25: | Line 25: | ||
* Explanations during the interview | * Explanations during the interview | ||
Assessment is one of the cornerstones of the physiotherapeutic approach.<ref name=":1">Hengeveld E (ed.), Banks K (ed.), Maitland GD. Maitland's peripheral manipulation. 4th ed. Philadelphia: Elsevier/Butterworth Heinemann; 2005.</ref> While the principles of musculoskeletal assessment are universal, it is important to also focus specifically on the area | Assessment is one of the cornerstones of the physiotherapeutic approach.<ref name=":1">Hengeveld E (ed.), Banks K (ed.), Maitland GD. Maitland's peripheral manipulation. 4th ed. Philadelphia: Elsevier/Butterworth Heinemann; 2005.</ref> While the principles of musculoskeletal assessment are universal, it is important to also focus specifically on the patient's complaint/area of concern, which in this instance is the heel. | ||
The typical musculoskeletal assessment includes:<ref name=":1" /><ref name=":2">Alazzawi S, Sukeik M, King D, Vemulapalli K. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5241541/pdf/WJO-8-21.pdf Foot and ankle history and clinical examination: A guide to everyday practice]. World journal of orthopedics. 2017 Jan 18;8(1):21 </ref> | The typical musculoskeletal assessment includes:<ref name=":1" /><ref name=":2">Alazzawi S, Sukeik M, King D, Vemulapalli K. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5241541/pdf/WJO-8-21.pdf Foot and ankle history and clinical examination: A guide to everyday practice]. World journal of orthopedics. 2017 Jan 18;8(1):21 </ref> | ||
| Line 31: | Line 31: | ||
* Subjective assessment (interview) | * Subjective assessment (interview) | ||
* Objective/physical examination | * Objective/physical examination | ||
[[File:Interview in PHP Assessment.jpg|thumb|500x500px|'''Figure 1'''. Aspects included in the Subjective Assessment of PHPS <ref name=":0" />]] | |||
The interview should include:<ref name=":0" /> | The '''interview''' should include (Figure 1):<ref name=":0" /> | ||
* Personal information | * Personal information | ||
* Analysis of the symptoms to | * Analysis of the symptoms to determine whether the condition is typical or atypical | ||
* Differential diagnosis of the sources of heel pain, including systemic sources, yellow flags and red flags | * Differential diagnosis of the sources of heel pain, including systemic sources, [[The Flag System|yellow flags]] and [[An Introduction to Red Flags in Serious Pathology|red flags]] | ||
* Functional measures including functional limitations | * Functional measures including functional limitations | ||
* General health | * General health | ||
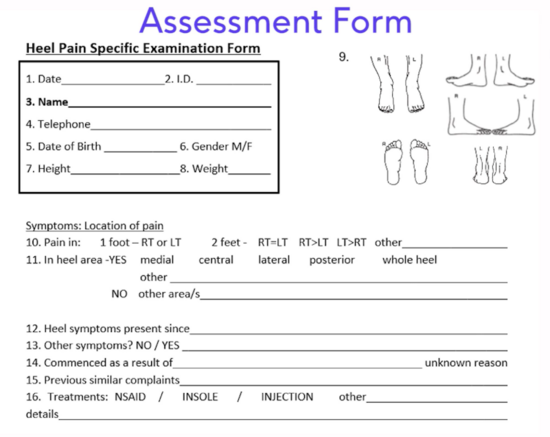
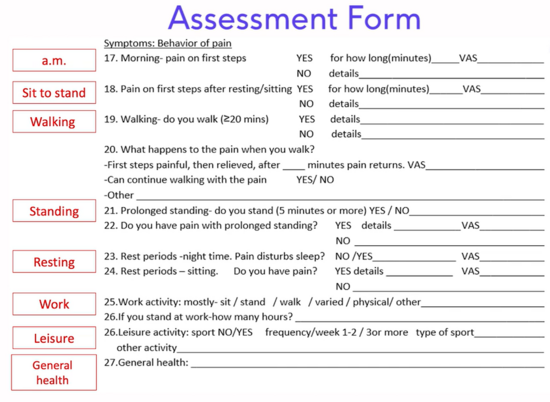
