Subjective Assessment of the Equine Patient: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) m (Text replacement - "Plus ." to "Plus.") |
||
| (36 intermediate revisions by 3 users not shown) | |||
| Line 2: | Line 2: | ||
== Introduction == | == Introduction == | ||
Equine physiotherapists are now an established part of the multidisciplinary team (MDT) that looks after equine athletes and their riders. Equine therapists work closely with this team and usually receive referrals from a veterinarian.<ref name=":1">McGowan CM, Stubbs NC, Jull GA. Equine physiotherapy: a comparative view of the science underlying the profession. Equine veterinary journal. 2007 Jan;39(1):90-4.</ref><ref name=":4">Paulekas R, Haussler KK. Principles and practice of therapeutic exercise for horses. Journal of equine veterinary science. 2009 Dec 1;29(12):870-93.</ref> The aim of the equine therapist is to conduct a thorough assessment in order to identify pain or loss of function caused by pain, injury, disorders or disability.[[File:Gallop.jpg|thumb]] <ref name=":1" /> | |||
The following skills are considered useful for equine physiotherapists:<ref name=":6">Goff L. Physiotherapy Assessment for the Equine Athlete. Vet Clin North Am Equine Pract. 2016 Apr;32(1):31-47.</ref> | |||
* The ability to communicate well with a horse's owner, handler and trainer | * The ability to communicate well with a horse's owner, handler and trainer | ||
* Excellent observation skills (of the horse in motion and at rest) | |||
* Good understanding of the anatomy, functional anatomy, and biomechanics of the horse | |||
* Being able to carry out functional movement tests, having effective palpation skills and being able to interpret the findings of an equine assessment | |||
== Subjective Assessment == | |||
When working with horses, the ability to obtain subjective history is limited - it is very difficult to determine the severity, irritability, nature (i.e. SIN) of a condition, its 24- hour pattern and the exact area of pain/ discomfort. [[File:Equine Subjective Assessment.jpg|center|frameless|alt=|400x400px]]The following subjective information can also help the therapist to develop his / her treatment plan:<ref name=":7">Chelin S. Assessment of the Equine Patient Course. Plus , 2021.</ref> | |||
*'''Background information''': It is important to have background information (age, gender etc) so that you can identify the horse and contact the MDT for information | |||
*'''Discipline, training history, the reason for referral:''' These areas provide clues about the type of injury, mechanism of injury and cause of injury (i.e. over-training) | |||
*'''Present medical history:''' It is important to consider what the problem is and how it has been assessed. What treatment has been given thus far and how has the horse responded? | |||
*'''Past medical history:''' This provides clues as to whether or not a previous injury may be associated with the horse's current issue. It also indicates what treatments the horse responds to and if the horse has been provided with sufficient rehabilitation | |||
*'''Special questions /red flags''': These are similar to those seen in [[An Introduction to Red Flags in Serious Pathology|human patients]] such as a sudden weight loss, general health issues, respiratory conditions etc | |||
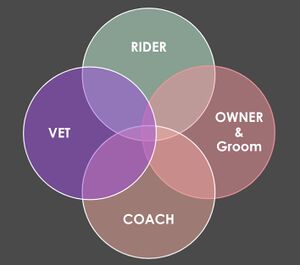
When working with horses, the ability to obtain subjective history is limited - it is very difficult to determine the severity, irritability, nature (SIN) of a condition, its 24- hour pattern and the exact area of pain/ discomfort. Unlike in human physiotherapy, you cannot interview an equine patient, so the animal therapist often has to interview the wider team to find out all the relevant information, including the:<ref name=":7" | [[File:Equine venn diagram.jpg|right|frameless]] | ||
Unlike in human physiotherapy, you cannot interview an equine patient, so the animal therapist often has to interview the wider team to find out all the relevant information, including the:<ref name=":7" /> | |||
# Rider - what are they feeling during training? | # Rider - what are they feeling during training? | ||
# Coach - what they are seeing during training? | # Coach - what they are seeing during training? | ||
# Owner and Groom - how is the horse at home and has it developed any abnormal behaviours? | # Owner and Groom - how is the horse at home and has it developed any abnormal behaviours? | ||
# Veterinarian and other medical professionals - what | # Veterinarian and other medical professionals - what has been found on examination and have there been any other investigations? | ||
=== Age === | |||
Age gives us clues about potential pathologies and should be considered in a differential diagnosis.<ref name=":7" /> | |||
Age gives us clues about potential pathologies and | |||
==== Young Horses (2-6 years) ==== | |||
