Introduction to Therapeutic Exercise: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) m (Text replacement - "Plus ." to "Plus.") |
||
| (35 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Jess Bell|Jess Bell]] based on the course by [https://members.physio-pedia.com/course_tutor/richard-jackson/ Richard Jackson]<br> | <div class="editorbox"> '''Original Editor '''- [[User:Jess Bell|Jess Bell]] based on the course by [https://members.physio-pedia.com/course_tutor/richard-jackson/ Richard Jackson]<br> | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== Introduction == | == Introduction == | ||
When considering exercise prescription in physiotherapy practice, it is important to understand the difference between therapeutic exercise and general exercise. General exercise is essentially a “work out”. It is exercise for wellness, overall health, appearance, fun, leisure etc.<ref name=":0">Jackson R. Therapeutic Exercise Course. | When considering exercise prescription in physiotherapy practice, it is important to understand the difference between therapeutic exercise and general exercise. General exercise is essentially a “work out”. It is exercise for wellness, overall health, appearance, fun, leisure etc.<ref name=":0">Jackson R. Therapeutic Exercise Course. Plus. 2022.</ref> | ||
Therapeutic exercise is specifically for individuals who have a physical problem / impairment, which is often painful.<ref name=":0" /> | Therapeutic exercise is specifically for individuals who have a physical problem / impairment, which is often painful.<ref name=":0" /><blockquote>“Therapeutic exercise is distinguishable from other forms of recreation because it is a purposeful, body-building activity, often prescribed by experts [...], drawing on their knowledge of bodily function to engage in a powerful form of anatomo-politics”.<ref>Nicholls D, Jachyra P, Gibson BE, Fusco C, Setchell J. Keep fit: marginal ideas in contemporary therapeutic exercise. Qualitative Research in Sport, Exercise and Health. 2018;10(4):400-11. </ref></blockquote>Rehabilitation professionals must be able to assess, analyse, and determine the cause of a client’s pain or impairment. Exercises are then prescribed in order to address deficits in:<ref name=":0" /> | ||
“Therapeutic exercise is distinguishable from other forms of recreation because it is a purposeful, body-building activity, often prescribed by experts [...], drawing on their knowledge of bodily function to engage in a powerful form of anatomo-politics”.<ref>Nicholls D, Jachyra P, Gibson BE, Fusco C, Setchell J. Keep fit: marginal ideas in contemporary therapeutic exercise. Qualitative Research in Sport, Exercise and Health. 2018;10(4):400-11. </ref> | |||
Rehabilitation professionals must be able to assess, analyse, and determine | |||
* Mobility / flexibility | * Mobility / flexibility | ||
| Line 20: | Line 14: | ||
== '''Why Include Therapeutic Exercise in a Treatment Plan?''' == | == '''Why Include Therapeutic Exercise in a Treatment Plan?''' == | ||
Exercise interventions are beneficial as they enable individuals to self-manage their symptoms.<ref name=":0" /> Moreover, there is a large body of research to support its use in clinical practice.<ref>Maestroni L, Read P, Bishop C, Papadopoulos K, Suchomel TJ, Comfort P et al. The benefits of strength training on musculoskeletal system health: practical applications for interdisciplinary care. Sports Med. 2020;50(8):1431-50. </ref><ref>Prall J, Ross M. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6509454/ The management of work-related musculoskeletal injuries in an occupational health setting: the role of the physical therapist]. ''J Exerc Rehabil''. 2019;15(2):193-9. </ref> <ref name=":1">Bielecki JE, Tadi P. Therapeutic Exercise. [Updated 2021 Sep 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK555914/</ref> | |||
* Research supports the use of exercise | * Research supports the use of exercise interventions for long-term changes when compared to manual therapy alone | ||
* Exercise is supported over | ** A systematic review by Lin et al.<ref name=":5">Lin I, Wiles L, Waller R, Goucke R, Nagree Y, Gibberd M et al. [https://bjsm.bmj.com/content/54/2/79.full What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: systematic review]. Br J Sports Med. 2020;54(2):79-86. </ref> appraised 44 clinical practice guidelines for musculoskeletal pain conditions. They found that exercise was recommended in all guidelines. However, when manual therapy is utilised, it should be used alongside other interventions (i.e. exercise, psychological therapy, information / education, activity advice).<ref name=":5" /> | ||
Table 1 provides | * Exercise is supported over other therapeutic interventions<ref name=":0" /> | ||
== Terminology == | |||
Table 1 provides a list of terms that are often used when discussing therapeutic exercise. | |||
{| class="wikitable" | {| class="wikitable" | ||
|+Table 1. Therapeutic exercise terminology<ref name=":0" /> | |+Table 1. Therapeutic exercise terminology<ref name=":0" /><ref>Wikipedia. Strength training. Available from: https://en.wikipedia.org/wiki/Strength_training (accessed 14 March 2022).</ref> | ||
!Term | !Term | ||
!Definition | !Definition | ||
|- | |- | ||
|Exercise | |Exercise | ||
|Rotating joints in specific | |Rotating joints in specific ways to challenge muscles | ||
|- | |- | ||
|Form | |Form | ||
|A topography of movement to maximise safety and muscle strength | |A "topography of movement" or a specific manner of performing an exercise to maximise safety and ensure gains in muscle strength | ||
|- | |- | ||
|Repetition / rep | |Repetition / rep | ||
|A | |A cycle consisting of controlled lifting and lowering of a weight | ||
|- | |- | ||
|Set | |Set | ||
|Several repetitions | |Several repetitions performed in a row without a break | ||
|- | |- | ||
|1 repetition maximum / 1RM | |1 repetition maximum / 1RM | ||