Typical questions asked in a thorough interview (subjective evaluation) | Typical questions asked in a thorough interview (subjective evaluation) include (Figure 2 and 3):<ref name=":0" /><ref name=":2" /><ref>Killens D. [https://web.a.ebscohost.com/ehost/ebookviewer/ebook/bmxlYmtfXzIxNDI1MjVfX0FO0?sid=fce810a0-b36b-4ffa-8db4-223b8adc0f22%40sessionmgr4007&vid=3&format=EB&rid=1 Mobilizing the Myofascial System: A Clinical Guide to Assessment and Treatment of Myofascial Dysfunctions]. Edinburgh: Handspring Publishing; 2018. </ref> | ||
* Areas of pain | * Areas of pain | ||
| Line 51: | Line 52: | ||
[[File:PHP Ax form part1 Area.png|frameless|550x550px]] | [[File:PHP Ax form part1 Area.png|frameless|550x550px]] | ||
'''Figure | '''Figure 2'''. Heel Pain Specific Examination Form - Location, Pain and History | ||
[[File:PHP Ax form part 2 Behaviour.png|frameless|550x550px]] | [[File:PHP Ax form part 2 Behaviour.png|frameless|550x550px]] | ||
'''Figure | '''Figure 3'''. Heel Pain Specific Examination Form - Behaviour of the Symptoms | ||
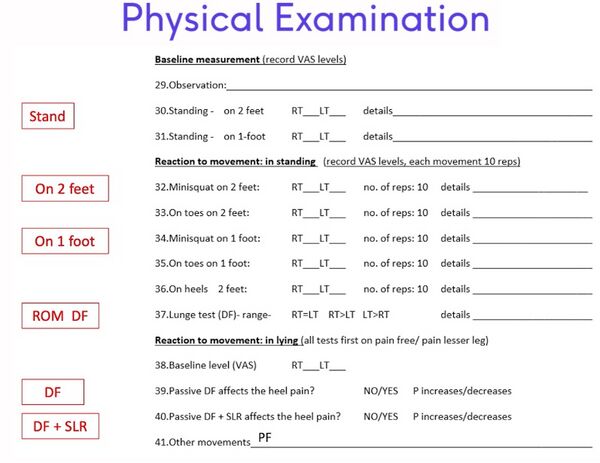
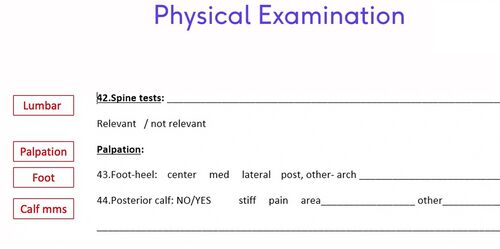
The interview is followed by the physical examination of the patient, which includes ( | The interview is followed by the physical examination of the patient, which includes (Figures 4 and 5):<ref name=":0" /> | ||
* Physical measures | |||
** For PHPS, these measures include the 3 heel pain tests previously discussed<ref name=":3">Saban B, Masharawi Y. [https://pubmed.ncbi.nlm.nih.gov/27908459/ Three single leg standing tests for clinical assessment of chronic plantar heel pain syndrome: static stance, half-squat and heel rise]. Physiotherapy. 2017 Jun 1;103(2):237-44. | |||
</ref> | </ref> | ||
* | * Relevant additional tests to support the estimated diagnosis and whether the presentation is typical or atypical | ||
* Investigation of other sources of heel pain, including the spine, systemic disease, yellow flags and red flags | * Investigation of other sources of heel pain, including the spine, systemic disease, yellow flags and red flags | ||
[[File:PHP Ax form part 3 Phys | [[File:PHP Ax form part 3 Phys examfinal.jpg|frameless|600x600px]] | ||
'''Figure | '''Figure 4'''. Heel Pain Specific Examination Form - Physical Examination<ref name=":0" /> | ||
[[File:PHP Ax form part 4 PE other | [[File:PHP Ax form part 4 PE other testsfinal.jpg|frameless|500x500px]] | ||
'''Figure | '''Figure 5'''. Heel Pain Specific Examination Form - Physical examination<ref name=":0" /> | ||
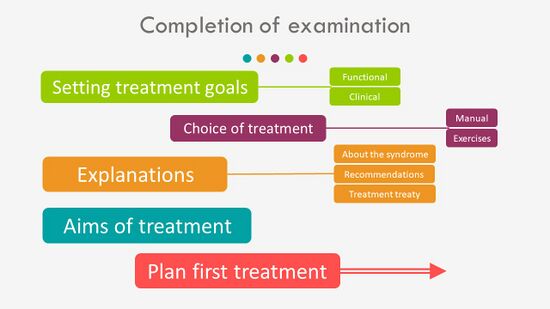
Completion of the examination includes (Figure | Completion of the examination includes (Figure 6):<ref name=":0" /> | ||
* | * Setting of functional and clinical treatment goals<ref>Stevens A, Köke A, van der Weijden T, Beurskens A. [https://www.researchgate.net/profile/Anna-Beurskens/publication/316910588_The_development_of_a_patient-specific_method_for_physiotherapy_goal_setting_a_user-centered_design/links/5a1d1335a6fdcc0af3269d5c/The-development-of-a-patient-specific-method-for-physiotherapy-goal-setting-a-user-centered-design.pdf The development of a patient-specific method for physiotherapy goal setting: a user-centered design]. Disability and rehabilitation. 2018 Aug 14;40(17):2048-55. </ref> | ||