* May present with developmental problems (e.g. osteochondrosis dissecans<ref>Naccache F, Metzger J, Distl O. Genetic risk factors for osteochondrosis in various horse breeds. Equine Vet J. 2018;50(5):556-63.</ref>) | |||
* Young horses are still developing soft tissue structures, so injuries may be related to poor motor control or a lack of adequate conditioning of the soft tissue structures to cope with work demands | |||
* Competing racehorses are under huge stress - young thoroughbred horses have been shown to experience a significant number of physiological and anatomical adaptations in response to exercise training<ref>Miglio A, Cappelli K, Capomaccio S, Mecocci S, Silvestrelli M, Antognoni MT. Metabolic and Biomolecular Changes Induced by Incremental Long-Term Training in Young Thoroughbred Racehorses during First Workout Season. Animals (Basel). 2020;10(2):317.</ref> | * Competing racehorses are under huge stress - young thoroughbred horses have been shown to experience a significant number of physiological and anatomical adaptations in response to exercise training<ref>Miglio A, Cappelli K, Capomaccio S, Mecocci S, Silvestrelli M, Antognoni MT. Metabolic and Biomolecular Changes Induced by Incremental Long-Term Training in Young Thoroughbred Racehorses during First Workout Season. Animals (Basel). 2020;10(2):317.</ref> | ||
==== Mid-Aged Horses (7-15 years) ==== | |||
* Sport horses are often competing at their peak at this age, so soft tissue injuries due to overuse are more common<ref name=":7" /> - ageing and exercise are considered important risk factors for tendon injury<ref>Dakin SG. A review of the healing processes in equine superficial digital flexor tendinopathy. Equine vet. Educ. 2017;29(9):516-20.</ref> | * Sport horses are often competing at their peak at this age, so soft tissue injuries due to overuse are more common<ref name=":7" /> - ageing and exercise are considered important risk factors for tendon injury<ref>Dakin SG. A review of the healing processes in equine superficial digital flexor tendinopathy. Equine vet. Educ. 2017;29(9):516-20.</ref> | ||
* Biomechanical problems can also play a role in soft tissue injuries at this stage | |||
* Degenerative joint disease (DJD) may already be present in some horses at this age especially when the animal has pre-existing developmental joint abnormalities | |||
==== Older Horses (15-20 years) ==== | |||
* Wear and tear is common especially in joints (e.g. DJD / arthritis) | |||
* Wear and tear is common especially in joints ( | |||
=== | === Gender === | ||
Hormonal changes may mimic behavioural changes that are associated with musculoskeletal pain | Hormonal changes may mimic behavioural changes that are associated with musculoskeletal pain. Common behavioural problems can occur in performance mares when they exhibit heat or oestrus.<ref>Crabtree JR. A review of oestrus suppression techniques in mares. Equine Vet Educ. 2021.</ref> Mares begin periods of heat due to increasing day length. In general, these periods of heat last five to seven days out of a 21-day cycle. Clinical signs of oestrus in mares that can affect performance include attitude changes, tail swishing, difficulty during training sessions, squealing, horsing, excessive urination, kicking, a decrease in performance and colic like pain that is associated with ovulation.<ref>Wessex Equine. Behavioural problems in performance mares. Available from: http://wessexequine.co.uk/wp-content/uploads/2016/07/Hormonal-problems-in-mares-.pdf (accessed 19/4/2021).</ref> | ||
Asking the owner or rider about previous problems with oestrus, or whether there appears to be a regular monthly pattern to the pain or if the mare is experiencing performance-related symptoms can be helpful.{{#ev:youtube|l2BeIZzfnBc}}<ref>Kim Hallin. Why are Mares so "Mareish"? Available from: https://www.youtube.com/watch?v=l2BeIZzfnBc [last accessed 21/4/2021]</ref> | |||
=== | === Length Of Ownership === | ||
Horses may often change hands a number of times throughout their life. However, during these changes of ownership, it is very rare for a horse's entire medical history to be passed on.<ref name=":0" /> Therapists are guided by pre-purchase vetting but unfortunately, not all previous musculoskeletal injuries will be obvious during these assessments.<ref name=":7" /> One of the most effective methods to identify musculoskeletal pain or discomfort is a horse's behaviour. New owners may not, however, yet know what ‘normal’ behaviour is for their horse.<ref name=":7" /> | |||
=== Discipline and Training History === | |||
[[File:Horse jumping.jpeg|right|frameless|326x326px]] | |||
'''Discipline and Level -''' It is important to understand a horse's training level, what discipline it competes in or the type of work it does as these factors may affect symptomatology and help establish a diagnosis. They may also provide clues about the mechanism and severity of the injury.<ref name=":7" /><ref name=":0" /> | |||