|The maximum weight that | |The maximum weight that an individual can lift once | ||
|- | |- | ||
|Agonist | |Agonist | ||
| Line 50: | Line 47: | ||
|- | |- | ||
|Antagonist | |Antagonist | ||
|Opposite | |Opposite of an agonist, can control rapid movement eccentrically | ||
|- | |- | ||
|Synergist | |Synergist | ||
|Muscle(s) that stabilise(s) a joint around which movement | |Muscle(s) that stabilise(s) a joint around which movement occurs | ||
|- | |- | ||
|Tempo | |Tempo | ||
|The speed at which an exercise is | |The speed at which an exercise is completed; tempo affects both the amount of weight that can be moved and the muscle | ||
|} | |} | ||
== Tissue Damage, Pathogenesis, Pain and Performance == | == Tissue Damage, Pathogenesis, Pain and Performance == | ||
Injury and tissue damage | Injury and tissue damage cause a disruption in joint biomechanics:<ref name=":0" /> | ||
* Pain from an injury or surgery results in a cascade of changes that can cause disruptions to the joint and | * Pain from an injury or surgery results in a cascade of changes that can cause disruptions to the joint and, potentially, ongoing pain. This pain may last for years. This, in turn, can lead to degenerative changes such as facet arthritis, accelerated annular degeneration, and nerve root irritation. | ||
* Tissue damage occurs when excessive stress / strain is applied to a tissue (i.e. the force exceeds the strength of the tissue).<ref>Kalkhoven JT, Watsford ML, Impellizzeri FM. A conceptual model and detailed framework for stress-related, strain-related, and overuse athletic injury. Journal of Science and Medicine in Sport. 2020;23(8):726-34.</ref> Injury may occur after a single insult or from repeated loads.<ref name=":0" /> Tissue damage leads to motor control problems, | * Tissue damage occurs when excessive stress / strain is applied to a tissue (i.e. the force exceeds the strength of the tissue).<ref>Kalkhoven JT, Watsford ML, Impellizzeri FM. A conceptual model and detailed framework for stress-related, strain-related, and overuse athletic injury. Journal of Science and Medicine in Sport. 2020;23(8):726-34.</ref> Injury may occur after a single insult or from repeated loads.<ref name=":0" /> Tissue damage leads to motor control problems and, subsequently, long-term pain and degenerative changes. | ||
Injuries can also cause motor changes.<ref name=":0" /> Research has shown that individuals who report significant low back pain experience changes in their motor control systems.<ref>Van Dieën JH, Reeves NP, Kawchuk G, van Dillen LR, Hodges PW. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7393576/ Motor control changes in low back pain: divergence in presentations and mechanisms]. J Orthop Sports Phys Ther. 2019;49(6):370-379. </ref><ref>Meier ML, Vrana A, Schweinhardt P. [https://journals.sagepub.com/doi/full/10.1177/1073858418809074 Low back pain: the potential contribution of supraspinal motor control and proprioception]. Neuroscientist. 2019;25(6):583-96. </ref> | |||
Therefore, the challenge is to train the stabilising system during steady-state activities and during rapid voluntary motions, so that the body can withstand sudden, surprise loads.<ref name=":0" /> However, the presence of pain prevents the re-establishment of “healthy” motor patterns. And just as motor patterns are affected by injury, inappropriate motor patterns can also cause injury. Therefore, perturbed motor control systems are both a cause and a consequence of injury.<ref name=":0" /> | |||
However, as discussed above, there is considerable evidence to support the use of therapeutic exercise as an intervention for musculoskeletal injury or pain.<ref>Bailey DL, Holden MA, Foster NE, Quicke JG, Haywood KL, Bishop A. Defining adherence to therapeutic exercise for musculoskeletal pain: a systematic review. Br J Sports Med. 2020;54(6):326-31.</ref><ref>Babatunde OO, Jordan JL, Van der Windt DA, Hill JC, Foster NE, Protheroe J. [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0178621 Effective treatment options for musculoskeletal pain in primary care: A systematic overview of current evidence]. PLoS One. 2017;12(6):e0178621. </ref> It can improve:<ref name=":0" /> | |||
* Range of motion, flexibility | * Range of motion, flexibility and mobility | ||
* Muscle activation | * Muscle activation | ||
* Neuromuscular coordination | * Neuromuscular coordination | ||
| Line 79: | Line 76: | ||
== Progression and Regression Design Principles == | == Progression and Regression Design Principles == | ||
When prescribing exercises, it is important to understand how to progress and regress exercises. If patients are improving, exercises can be progressed. However, if they experience an increase in pain/symptoms, it may be necessary to | When prescribing exercises, it is important to understand how to progress and regress exercises. If patients are improving, exercises can be progressed. However, if they experience an increase in pain / symptoms, it may be necessary to alter certain parameters, including:<ref name=":0" /> | ||
* Sets | * Sets | ||
| Line 89: | Line 86: | ||
* Activation | * Activation | ||
** | ** Firstly, it is necessary to determine if the patient can activate the affected muscle - i.e. is there a connection between muscle and brain? | ||
* Tissue healing | * Tissue healing | ||
** The phase of healing will have a significant impact on which exercises are given | ** The [[Injury and Healing Within Sports Physiotherapy|phase of healing]] will have a significant impact on which exercises are given | ||
* Stabilisation | * Stabilisation | ||
** Joints are stabilised | ** Joints are stabilised by the muscles | ||
* Mobility | * Mobility | ||
** As stability increases, range can be added | ** As stability increases, range can be added | ||
| Line 107: | Line 104: | ||
* Manual cues<ref name=":0" /> | * Manual cues<ref name=":0" /> | ||