* Planning of the treatment interventions - manual therapy and exercises | * Planning of the treatment interventions - manual therapy and exercises | ||
* Explanations to the | * Explanations to the patient including:<ref>Cotchett M, Rathleff MS, Dilnot M, Landorf KB, Morrissey D, Barton C. [https://jfootankleres.biomedcentral.com/articles/10.1186/s13047-020-0377-3 Lived experience and attitudes of people with plantar heel pain: a qualitative exploration.] Journal of foot and ankle research. 2020 Dec;13(1):1-9.</ref> | ||
** Information about PHPS | |||
** Recommendations and advice | |||
** Answering questions | |||
** Information about the treatment plan | |||
[[File:Completion of examination.jpg|frameless|550x550px]] | [[File:Completion of examination.jpg|frameless|550x550px]] | ||
'''Figure | '''Figure 6'''. Completion of the Examination <ref name=":0" /> | ||
== Planning of the Initial Sessions == | == Planning of the Initial Sessions == | ||
| Line 91: | Line 93: | ||
* Assessment | * Assessment | ||
* Manual | * Manual therapy | ||
* Exercise | * Exercise therapy | ||
The '''''<u>first treatment session</u>''''' should include: | The '''''<u>first treatment session</u>''''' should include: | ||
* The interview and physical examination, including the 3 clinical tests <ref name=":3" /> and palpation of the calf muscles <ref name=":3" /><ref name=":4">Saban B, Deutscher D, Ziv T. [https://www.sciencedirect.com/science/article/abs/pii/S1356689X13001471?via%3Dihub Deep massage to posterior calf muscles in combination with neural mobilization exercises as a treatment for heel pain: a pilot randomized clinical trial]. Manual therapy. 2014 Apr 1;19(2):102-8. </ref> | * The interview and physical examination, including the [[A New Protocol for Plantar Heel Pain|3 clinical tests]]<ref name=":3" /> and palpation of the calf muscles<ref name=":3" /><ref name=":4">Saban B, Deutscher D, Ziv T. [https://www.sciencedirect.com/science/article/abs/pii/S1356689X13001471?via%3Dihub Deep massage to posterior calf muscles in combination with neural mobilization exercises as a treatment for heel pain: a pilot randomized clinical trial]. Manual therapy. 2014 Apr 1;19(2):102-8. </ref> | ||
* Treatment - deep friction massage of the calf muscles for at least 10 minutes <ref name=":4" /> | * Treatment - [[The Theory and Practice of Massage and Exercise for Plantar Heel Pain|deep friction massage]] of the calf muscles for at least 10 minutes<ref name=":4" /> | ||
* Reassessment using the 3 clinical tests | * Reassessment using the 3 clinical tests | ||
* Home exercise - the | * Home exercise - the [[The Theory and Practice of Massage and Exercise for Plantar Heel Pain|lunge stretch exercise]] <ref name=":4" /> | ||