= | '''Last Competition -''' Finding out about a horse's last competition will provide the therapist with an understanding of:<ref name=":7" /> | ||
* When the horse was (possibly) last put under great strain | |||
* How long the horse has been out of action | |||
[[File:Dressage.jpeg|right|frameless]] | |||
'''Training Programme:''' It is also important to gain an understanding of a horse's training programme. This will enable the therapist to determine how often the horse is working and what it is doing. Questions to consider include: | |||
* Does the horse cross-train? | |||
* | * Does it participate in a range of work / activities (e.g. pole work, jumping, flatwork, hill work or track work and hacking)<ref name=":7" /> | ||
You may not have access to this history in horses who are newly acquired, but details such as the length of a horse's racing career can provide additional clues about the amount of wear and tear a horse may have experienced.<ref name=":0" /> | |||
=== | === Present Medical History === | ||
It is important to find out:<ref name=":7" /> | It is important to establish the general area and nature of a horse's symptoms during a subjective interview.<ref name=":0" /> You will need to find out:<ref name=":7" /> | ||
* | * The horse's main complaint (SIN) | ||
* | * Which behavioural issues have caused the owner to contact an animal therapist | ||
* How long the complaint | * How long the complaint / issue has been present | ||
* | ** Also find out if it has improved, deteriorated or remained unchanged | ||
* | * What caused the issue in the owner's opinion - remember that this is entirely subjective as it is based on his / her interpretation of events | ||
* | * Has a veterinarian seen the horse for this issue - and if so, were there any investigations, is there a diagnosis, has the horse been prescribed any medications and, if so, for how long? | ||
* The 24-hour pattern - does the horse worsen or improve with work? Is the horse worse on walking out of the stable in the morning? How long does it take for the horse to improve? | |||
* Which other professionals (e.g saddle fitter, dentist, chiropractor etc) are involved in the horses' care - what have they done and how have these interventions helped? | |||
=== | === Past Medical History === | ||
Information about a horse's medical history may not always available | Information about a horse's medical history may help you to identify potential presenting conditions, but it is not always available or accurate. Where possible it is important to ask:<ref name=":7" /> | ||
* What veterinary | * What veterinary treatments have the horse had? | ||
* Was there a pre-purchase vetting? | * Was there a pre-purchase vetting? | ||
* What was picked up on this pre-purchase vetting? | * What was picked up on this pre-purchase vetting? | ||
''' | '''Pre-purchase vetting''' refers to the comprehensive assessment of a horse by a veterinarian before a horse is purchased. It typically includes a general health check, gait assessment, examination of the horse performing strenuous exercise, a re-assessment 30 minutes post-exercise and finally another trotting assessment.<ref name=":8">Equine World UK. Vetting a horse. Available from: https://equine-world.co.uk/info/buying-loaning-selling-horses/buying-a-horse/vetting-a-horse (accessed 19/4/2021).</ref> X-rays may also be taken during more extensive vettings.<ref name=":7" /> | ||
The price of the horse often determines if there is vetting and how extensive it is. Some horses (i.e. those with great potential or expensive horses) may be x-rayed every few years as a preventative measure. The equine therapist should also try to find out if a veterinarian has ever recommended any diagnostic tests for a horse that were not actually undertaken as these can provide clues to potential causes of dysfunction.<ref name=":7" /> | |||
{{#ev:youtube|9JDfrYhXw9Y}}<ref>SmartPak. Equine Pre-Purchase Exams. Available from: https://www.youtube.com/watch?v=9JDfrYhXw9Y [last accessed 21/4/2021]</ref> | |||
=== | === Red Flags and Special Questions === | ||
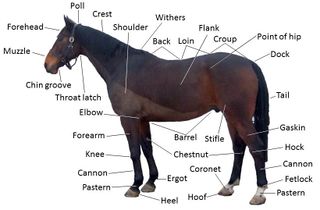
[[File:Points of a horse.jpg|thumb|320x320px]]Red flags are signs or symptoms that suggest serious pathology may be present.<ref>Finucane LM, Downie A, Mercer C, Greenhalgh SM, Boissonnault WG, Pool-Goudzwaard AL et al. International Framework for Red Flags for Potential Serious Spinal Pathologies. J Orthop Sports Phys Ther. 2020;50(7):350-72.</ref> | [[File:Points of a horse.jpg|thumb|320x320px]]Red flags are signs or symptoms that suggest serious pathology may be present.<ref>Finucane LM, Downie A, Mercer C, Greenhalgh SM, Boissonnault WG, Pool-Goudzwaard AL et al. International Framework for Red Flags for Potential Serious Spinal Pathologies. J Orthop Sports Phys Ther. 2020;50(7):350-72.</ref> | ||
The horse's general health should be considered, including if there could be:<ref name=":7" /> | |||