Various cues used to assist motor learning are discussed in more detail [[Motor Learning - Back to the Basics#Augmented Feedback|here]]. | |||
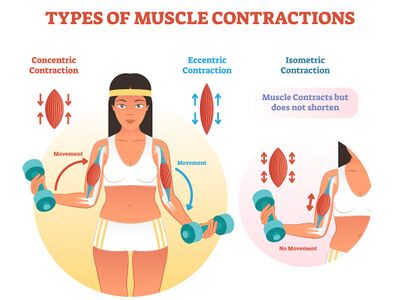
== Types of Muscle Contraction == | == Types of Muscle Contraction == | ||
Types of muscle contraction are:<ref name=":0" /><ref name=":1" /><ref>Padulo J, Laffaye G, Chamari K, Concu A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3899915/ Concentric and eccentric: muscle contraction or exercise?] ''Sports Health''. 2013;5(4):306.</ref> | [[File:Types of muscle contractions - shutterstock 1067519069.jpeg|thumb|400x400px|Figure 1. Types of muscle contractions.]] | ||
The types of muscle contraction are:<ref name=":0" /><ref name=":1" /><ref>Padulo J, Laffaye G, Chamari K, Concu A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3899915/ Concentric and eccentric: muscle contraction or exercise?] ''Sports Health''. 2013;5(4):306.</ref> | |||
* Isotonic | * Isotonic | ||
| Line 121: | Line 119: | ||
'''Eccentric exercise''':<ref name=":0" /><ref name=":2">Hody S, Croisier JL, Bury T, Rogister B, Leprince P. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6510035/ Eccentric muscle contractions: risks and benefits]. ''Front Physiol''. 2019;10:536. </ref> | '''Eccentric exercise''':<ref name=":0" /><ref name=":2">Hody S, Croisier JL, Bury T, Rogister B, Leprince P. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6510035/ Eccentric muscle contractions: risks and benefits]. ''Front Physiol''. 2019;10:536. </ref> | ||
* Negative force of a muscle contraction | * Negative force of a muscle contraction (i.e. negative work) | ||
* Leads to muscle hypertrophy | * Leads to muscle hypertrophy | ||
* Beneficial for tendons | * Beneficial for tendons | ||
| Line 129: | Line 127: | ||
'''Isometric exercise''':<ref name=":1" /> | '''Isometric exercise''':<ref name=":1" /> | ||
* Muscle contraction without any | * Muscle contraction without any movement / change in muscle length | ||
'''Concentric exercise''':<ref name=":0" /><ref name=":2" /> | '''Concentric exercise''':<ref name=":0" /><ref name=":2" /> | ||
* Positive force of a muscle contraction | * Positive force of a muscle contraction (i.e. positive work) | ||
* Used to build endurance and increase tolerance to exercise | * Used to build endurance and increase tolerance to exercise | ||
* Should take no | * Should take no longer than 3 seconds | ||
'''Concentric | '''Concentric versus eccentric''':<ref name=":0" /> | ||
* Eccentric strength must be greater than concentric strength<ref>Hollander DB, Kraemer RR, Kilpatrick MW, Ramadan ZG, Reeves GV, Francois M et al. Maximal eccentric and concentric strength discrepancies between young men and women for dynamic resistance exercise. J Strength Cond Res. 2007;21(1):34-40. </ref> | * Eccentric strength must be greater than concentric strength<ref>Hollander DB, Kraemer RR, Kilpatrick MW, Ramadan ZG, Reeves GV, Francois M et al. Maximal eccentric and concentric strength discrepancies between young men and women for dynamic resistance exercise. J Strength Cond Res. 2007;21(1):34-40. </ref> | ||
* The eccentric load must be greater than what an individual can lift concentrically | * The eccentric load must be greater than what an individual can lift concentrically | ||
The following video provides a detailed discussion of concentric, eccentric and isometric muscle contractions.{{#ev:youtube|gCyNj-Upbe4}}<ref>Corporis. Easiest Way to Remember Contraction Types: Concentric vs Eccentric vs Isometric | Corporis. Available from: https://www.youtube.com/watch?v=gCyNj-Upbe4 [last accessed 14/03/2022]</ref> | |||
== Overload Principle == | == Overload Principle == | ||
In order to improve strength, increased load must be applied to a muscle. This will increase the muscle's capability | In order to improve strength, increased load must be applied to a muscle. This will increase the muscle's capability. Progressively adding stress to the system means that it can adapt. It also prepares the body to do more in the future.<ref name=":0" /> | ||
The following video provides a brief discussion of the [https://www.physio-pedia.com/Physiology_In_Sport?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal#The_Basic_Principles_in_Exercise_Physiology overload principle]. | |||
{{#ev:youtube|TocsLwo7l9A}}<ref>National Council on Strength and Fitness. What is Overload, Progression & Specificity. Available from: https://www.youtube.com/watch?v=TocsLwo7l9A [last accessed 14/03/2022]</ref> | |||
Learn more about some of the basic principles (such as specificity, overload, reversibility and individuality) in exercise physiology [https://www.physio-pedia.com/Physiology_In_Sport?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal#The_Basic_Principles_in_Exercise_Physiology here]. | |||
=== Preparing the Patient === | === Preparing the Patient === | ||
| Line 153: | Line 155: | ||
* Educate for success: | * Educate for success: | ||
** Discuss how to progress | ** Discuss how to progress | ||
** Encourage | ** Encourage patients to keep going once they have finished therapy | ||
* Set expectations: | * Set expectations: | ||
** What is normal muscle soreness? | ** What is normal muscle soreness? | ||
*** 24-48 hours | *** 24-48 hours | ||
** How often should exercises be performed? | ** How often should exercises be performed? | ||
** How long will it take to make changes? | ** How long will it take to make changes? It is important to note that:<ref name=":0" /> | ||
*** It takes 4-6 weeks to achieve physiological changes in | *** It takes 4-6 weeks to achieve physiological changes in a muscle | ||
*** | *** Early increases in force production are associated with neural adaptations<ref>Škarabot J, Brownstein CG, Casolo A, Del Vecchio A, Ansdell P. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7892509/ The knowns and unknowns of neural adaptations to resistance training]. ''Eur J Appl Physiol''. 2021;121(3):675-85. </ref> | ||
*** A patient may ‘feel’ stronger | *** A patient may ‘feel’ stronger before 4-6 weeks have passed | ||
== Programme Design == | == Programme Design == | ||