For the '''<u>''second treatment session''</u>''', it is necessary to establish “what has changed” since the previous session with the patient through reassessment. From here on, each treatment should be customised for | For the '''<u>''second treatment session''</u>''', it is necessary to establish “what has changed” since the previous session with the patient through reassessment. From here on, each treatment should be customised for the patient in order to comprehensively address their needs. | ||
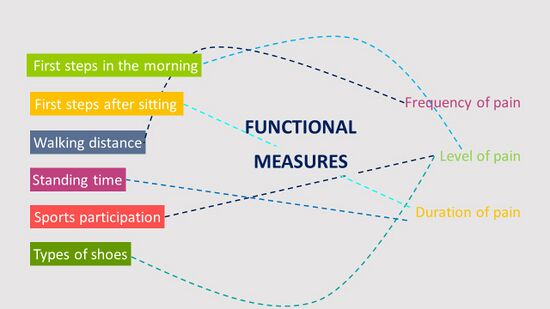
The second treatment will include an assessment of the functional measures as reported by the patient (Figure | The second treatment will include an assessment of the functional measures as reported by the patient (Figure 7). These generally include the level, frequency and duration of the pain with “first steps in the morning”, followed by other measures previously reported by the patient.<ref name=":0" /> | ||
[[File:Functional measure reassessment.jpg|frameless|550x550px]] | [[File:Functional measure reassessment.jpg|frameless|550x550px]] | ||
'''Figure | '''Figure 7'''. Functional Measures<ref name=":0" /> | ||
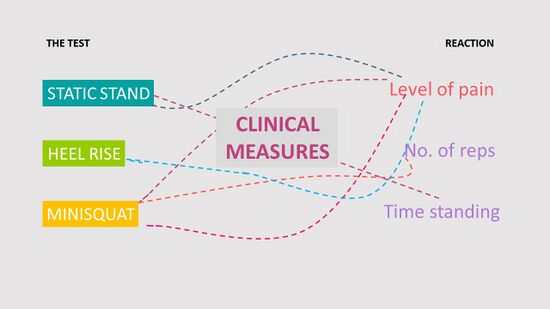
Following the reassessment of the functional measures, the clinical measures (3 clinical tests) should also be reassessed based on the (Figure | Following the reassessment of the functional measures, the clinical measures (3 clinical tests) should also be reassessed based on the (Figure 8): | ||
* Level of pain | * Level of pain | ||
| Line 120: | Line 122: | ||
[[File:Clinical Measures.jpg|frameless|550x550px]] | [[File:Clinical Measures.jpg|frameless|550x550px]] | ||
'''Figure | '''Figure 8'''. Reassessment of the Clinical Measures <ref name=":0" /> | ||
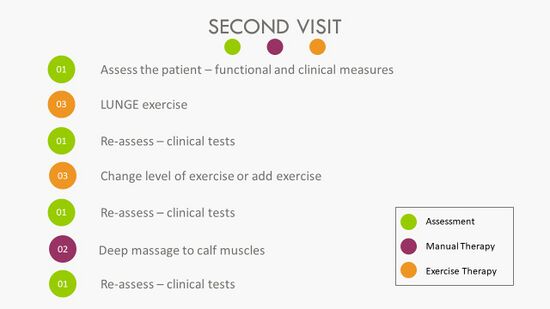
A summary of the steps to follow during the second treatment session is provided in Figure | A summary of the steps to follow during the second treatment session is provided in Figure 9: | ||
[[File:Second treatment outlay.jpg|frameless|550x550px]] | [[File:Second treatment outlay.jpg|frameless|550x550px]] | ||
'''Figure | '''Figure 9'''. Second Treatment Session <ref name=":0" /> | ||
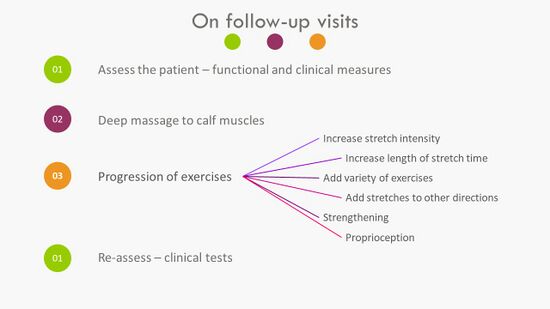
All '''<u>''follow-up sessions''</u>''' should follow the sequence of the first session while progressing the exercises as necessary (Figure | All '''<u>''follow-up sessions''</u>''' should follow the sequence of the first session while progressing the exercises as necessary (Figure 10). | ||
[[File:Outlay of follow up sessions PHPS.jpg|frameless|550x550px]] | [[File:Outlay of follow up sessions PHPS.jpg|frameless|550x550px]] | ||
'''Figure | '''Figure 10'''. Approach to Follow-Up Visits <ref name=":0" /> | ||
== Planning | == Planning the Treatment Series == | ||
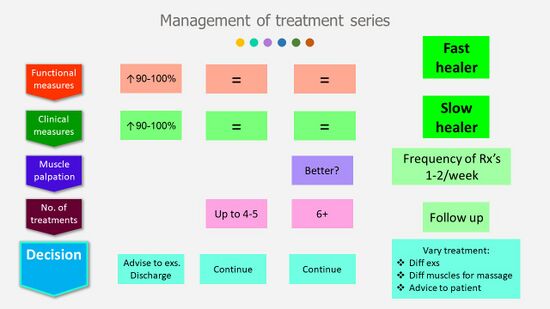