* Metabolic diseases such as Cushing’s | |||
* | |||
== | * Respiratory diseases such as COPD | ||
It is also beneficial to find out what medications / supplements the horse may be on. Remember that your subjective assessment should give you an indication of:<ref name=":7" /> | |||
* The source of the problem | |||
* Whether something is not making sense in the history - this may indicate that a referral is necessary | |||
Horses who require regular treatment by a range of therapists to remain comfortable should:<ref name=":0">Zikmann P. Assessment and Management of the Equine Spine Course. Plus. 2021.</ref> | |||
* Have a history of being recently reviewed by a veterinarian or should be referred for review in order to check that there are no underlying pathologies | |||
* Should be reassessed for other causes of pain such as saddle / bridle / bit fit, teeth problems or issues with foot balance | |||
Where possible, it is important to try to corroborate any information obtained from the owner with the relevant professional. You should obtain a history from the horse's veterinarian, as well as consent for you to treat the horse. In instances where a change in the horse's behaviour is the main complaint, it can be useful to talk with the riding instructor in addition to the owner. If it is indicated, it is also useful to communicate with the horse's farrier or dentist in order to hear their opinions on the horse's feet / teeth.<ref name=":0" /> | |||
== | == Summary == | ||
* It is difficult to obtain a subjective history directly from your equine patients | |||
* You can, however, obtain a significant amount of information by working closely with the horse's entire team, including the coach, rider, owner, groom and veterinarian | |||
* You will structure your [[Objective Assessment of the Equine Patient|objective assessment]] based on your findings in the subjective interview | |||
== References == | == References == | ||
| Line 350: | Line 112: | ||
[[Category:Animal Physiotherapy]] | [[Category:Animal Physiotherapy]] | ||
[[Category:Course Pages]] | [[Category:Course Pages]] | ||
[[Category:Plus Content]] | |||
Latest revision as of 11:49, 18 August 2022
Introduction[edit | edit source]
Equine physiotherapists are now an established part of the multidisciplinary team (MDT) that looks after equine athletes and their riders. Equine therapists work closely with this team and usually receive referrals from a veterinarian.[1][2] The aim of the equine therapist is to conduct a thorough assessment in order to identify pain or loss of function caused by pain, injury, disorders or disability.
The following skills are considered useful for equine physiotherapists:[3]
- The ability to communicate well with a horse's owner, handler and trainer
- Excellent observation skills (of the horse in motion and at rest)
- Good understanding of the anatomy, functional anatomy, and biomechanics of the horse
- Being able to carry out functional movement tests, having effective palpation skills and being able to interpret the findings of an equine assessment
Subjective Assessment[edit | edit source]
When working with horses, the ability to obtain subjective history is limited - it is very difficult to determine the severity, irritability, nature (i.e. SIN) of a condition, its 24- hour pattern and the exact area of pain/ discomfort.
The following subjective information can also help the therapist to develop his / her treatment plan:[4]
- Background information: It is important to have background information (age, gender etc) so that you can identify the horse and contact the MDT for information
- Discipline, training history, the reason for referral: These areas provide clues about the type of injury, mechanism of injury and cause of injury (i.e. over-training)
- Present medical history: It is important to consider what the problem is and how it has been assessed. What treatment has been given thus far and how has the horse responded?
- Past medical history: This provides clues as to whether or not a previous injury may be associated with the horse's current issue. It also indicates what treatments the horse responds to and if the horse has been provided with sufficient rehabilitation
- Special questions /red flags: These are similar to those seen in human patients such as a sudden weight loss, general health issues, respiratory conditions etc
Unlike in human physiotherapy, you cannot interview an equine patient, so the animal therapist often has to interview the wider team to find out all the relevant information, including the:[4]
- Rider - what are they feeling during training?
- Coach - what they are seeing during training?
- Owner and Groom - how is the horse at home and has it developed any abnormal behaviours?
- Veterinarian and other medical professionals - what has been found on examination and have there been any other investigations?