Table 2 provides a summary of the traffic light system | Table 2 provides a summary of the traffic light system. This system can be used to determine at what level an individual should exercise. | ||
{| class="wikitable" | {| class="wikitable" | ||
|+ | |+ | ||
Table 2. Traffic light system | Table 2. Traffic light system for therapeutic exercise<ref name=":0" /> | ||
|- | |- | ||
|Red light | |Red light | ||
| Line 175: | Line 175: | ||
* Movement hurts and may cause further injury | * Movement hurts and may cause further injury | ||
* Pain before resistance | * Pain before resistance | ||
* “Hands-off” approach or | * “Hands-off” approach or isometric exercises | ||
|- | |- | ||
| | |Yellow light | ||
| | | | ||
* Movement does not hurt unless | * Movement does not hurt unless overpressure is applied | ||
* Pain at resistance | * Pain at resistance | ||
* Treat with | * Treat with minimum to moderate manual techniques, exercise before pain | ||
|- | |- | ||
|Green light | |Green light | ||
| Line 187: | Line 187: | ||
* Pain after resistance | * Pain after resistance | ||
* Decreased chance to cause further injury | * Decreased chance to cause further injury | ||
* | * Treat directly | ||
|} | |} | ||
=== General Principles === | === General Principles === | ||
It is essential to target an exercise intervention and focus on the impairment (i.e. weakness versus | It is essential to target an exercise intervention and focus on the impairment (i.e. weakness versus sensorimotor or neuromotor deficit). Consider:<ref name=":0" /> | ||
* Irritability and current level of function | * Irritability and current level of function | ||
| Line 198: | Line 198: | ||
* Progressions (necessary to see changes) | * Progressions (necessary to see changes) | ||
== Neuromuscular Education == | |||
Sensorimotor control is defined as "afferent and efferent information streams, as well as the central processing of these two, contributing to joint stability."<ref name=":3">De Zoete RMJ, Osmotherly PG, Rivett DA, Snodgrass SJ. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6994390/ Seven cervical sensorimotor control tests measure different skills in individuals with chronic idiopathic neck pain]. ''Braz J Phys Ther''. 2020;24(1):69-78.</ref> | Sensorimotor control is defined as "afferent and efferent information streams, as well as the central processing of these two, contributing to joint stability."<ref name=":3">De Zoete RMJ, Osmotherly PG, Rivett DA, Snodgrass SJ. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6994390/ Seven cervical sensorimotor control tests measure different skills in individuals with chronic idiopathic neck pain]. ''Braz J Phys Ther''. 2020;24(1):69-78.</ref> | ||
Sensorimotor impairment is associated with various musculoskeletal conditions, including neck pain,<ref name=":3" /> hand disorders,<ref>Röijezon U, Faleij R, Karvelis P, Georgoulas G, Nikolakopoulos G. [https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-017-1764-1 A new clinical test for sensorimotor function of the hand – development and preliminary validation]. ''BMC Musculoskelet Disord.'' 2017;18:407.</ref> back pain,<ref>Goossens N, Rummens S, Janssens L, Caeyenberghs K, Brumagne S. Association between sensorimotor impairments and functional brain changes in patients with low back pain: a critical review. Am J Phys Med Rehabil. 2018;97(3):200-11.</ref> etc. | Sensorimotor impairment is associated with various musculoskeletal conditions, including neck pain,<ref name=":3" /> hand disorders,<ref>Röijezon U, Faleij R, Karvelis P, Georgoulas G, Nikolakopoulos G. [https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-017-1764-1 A new clinical test for sensorimotor function of the hand – development and preliminary validation]. ''BMC Musculoskelet Disord.'' 2017;18:407.</ref> back pain,<ref>Goossens N, Rummens S, Janssens L, Caeyenberghs K, Brumagne S. Association between sensorimotor impairments and functional brain changes in patients with low back pain: a critical review. Am J Phys Med Rehabil. 2018;97(3):200-11.</ref> etc. Mechanisms for sensorimotor deficiency include:<ref name=":4">Ageberg E, Roos EM. Neuromuscular exercise as treatment of degenerative knee disease. Exerc Sport Sci Rev. 2015;43(1):14-22. </ref> | ||
* Impairments in the integration and processing of information in various parts of the sensorimotor system (e.g. sensory input, central nervous system, motor output) | |||
* Neural inhibition is associated with pain, swelling, inflammation, joint laxity, and damage to the afferents of joints<ref>Rice DA, McNair PJ. Quadriceps arthrogenic muscle inhibition: neural mechanisms and treatment perspectives. Semin Arthritis Rheum. 2010;40(3):250-66. </ref> | |||
* In knee pain, sensorimotor deficiencies have also been found in the non-injured leg:<ref name=":4" /> | |||
** This may be due to physical inactivity post-injury, reduced function, and impaired sensory feedback from the injured joint | |||
For a detailed discussion of the sensorimotor system, please see this article, and figure 1 in particular: [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC164311/ The sensorimotor system, part I: the physiologic basis of functional joint stability]<ref>Riemann BL, Lephart SM. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC164311/ The sensorimotor system, part I: the physiologic basis of functional joint stability]. ''J Athl Train''. 2002;37(1):71-9.</ref> | |||
The video below summarises the sensorimotor system. | |||
{{#ev:youtube|M0PEXquyhA4}}<ref>Professor Dave Explains. The Sensorimotor System and Human Reflexes. Available from: https://www.youtube.com/watch?v=M0PEXquyhA4 [last accessed 14/03/2022]</ref> | |||