Management of the treatment series will be mostly determined by the functional and clinical measures (Figure | Management of the treatment series will be mostly determined by the functional and clinical measures (Figure 11). If there is a 90-100 percent improvement in these measures, patients can be discharged from therapy with advice to:<ref name=":0" /> | ||
* Continue with the stretch exercises to prevent deterioration of their condition | * Continue with the stretch exercises to prevent deterioration of their condition | ||
| Line 146: | Line 148: | ||
* Incorporating different muscles in the massage | * Incorporating different muscles in the massage | ||
* Adapting the advice to the patient | * Adapting the advice to the patient | ||
[[File:Management of the treatment series PHPS.jpg|frameless|550x550px]] | [[File:Management of the treatment series PHPS.jpg|frameless|550x550px]] | ||
'''Figure | '''Figure 11'''. Management of the Treatment Series <ref name=":0" /> | ||
On average, six to eight treatments provided at a frequency of | On average, six to eight treatments provided at a frequency of one to two times per week should be sufficient to alleviate symptoms of heel pain in individuals with PHPS.<ref name=":0" /><ref name=":4" /> Even if no improvement occurred in the functional and clinical measures after 4-5 treatments, treatment should be continued. <ref>Morrissey D, Cotchett M, J'Bari AS, Prior T, Griffiths IB, Rathleff MS, Gulle H, Vicenzino B, Barton CJ. [https://bjsm.bmj.com/content/bjsports/55/19/1106.full.pdf Management of plantar heel pain: a best practice guide informed by a systematic review, expert clinical reasoning and patient values.] British journal of sports medicine. 2021 Oct 1;55(19):1106-18.</ref> Change in the calf muscles with palpation (more pliable, less stiff, fewer painful areas) can also be used to measure improvement should there be no change in the functional or clinical measures after six treatments (Figure 11). If no improvement occurs and the patient reports worsening of the symptoms which cannot be attributed to treatment soreness, it is necessary to refer to a physician.<ref name=":0" /> | ||
Patients should be encouraged to return to function, including | Patients should be encouraged to return to function, including walking and a gradual return to sports. Research has shown an association between a lack of participation in regular exercise and PHPS, affirming that walking, running and sports are not risk factors for PHPS, but rather protective against it.<ref name=":4" /><ref>Van Leeuwen KD, Rogers J, Winzenberg T, van Middelkoop M. [https://bjsm.bmj.com/content/50/16/972.short Higher body mass index is associated with plantar fasciopathy/‘plantar fasciitis’: systematic review and meta-analysis of various clinical and imaging risk factors]. British journal of sports medicine. 2016 Aug 1;50(16):972-81. | ||
</ref> | </ref> | ||