Age[edit | edit source]
Age gives us clues about potential pathologies and should be considered in a differential diagnosis.[4]
Young Horses (2-6 years)[edit | edit source]
- May present with developmental problems (e.g. osteochondrosis dissecans[5])
- Young horses are still developing soft tissue structures, so injuries may be related to poor motor control or a lack of adequate conditioning of the soft tissue structures to cope with work demands
- Competing racehorses are under huge stress - young thoroughbred horses have been shown to experience a significant number of physiological and anatomical adaptations in response to exercise training[6]
Mid-Aged Horses (7-15 years)[edit | edit source]
- Sport horses are often competing at their peak at this age, so soft tissue injuries due to overuse are more common[4] - ageing and exercise are considered important risk factors for tendon injury[7]
- Biomechanical problems can also play a role in soft tissue injuries at this stage
- Degenerative joint disease (DJD) may already be present in some horses at this age especially when the animal has pre-existing developmental joint abnormalities
Older Horses (15-20 years)[edit | edit source]
- Wear and tear is common especially in joints (e.g. DJD / arthritis)
Gender[edit | edit source]
Hormonal changes may mimic behavioural changes that are associated with musculoskeletal pain. Common behavioural problems can occur in performance mares when they exhibit heat or oestrus.[8] Mares begin periods of heat due to increasing day length. In general, these periods of heat last five to seven days out of a 21-day cycle. Clinical signs of oestrus in mares that can affect performance include attitude changes, tail swishing, difficulty during training sessions, squealing, horsing, excessive urination, kicking, a decrease in performance and colic like pain that is associated with ovulation.[9]
Asking the owner or rider about previous problems with oestrus, or whether there appears to be a regular monthly pattern to the pain or if the mare is experiencing performance-related symptoms can be helpful.
Length Of Ownership[edit | edit source]
Horses may often change hands a number of times throughout their life. However, during these changes of ownership, it is very rare for a horse's entire medical history to be passed on.[11] Therapists are guided by pre-purchase vetting but unfortunately, not all previous musculoskeletal injuries will be obvious during these assessments.[4] One of the most effective methods to identify musculoskeletal pain or discomfort is a horse's behaviour. New owners may not, however, yet know what ‘normal’ behaviour is for their horse.[4]
Discipline and Training History[edit | edit source]
Discipline and Level - It is important to understand a horse's training level, what discipline it competes in or the type of work it does as these factors may affect symptomatology and help establish a diagnosis. They may also provide clues about the mechanism and severity of the injury.[4][11]
Last Competition - Finding out about a horse's last competition will provide the therapist with an understanding of:[4]
- When the horse was (possibly) last put under great strain
- How long the horse has been out of action
Training Programme: It is also important to gain an understanding of a horse's training programme. This will enable the therapist to determine how often the horse is working and what it is doing. Questions to consider include:
- Does the horse cross-train?
- Does it participate in a range of work / activities (e.g. pole work, jumping, flatwork, hill work or track work and hacking)[4]
You may not have access to this history in horses who are newly acquired, but details such as the length of a horse's racing career can provide additional clues about the amount of wear and tear a horse may have experienced.[11]
Present Medical History[edit | edit source]
It is important to establish the general area and nature of a horse's symptoms during a subjective interview.[11] You will need to find out:[4]
- The horse's main complaint (SIN)
- Which behavioural issues have caused the owner to contact an animal therapist
- How long the complaint / issue has been present
- Also find out if it has improved, deteriorated or remained unchanged
- What caused the issue in the owner's opinion - remember that this is entirely subjective as it is based on his / her interpretation of events
- Has a veterinarian seen the horse for this issue - and if so, were there any investigations, is there a diagnosis, has the horse been prescribed any medications and, if so, for how long?
- The 24-hour pattern - does the horse worsen or improve with work? Is the horse worse on walking out of the stable in the morning? How long does it take for the horse to improve?
- Which other professionals (e.g saddle fitter, dentist, chiropractor etc) are involved in the horses' care - what have they done and how have these interventions helped?
Past Medical History[edit | edit source]
Information about a horse's medical history may help you to identify potential presenting conditions, but it is not always available or accurate. Where possible it is important to ask:[4]
- What veterinary treatments have the horse had?
- Was there a pre-purchase vetting?
- What was picked up on this pre-purchase vetting?