=== Neuromuscular Training === | |||
Neuromuscular training programmes have been found to be effective in improving function and reducing symptoms for various injuries.<ref>Zech A, Hubscher M, Vogt L, Banzer W, Hansel F, Pfeifer K. [https://journals.lww.com/acsm-msse/Fulltext/2009/10000/Neuromuscular_Training_for_Rehabilitation_of.1.aspx Neuromuscular training for rehabilitation of sports injuries: a systematic review]. Med Sci Sports Exerc. 2009;41(10):1831-41.</ref><ref>Taulaniemi A, Kankaanpää M, Tokola K, Parkkari J, Suni JH. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6626624/ Neuromuscular exercise reduces low back pain intensity and improves physical functioning in nursing duties among female healthcare workers; secondary analysis of a randomised controlled trial]. ''BMC Musculoskelet Disord''. 2019;20(1):328.</ref> To improve sensorimotor control, [[Closed Chain Exercise|closed kinetic chain exercises]] are often performed in a range of positions.<ref name=":4" /> | |||
Please note that closed kinetic chain exercises are exercises or movements where the distal body segment is fixed to a stationary object.<ref>Physiopedia. [[Closed Chain Exercise|Closed chain exercise]].</ref> Open kinetic chain exercises are when the distal body segment (e.g. foot) is free / not fixed to an object.<ref>Physiopedia. [[Open Chain Exercise|Open chain exercise]].</ref> | |||
Progress function through motor learning principles:<ref name=":0" /> | |||
* Consider the [[Motor Learning - Back to the Basics#Practice Schedules|type of practice]] (components, variety) | |||
* Closed to [[Open Chain Exercise|open kinetic chain]]; simple to complex | |||
Progress function through movement:<ref name=":0" /> | |||
* Frequency, intensity, duration (time) | |||
* Endurance | |||
* Single- to multi-joint; closed to open | |||
The following video provides a basic summary of the FITT principles (i.e. frequency, intensity, time, type).{{#ev:youtube|Qss0afEmQiY}}<ref>PE Buddy. Learn the FITT Training Principles! Available from: https://www.youtube.com/watch?v=Qss0afEmQiY [last accessed 18/03/2022]</ref> | |||
The process is as follows:<ref name=":0" /> | |||
* Activation | |||
* Re-education | |||
* Motor learning | |||
* Functional movement training | |||
Remember that:<ref name=":0" /> | |||
* The core musculature is key to the movement of the extremities | |||
** The extremities are tied to the spine | |||
** The spine must be stable | |||
== Strength and Conditioning == | |||
'''Strength''' is defined as the amount of force that a specific muscle or muscle group can generate.<ref name=":0" /> | |||
'''Conditioning''' (endurance) is defined as the ability to “perform repetitive muscular contraction against some resistance for an extended period”.<ref>Prentice WE. Regaining muscular strength, endurance, and power [Internet]. Musculoskeletal Key. 2021 [cited 13 March 2022]. Available from: https://musculoskeletalkey.com/regaining-muscular-strength-endurance-and-power/</ref><blockquote>"Strength does not equal stability".<ref name=":0" /></blockquote>Strength and endurance training have many benefits:<ref name=":0" /> | |||
* Increased tissue vascularisation | |||
* Increased structural integrity of connective tissue | |||
* Improved lean muscle mass | |||
* Increased metabolic rate | |||
* Decreased body fat | |||
'''Tolerance:'''<ref name=":0" /> | |||
* Every individual has a tolerance for work | |||
* Tissues are damaged if their load tolerance is exceeded | |||
* Tolerance is lower in tissues that are already weakened by injury | |||
* Understanding each individual’s tolerance will assist in choosing the appropriate dosage / load for each stage of training | |||
'''Capacity''':<ref name=":0" /> | |||
* Every individual has a capacity for work | |||
* Capacity is defined as “the sum total of all activities over a period of time”<ref name=":0" /> (i.e. the maximum physical exertion that an individual can sustain<ref>Goldstein RE. Exercise Capacity. In: Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition. Boston: Butterworths; 1990. Chapter 8. Available from: https://www.ncbi.nlm.nih.gov/books/NBK404/</ref>) | |||
* People use up a portion of their daily capacity with every task they perform, including warm-up activities, poor posture (sitting or standing) | |||
* Ideal training occurs when capacity and tolerance are increased together | |||
Read more on: [[Neuromuscular Adaptations to Exercise]] | |||
=== Principles of Conditioning === | |||
* Warm up / cool down | |||
* Motivation | |||
* Overload (see below) | |||
* Consistency | |||
* Progression | |||
* Intensity | |||
* Specificity | |||
* Individuality | |||
* Minimise stress<ref name=":0" /> | |||
=== SAID Principle === | |||
The Specific Adaptation to Imposed Demands (SAID) principle is a framework on which strength and conditioning programmes can be designed.<ref>Johnson AM, Sandage MJ. [https://www.sciencedirect.com/science/article/pii/S0892199721002186 Exercise science and the vocalist]. J Voice. 2021;35(4):668-77. </ref> | |||
* All training is specific to a particular task | |||
* Specific skills or training may not be easily generalised or transferred to distinct activities<ref name=":0" /> | |||
The following video includes a discussion of the SAID principle and other principles of exercise training.{{#ev:youtube|X-zQ5hKB_G8}}<ref>Dr. Jacob Goodin. Scientific Training Principles for Strength & Conditioning. Available from: https://www.youtube.com/watch?v=X-zQ5hKB_G8 [last accessed 14/03/2022]</ref> | |||
=== Principles of Progression === | |||
'''Progressive overload''':<ref name=":0" /> | |||
* Increase or decrease difficulty with: | |||
** Reps | |||
** Sets | |||
** Speed | |||
** Complexity of exercise | |||
** Balance | |||
** Closed versus open chain | |||
*** Best results come from including both open and closed chain exercises | |||
*** Open to closed, closed to functional | |||
Exercises can also be progressed by challenging the '''balance system''':<ref name=":0" /> | |||