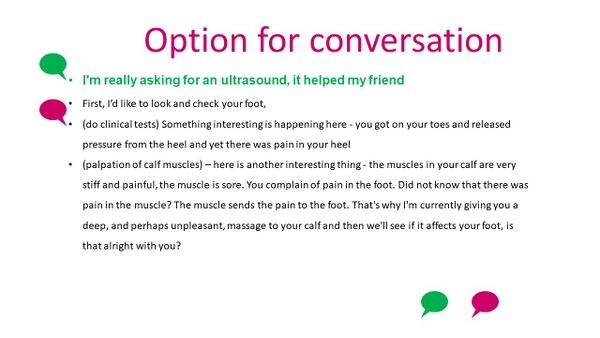
Patients often arrive at physiotherapy with ideas from friends/family of what is needed to alleviate their symptoms. Figure | Patients often arrive at physiotherapy with ideas from friends/family of what is needed to alleviate their symptoms. Figure 12 provides an example of a conversation that the therapist can have with a patient who is demanding treatment modalities that might have a limited effect on their condition.<ref name=":0" /> | ||
[[File:Option for conversation PHPS.jpg|frameless|600x600px]] | [[File:Option for conversation PHPS.jpg|frameless|600x600px]] | ||
'''Figure | '''Figure 12'''. Option for Conversation with a Patient<ref name=":0" /> | ||
== Conclusion == | == Conclusion == | ||
The series on PHPS has provided clinicians with:<ref name=":0" /> | The series on PHPS has provided clinicians with:<ref name=":0" /> | ||
* | * An assessment tool that that provides immediate and useful measures and is cost-free and easy to apply | ||
* | * A manual therapy intervention which includes deep friction massage and exercise | ||
* | * A self-exercise programme | ||
These tools provide pain relief and enable a return to function for the patient. | |||
== References == | == References == | ||
| Line 188: | Line 180: | ||
[[Category:Course Pages]] | [[Category:Course Pages]] | ||
[[Category:Musculoskeletal/Orthopaedics]] | [[Category:Musculoskeletal/Orthopaedics]] | ||
[[Category:Plus Content]] | |||
Latest revision as of 23:15, 15 January 2023
Original Editor - Merinda Rodseth based on the course by
Bernice Saban
Top Contributors - Merinda Rodseth, Wanda van Niekerk, Kim Jackson, Jess Bell, Olajumoke Ogunleye and Ewa Jaraczewska
Introduction[edit | edit source]
The application of the “new protocol” for plantar heel pain (PHP) will be discussed in three distinct parts:
- Assessment of the patient
- Planning of the initial session
- Planning of the treatment series
Patient Assessment[edit | edit source]
“Not only will a thorough subjective exam tell you what the problem(s) are, but also how to treat them” - Geoff Maitland
Communication plays an essential role in the assessment process and effective, competent clinical communication skills are key to high-quality healthcare.[1] Different communication techniques, such as motivational interviewing, also have positive effects on the outcomes of physiotherapy treatment.[2] Following the principles of motivational interviewing, communication with the patient should include: [3][4][5][6][7]
- Open questions
- Patient involvement
- Empathy
- Active listening
- Use of reflections
- Explanations during the interview
Assessment is one of the cornerstones of the physiotherapeutic approach.[8] While the principles of musculoskeletal assessment are universal, it is important to also focus specifically on the patient's complaint/area of concern, which in this instance is the heel.