Pre-purchase vetting refers to the comprehensive assessment of a horse by a veterinarian before a horse is purchased. It typically includes a general health check, gait assessment, examination of the horse performing strenuous exercise, a re-assessment 30 minutes post-exercise and finally another trotting assessment.[12] X-rays may also be taken during more extensive vettings.[4]
The price of the horse often determines if there is vetting and how extensive it is. Some horses (i.e. those with great potential or expensive horses) may be x-rayed every few years as a preventative measure. The equine therapist should also try to find out if a veterinarian has ever recommended any diagnostic tests for a horse that were not actually undertaken as these can provide clues to potential causes of dysfunction.[4]
Red Flags and Special Questions[edit | edit source]
Red flags are signs or symptoms that suggest serious pathology may be present.[14]
The horse's general health should be considered, including if there could be:[4]
- Metabolic diseases such as Cushing’s
- Respiratory diseases such as COPD
It is also beneficial to find out what medications / supplements the horse may be on. Remember that your subjective assessment should give you an indication of:[4]
- The source of the problem
- Whether something is not making sense in the history - this may indicate that a referral is necessary
Horses who require regular treatment by a range of therapists to remain comfortable should:[11]
- Have a history of being recently reviewed by a veterinarian or should be referred for review in order to check that there are no underlying pathologies
- Should be reassessed for other causes of pain such as saddle / bridle / bit fit, teeth problems or issues with foot balance
Where possible, it is important to try to corroborate any information obtained from the owner with the relevant professional. You should obtain a history from the horse's veterinarian, as well as consent for you to treat the horse. In instances where a change in the horse's behaviour is the main complaint, it can be useful to talk with the riding instructor in addition to the owner. If it is indicated, it is also useful to communicate with the horse's farrier or dentist in order to hear their opinions on the horse's feet / teeth.[11]
Summary[edit | edit source]
- It is difficult to obtain a subjective history directly from your equine patients
- You can, however, obtain a significant amount of information by working closely with the horse's entire team, including the coach, rider, owner, groom and veterinarian
- You will structure your objective assessment based on your findings in the subjective interview
References[edit | edit source]
- ↑ 1.0 1.1 McGowan CM, Stubbs NC, Jull GA. Equine physiotherapy: a comparative view of the science underlying the profession. Equine veterinary journal. 2007 Jan;39(1):90-4.
- ↑ Paulekas R, Haussler KK. Principles and practice of therapeutic exercise for horses. Journal of equine veterinary science. 2009 Dec 1;29(12):870-93.
- ↑ Goff L. Physiotherapy Assessment for the Equine Athlete. Vet Clin North Am Equine Pract. 2016 Apr;32(1):31-47.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 Chelin S. Assessment of the Equine Patient Course. Plus , 2021.
- ↑ Naccache F, Metzger J, Distl O. Genetic risk factors for osteochondrosis in various horse breeds. Equine Vet J. 2018;50(5):556-63.
- ↑ Miglio A, Cappelli K, Capomaccio S, Mecocci S, Silvestrelli M, Antognoni MT. Metabolic and Biomolecular Changes Induced by Incremental Long-Term Training in Young Thoroughbred Racehorses during First Workout Season. Animals (Basel). 2020;10(2):317.
- ↑ Dakin SG. A review of the healing processes in equine superficial digital flexor tendinopathy. Equine vet. Educ. 2017;29(9):516-20.
- ↑ Crabtree JR. A review of oestrus suppression techniques in mares. Equine Vet Educ. 2021.
- ↑ Wessex Equine. Behavioural problems in performance mares. Available from: http://wessexequine.co.uk/wp-content/uploads/2016/07/Hormonal-problems-in-mares-.pdf (accessed 19/4/2021).
- ↑ Kim Hallin. Why are Mares so "Mareish"? Available from: https://www.youtube.com/watch?v=l2BeIZzfnBc [last accessed 21/4/2021]
- ↑ 11.0 11.1 11.2 11.3 11.4 11.5 Zikmann P. Assessment and Management of the Equine Spine Course. Plus. 2021.
- ↑ Equine World UK. Vetting a horse. Available from: https://equine-world.co.uk/info/buying-loaning-selling-horses/buying-a-horse/vetting-a-horse (accessed 19/4/2021).
- ↑ SmartPak. Equine Pre-Purchase Exams. Available from: https://www.youtube.com/watch?v=9JDfrYhXw9Y [last accessed 21/4/2021]
- ↑ Finucane LM, Downie A, Mercer C, Greenhalgh SM, Boissonnault WG, Pool-Goudzwaard AL et al. International Framework for Red Flags for Potential Serious Spinal Pathologies. J Orthop Sports Phys Ther. 2020;50(7):350-72.