* Unstable surfaces | |||
* Head-turning | |||
* Eyes closed | |||
* Visual distraction | |||
More information on balance training is available [[Balance Training|here]]. | |||
== Additional Resource == | |||
{{#ev:youtube|wMbp1ZVUNKc }}<ref>The Principles of Exercise Therapy (PET). Lecture 4 - The Principles of Exercise Therapy. Available from: https://www.youtube.com/watch?v=wMbp1ZVUNKc [last accessed 18/03/2022]</ref> | |||
== References == | == References == | ||
[[Category: | [[Category:Plus Content]] | ||
[[Category:Course Pages]] | [[Category:Course Pages]] | ||
[[Category:Exercise Therapy]] | [[Category:Exercise Therapy]] | ||
Latest revision as of 11:48, 18 August 2022
Top Contributors - Jess Bell, Wanda van Niekerk and Kim Jackson
Introduction[edit | edit source]
When considering exercise prescription in physiotherapy practice, it is important to understand the difference between therapeutic exercise and general exercise. General exercise is essentially a “work out”. It is exercise for wellness, overall health, appearance, fun, leisure etc.[1]
Therapeutic exercise is specifically for individuals who have a physical problem / impairment, which is often painful.[1]
“Therapeutic exercise is distinguishable from other forms of recreation because it is a purposeful, body-building activity, often prescribed by experts [...], drawing on their knowledge of bodily function to engage in a powerful form of anatomo-politics”.[2]
Rehabilitation professionals must be able to assess, analyse, and determine the cause of a client’s pain or impairment. Exercises are then prescribed in order to address deficits in:[1]
- Mobility / flexibility
- Strength and power
- Neuromuscular control
- Muscular endurance
Why Include Therapeutic Exercise in a Treatment Plan?[edit | edit source]
Exercise interventions are beneficial as they enable individuals to self-manage their symptoms.[1] Moreover, there is a large body of research to support its use in clinical practice.[3][4] [5]
- Research supports the use of exercise interventions for long-term changes when compared to manual therapy alone
- A systematic review by Lin et al.[6] appraised 44 clinical practice guidelines for musculoskeletal pain conditions. They found that exercise was recommended in all guidelines. However, when manual therapy is utilised, it should be used alongside other interventions (i.e. exercise, psychological therapy, information / education, activity advice).[6]
- Exercise is supported over other therapeutic interventions[1]
Terminology[edit | edit source]
Table 1 provides a list of terms that are often used when discussing therapeutic exercise.
| Term | Definition |
|---|---|
| Exercise | Rotating joints in specific ways to challenge muscles |
| Form | A "topography of movement" or a specific manner of performing an exercise to maximise safety and ensure gains in muscle strength |
| Repetition / rep | A cycle consisting of controlled lifting and lowering of a weight |
| Set | Several repetitions performed in a row without a break |
| 1 repetition maximum / 1RM | The maximum weight that an individual can lift once |
| Agonist | Prime mover |
| Antagonist | Opposite of an agonist, can control rapid movement eccentrically |
| Synergist | Muscle(s) that stabilise(s) a joint around which movement occurs |
| Tempo | The speed at which an exercise is completed; tempo affects both the amount of weight that can be moved and the muscle |
Tissue Damage, Pathogenesis, Pain and Performance[edit | edit source]
Injury and tissue damage cause a disruption in joint biomechanics:[1]
- Pain from an injury or surgery results in a cascade of changes that can cause disruptions to the joint and, potentially, ongoing pain. This pain may last for years. This, in turn, can lead to degenerative changes such as facet arthritis, accelerated annular degeneration, and nerve root irritation.
- Tissue damage occurs when excessive stress / strain is applied to a tissue (i.e. the force exceeds the strength of the tissue).[8] Injury may occur after a single insult or from repeated loads.[1] Tissue damage leads to motor control problems and, subsequently, long-term pain and degenerative changes.
Injuries can also cause motor changes.[1] Research has shown that individuals who report significant low back pain experience changes in their motor control systems.[9][10]
Therefore, the challenge is to train the stabilising system during steady-state activities and during rapid voluntary motions, so that the body can withstand sudden, surprise loads.[1] However, the presence of pain prevents the re-establishment of “healthy” motor patterns. And just as motor patterns are affected by injury, inappropriate motor patterns can also cause injury. Therefore, perturbed motor control systems are both a cause and a consequence of injury.[1]
However, as discussed above, there is considerable evidence to support the use of therapeutic exercise as an intervention for musculoskeletal injury or pain.[11][12] It can improve:[1]
- Range of motion, flexibility and mobility
- Muscle activation
- Neuromuscular coordination
- Joint stability
- Strength and power
- Muscle endurance
Progression and Regression Design Principles[edit | edit source]
When prescribing exercises, it is important to understand how to progress and regress exercises. If patients are improving, exercises can be progressed. However, if they experience an increase in pain / symptoms, it may be necessary to alter certain parameters, including:[1]
- Sets
- Repetitions
- Speed
- Resistance
Phases of Exercise[edit | edit source]
- Activation
- Firstly, it is necessary to determine if the patient can activate the affected muscle - i.e. is there a connection between muscle and brain?