The typical musculoskeletal assessment includes:[8][9]
- Subjective assessment (interview)
- Objective/physical examination

The interview should include (Figure 1):[3]
- Personal information
- Analysis of the symptoms to determine whether the condition is typical or atypical
- Differential diagnosis of the sources of heel pain, including systemic sources, yellow flags and red flags
- Functional measures including functional limitations
- General health
Typical questions asked in a thorough interview (subjective evaluation) include (Figure 2 and 3):[3][9][10]
- Areas of pain
- History of the complaint
- Behaviour of the symptoms (factors that provoke and ease symptoms, 24-hour behaviour)
- Functional difficulties
Figure 2. Heel Pain Specific Examination Form - Location, Pain and History
Figure 3. Heel Pain Specific Examination Form - Behaviour of the Symptoms
The interview is followed by the physical examination of the patient, which includes (Figures 4 and 5):[3]
- Physical measures
- For PHPS, these measures include the 3 heel pain tests previously discussed[11]
- Relevant additional tests to support the estimated diagnosis and whether the presentation is typical or atypical
- Investigation of other sources of heel pain, including the spine, systemic disease, yellow flags and red flags
Figure 4. Heel Pain Specific Examination Form - Physical Examination[3]
Figure 5. Heel Pain Specific Examination Form - Physical examination[3]
Completion of the examination includes (Figure 6):[3]
- Setting of functional and clinical treatment goals[12]
- Planning of the treatment interventions - manual therapy and exercises
- Explanations to the patient including:[13]
- Information about PHPS
- Recommendations and advice
- Answering questions
- Information about the treatment plan
Figure 6. Completion of the Examination [3]
Planning of the Initial Sessions[edit | edit source]
Each treatment session will include 3 main sections:
- Assessment
- Manual therapy
- Exercise therapy
The first treatment session should include:
- The interview and physical examination, including the 3 clinical tests[11] and palpation of the calf muscles[11][14]
- Treatment - deep friction massage of the calf muscles for at least 10 minutes[14]
- Reassessment using the 3 clinical tests
- Home exercise - the lunge stretch exercise [14]
For the second treatment session, it is necessary to establish “what has changed” since the previous session with the patient through reassessment. From here on, each treatment should be customised for the patient in order to comprehensively address their needs.
The second treatment will include an assessment of the functional measures as reported by the patient (Figure 7). These generally include the level, frequency and duration of the pain with “first steps in the morning”, followed by other measures previously reported by the patient.[3]
Figure 7. Functional Measures[3]
Following the reassessment of the functional measures, the clinical measures (3 clinical tests) should also be reassessed based on the (Figure 8):
- Level of pain
- Number of repetitions
- Time standing
Figure 8. Reassessment of the Clinical Measures [3]
A summary of the steps to follow during the second treatment session is provided in Figure 9:
Figure 9. Second Treatment Session [3]
All follow-up sessions should follow the sequence of the first session while progressing the exercises as necessary (Figure 10).
Figure 10. Approach to Follow-Up Visits [3]
Planning the Treatment Series[edit | edit source]
Management of the treatment series will be mostly determined by the functional and clinical measures (Figure 11). If there is a 90-100 percent improvement in these measures, patients can be discharged from therapy with advice to:[3]
- Continue with the stretch exercises to prevent deterioration of their condition
- Incorporate self-massage of the calf muscles
It is also important to note that the effect of the deep friction massage and the stretch exercises might not be immediate as it takes time for the tissues to change and adapt. Treatments can also be varied as the patient progresses through the treatment series by:[3]
- Including different exercises
- Incorporating different muscles in the massage
- Adapting the advice to the patient
Figure 11. Management of the Treatment Series [3]
On average, six to eight treatments provided at a frequency of one to two times per week should be sufficient to alleviate symptoms of heel pain in individuals with PHPS.[3][14] Even if no improvement occurred in the functional and clinical measures after 4-5 treatments, treatment should be continued. [15] Change in the calf muscles with palpation (more pliable, less stiff, fewer painful areas) can also be used to measure improvement should there be no change in the functional or clinical measures after six treatments (Figure 11). If no improvement occurs and the patient reports worsening of the symptoms which cannot be attributed to treatment soreness, it is necessary to refer to a physician.[3]
Patients should be encouraged to return to function, including walking and a gradual return to sports. Research has shown an association between a lack of participation in regular exercise and PHPS, affirming that walking, running and sports are not risk factors for PHPS, but rather protective against it.[14][16]
Patients often arrive at physiotherapy with ideas from friends/family of what is needed to alleviate their symptoms. Figure 12 provides an example of a conversation that the therapist can have with a patient who is demanding treatment modalities that might have a limited effect on their condition.[3]
Figure 12. Option for Conversation with a Patient[3]
Conclusion[edit | edit source]
The series on PHPS has provided clinicians with:[3]
- An assessment tool that that provides immediate and useful measures and is cost-free and easy to apply
- A manual therapy intervention which includes deep friction massage and exercise
- A self-exercise programme
These tools provide pain relief and enable a return to function for the patient.
References[edit | edit source]
- ↑ Iversen ED, Wolderslund MO, Kofoed PE, Gulbrandsen P, Poulsen H, Cold S et al. Codebook for rating clinical communication skills based on the Calgary-Cambridge Guide. BMC Med Educ. 2020;20(1):140.
- ↑ Hiller A, Delany C. Communication in physiotherapy: Challenging established theoretical approaches. Manipulating Practices: A Critical Physiotherapy Reader. 2018:308-33.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 3.17 3.18 3.19 3.20 3.21 Bernice Saban. Application of the New Protocol for Plantar Heel Pain. Plus Course. 2021
- ↑ Norris M, Eva G, Fortune J, Frater T, Breckon J. Educating undergraduate occupational therapy and physiotherapy students in motivational interviewing: the student perspective. BMC medical education. 2019 Dec;19(1):1-7.
- ↑ Pace BT, Dembe A, Soma CS, Baldwin SA, Atkins DC, Imel ZE. A multivariate meta-analysis of motivational interviewing process and outcome. Psychology of Addictive Behaviors. 2017 Aug;31(5):524.
- ↑ Hashim MJ. Patient-centered communication: basic skills. American family physician. 2017 Jan 1;95(1):29-34.
- ↑ Diener I. Physiotherapy support for self-management of persisting musculoskeletal pain disorders. South African Journal of Physiotherapy. 2021 Oct 29;77(1):1564.
- ↑ 8.0 8.1 Hengeveld E (ed.), Banks K (ed.), Maitland GD. Maitland's peripheral manipulation. 4th ed. Philadelphia: Elsevier/Butterworth Heinemann; 2005.
- ↑ 9.0 9.1 Alazzawi S, Sukeik M, King D, Vemulapalli K. Foot and ankle history and clinical examination: A guide to everyday practice. World journal of orthopedics. 2017 Jan 18;8(1):21
- ↑ Killens D. Mobilizing the Myofascial System: A Clinical Guide to Assessment and Treatment of Myofascial Dysfunctions. Edinburgh: Handspring Publishing; 2018.
- ↑ 11.0 11.1 11.2 Saban B, Masharawi Y. Three single leg standing tests for clinical assessment of chronic plantar heel pain syndrome: static stance, half-squat and heel rise. Physiotherapy. 2017 Jun 1;103(2):237-44.
- ↑ Stevens A, Köke A, van der Weijden T, Beurskens A. The development of a patient-specific method for physiotherapy goal setting: a user-centered design. Disability and rehabilitation. 2018 Aug 14;40(17):2048-55.
- ↑ Cotchett M, Rathleff MS, Dilnot M, Landorf KB, Morrissey D, Barton C. Lived experience and attitudes of people with plantar heel pain: a qualitative exploration. Journal of foot and ankle research. 2020 Dec;13(1):1-9.
- ↑ 14.0 14.1 14.2 14.3 14.4 Saban B, Deutscher D, Ziv T. Deep massage to posterior calf muscles in combination with neural mobilization exercises as a treatment for heel pain: a pilot randomized clinical trial. Manual therapy. 2014 Apr 1;19(2):102-8.
- ↑ Morrissey D, Cotchett M, J'Bari AS, Prior T, Griffiths IB, Rathleff MS, Gulle H, Vicenzino B, Barton CJ. Management of plantar heel pain: a best practice guide informed by a systematic review, expert clinical reasoning and patient values. British journal of sports medicine. 2021 Oct 1;55(19):1106-18.
- ↑ Van Leeuwen KD, Rogers J, Winzenberg T, van Middelkoop M. Higher body mass index is associated with plantar fasciopathy/‘plantar fasciitis’: systematic review and meta-analysis of various clinical and imaging risk factors. British journal of sports medicine. 2016 Aug 1;50(16):972-81.