- Tissue healing
- The phase of healing will have a significant impact on which exercises are given
- Stabilisation
- Joints are stabilised by the muscles
- Mobility
- As stability increases, range can be added
- Muscle performance improvement
- Advanced coordination and skill
- Progressively add difficulty in movement patterns to restore normal functional abilities[1]
Teaching Methods for Exercise[edit | edit source]
- Verbal cues
- Mental imagery
- Visual feedback
- Manual cues[1]
Various cues used to assist motor learning are discussed in more detail here.
Types of Muscle Contraction[edit | edit source]
The types of muscle contraction are:[1][5][13]
- Isotonic
- Concentric (shortening)
- Eccentric (lengthening)
- Isometric
- Static / holding
- Isokinetic
- Negative force of a muscle contraction (i.e. negative work)
- Leads to muscle hypertrophy
- Beneficial for tendons
- Causes delayed onset muscle soreness
- Should take no less than 4 seconds
Isometric exercise:[5]
- Muscle contraction without any movement / change in muscle length
- Positive force of a muscle contraction (i.e. positive work)
- Used to build endurance and increase tolerance to exercise
- Should take no longer than 3 seconds
Concentric versus eccentric:[1]
- Eccentric strength must be greater than concentric strength[15]
- The eccentric load must be greater than what an individual can lift concentrically
The following video provides a detailed discussion of concentric, eccentric and isometric muscle contractions.
Overload Principle[edit | edit source]
In order to improve strength, increased load must be applied to a muscle. This will increase the muscle's capability. Progressively adding stress to the system means that it can adapt. It also prepares the body to do more in the future.[1]
The following video provides a brief discussion of the overload principle.
Learn more about some of the basic principles (such as specificity, overload, reversibility and individuality) in exercise physiology here.
Preparing the Patient[edit | edit source]
In order to prepare the patient for therapeutic exercise, please consider the following:[1]
- Educate for success:
- Discuss how to progress
- Encourage patients to keep going once they have finished therapy
- Set expectations:
- What is normal muscle soreness?
- 24-48 hours
- How often should exercises be performed?
- How long will it take to make changes? It is important to note that:[1]
- It takes 4-6 weeks to achieve physiological changes in a muscle
- Early increases in force production are associated with neural adaptations[18]
- A patient may ‘feel’ stronger before 4-6 weeks have passed
- What is normal muscle soreness?
Programme Design[edit | edit source]
Table 2 provides a summary of the traffic light system. This system can be used to determine at what level an individual should exercise.
| Red light |
|
| Yellow light |
|
| Green light |
|
General Principles[edit | edit source]
It is essential to target an exercise intervention and focus on the impairment (i.e. weakness versus sensorimotor or neuromotor deficit). Consider:[1]
- Irritability and current level of function
- Reps and sets scheme
- Targeted impairment category
- Progressions (necessary to see changes)
Neuromuscular Education[edit | edit source]
Sensorimotor control is defined as "afferent and efferent information streams, as well as the central processing of these two, contributing to joint stability."[19]
Sensorimotor impairment is associated with various musculoskeletal conditions, including neck pain,[19] hand disorders,[20] back pain,[21] etc. Mechanisms for sensorimotor deficiency include:[22]
- Impairments in the integration and processing of information in various parts of the sensorimotor system (e.g. sensory input, central nervous system, motor output)
- Neural inhibition is associated with pain, swelling, inflammation, joint laxity, and damage to the afferents of joints[23]
- In knee pain, sensorimotor deficiencies have also been found in the non-injured leg:[22]
- This may be due to physical inactivity post-injury, reduced function, and impaired sensory feedback from the injured joint
For a detailed discussion of the sensorimotor system, please see this article, and figure 1 in particular: The sensorimotor system, part I: the physiologic basis of functional joint stability[24]
The video below summarises the sensorimotor system.
Neuromuscular Training[edit | edit source]
Neuromuscular training programmes have been found to be effective in improving function and reducing symptoms for various injuries.[26][27] To improve sensorimotor control, closed kinetic chain exercises are often performed in a range of positions.[22]
Please note that closed kinetic chain exercises are exercises or movements where the distal body segment is fixed to a stationary object.[28] Open kinetic chain exercises are when the distal body segment (e.g. foot) is free / not fixed to an object.[29]
Progress function through motor learning principles:[1]
- Consider the type of practice (components, variety)
- Closed to open kinetic chain; simple to complex
Progress function through movement:[1]
- Frequency, intensity, duration (time)
- Endurance
- Single- to multi-joint; closed to open
The following video provides a basic summary of the FITT principles (i.e. frequency, intensity, time, type).
The process is as follows:[1]
- Activation
- Re-education
- Motor learning
- Functional movement training
Remember that:[1]
- The core musculature is key to the movement of the extremities
- The extremities are tied to the spine
- The spine must be stable
Strength and Conditioning[edit | edit source]
Strength is defined as the amount of force that a specific muscle or muscle group can generate.[1]
Conditioning (endurance) is defined as the ability to “perform repetitive muscular contraction against some resistance for an extended period”.[31]
"Strength does not equal stability".[1]
Strength and endurance training have many benefits:[1]
- Increased tissue vascularisation
- Increased structural integrity of connective tissue
- Improved lean muscle mass
- Increased metabolic rate
- Decreased body fat
Tolerance:[1]
- Every individual has a tolerance for work
- Tissues are damaged if their load tolerance is exceeded
- Tolerance is lower in tissues that are already weakened by injury
- Understanding each individual’s tolerance will assist in choosing the appropriate dosage / load for each stage of training
Capacity:[1]
- Every individual has a capacity for work
- Capacity is defined as “the sum total of all activities over a period of time”[1] (i.e. the maximum physical exertion that an individual can sustain[32])
- People use up a portion of their daily capacity with every task they perform, including warm-up activities, poor posture (sitting or standing)
- Ideal training occurs when capacity and tolerance are increased together
Read more on: Neuromuscular Adaptations to Exercise
Principles of Conditioning[edit | edit source]
- Warm up / cool down
- Motivation
- Overload (see below)
- Consistency
- Progression
- Intensity
- Specificity
- Individuality
- Minimise stress[1]
SAID Principle[edit | edit source]
The Specific Adaptation to Imposed Demands (SAID) principle is a framework on which strength and conditioning programmes can be designed.[33]
- All training is specific to a particular task
- Specific skills or training may not be easily generalised or transferred to distinct activities[1]
The following video includes a discussion of the SAID principle and other principles of exercise training.
Principles of Progression[edit | edit source]
Progressive overload:[1]
- Increase or decrease difficulty with:
- Reps
- Sets
- Speed
- Complexity of exercise
- Balance
- Closed versus open chain
- Best results come from including both open and closed chain exercises
- Open to closed, closed to functional
Exercises can also be progressed by challenging the balance system:[1]
- Unstable surfaces
- Head-turning
- Eyes closed
- Visual distraction
More information on balance training is available here.
Additional Resource[edit | edit source]
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 1.22 1.23 1.24 1.25 1.26 1.27 1.28 1.29 1.30 1.31 1.32 1.33 1.34 1.35 1.36 1.37 Jackson R. Therapeutic Exercise Course. Plus. 2022.
- ↑ Nicholls D, Jachyra P, Gibson BE, Fusco C, Setchell J. Keep fit: marginal ideas in contemporary therapeutic exercise. Qualitative Research in Sport, Exercise and Health. 2018;10(4):400-11.
- ↑ Maestroni L, Read P, Bishop C, Papadopoulos K, Suchomel TJ, Comfort P et al. The benefits of strength training on musculoskeletal system health: practical applications for interdisciplinary care. Sports Med. 2020;50(8):1431-50.
- ↑ Prall J, Ross M. The management of work-related musculoskeletal injuries in an occupational health setting: the role of the physical therapist. J Exerc Rehabil. 2019;15(2):193-9.
- ↑ 5.0 5.1 5.2 Bielecki JE, Tadi P. Therapeutic Exercise. [Updated 2021 Sep 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK555914/
- ↑ 6.0 6.1 Lin I, Wiles L, Waller R, Goucke R, Nagree Y, Gibberd M et al. What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: systematic review. Br J Sports Med. 2020;54(2):79-86.
- ↑ Wikipedia. Strength training. Available from: https://en.wikipedia.org/wiki/Strength_training (accessed 14 March 2022).
- ↑ Kalkhoven JT, Watsford ML, Impellizzeri FM. A conceptual model and detailed framework for stress-related, strain-related, and overuse athletic injury. Journal of Science and Medicine in Sport. 2020;23(8):726-34.
- ↑ Van Dieën JH, Reeves NP, Kawchuk G, van Dillen LR, Hodges PW. Motor control changes in low back pain: divergence in presentations and mechanisms. J Orthop Sports Phys Ther. 2019;49(6):370-379.
- ↑ Meier ML, Vrana A, Schweinhardt P. Low back pain: the potential contribution of supraspinal motor control and proprioception. Neuroscientist. 2019;25(6):583-96.
- ↑ Bailey DL, Holden MA, Foster NE, Quicke JG, Haywood KL, Bishop A. Defining adherence to therapeutic exercise for musculoskeletal pain: a systematic review. Br J Sports Med. 2020;54(6):326-31.
- ↑ Babatunde OO, Jordan JL, Van der Windt DA, Hill JC, Foster NE, Protheroe J. Effective treatment options for musculoskeletal pain in primary care: A systematic overview of current evidence. PLoS One. 2017;12(6):e0178621.
- ↑ Padulo J, Laffaye G, Chamari K, Concu A. Concentric and eccentric: muscle contraction or exercise? Sports Health. 2013;5(4):306.
- ↑ 14.0 14.1 Hody S, Croisier JL, Bury T, Rogister B, Leprince P. Eccentric muscle contractions: risks and benefits. Front Physiol. 2019;10:536.
- ↑ Hollander DB, Kraemer RR, Kilpatrick MW, Ramadan ZG, Reeves GV, Francois M et al. Maximal eccentric and concentric strength discrepancies between young men and women for dynamic resistance exercise. J Strength Cond Res. 2007;21(1):34-40.
- ↑ Corporis. Easiest Way to Remember Contraction Types: Concentric vs Eccentric vs Isometric | Corporis. Available from: https://www.youtube.com/watch?v=gCyNj-Upbe4 [last accessed 14/03/2022]
- ↑ National Council on Strength and Fitness. What is Overload, Progression & Specificity. Available from: https://www.youtube.com/watch?v=TocsLwo7l9A [last accessed 14/03/2022]
- ↑ Škarabot J, Brownstein CG, Casolo A, Del Vecchio A, Ansdell P. The knowns and unknowns of neural adaptations to resistance training. Eur J Appl Physiol. 2021;121(3):675-85.
- ↑ 19.0 19.1 De Zoete RMJ, Osmotherly PG, Rivett DA, Snodgrass SJ. Seven cervical sensorimotor control tests measure different skills in individuals with chronic idiopathic neck pain. Braz J Phys Ther. 2020;24(1):69-78.
- ↑ Röijezon U, Faleij R, Karvelis P, Georgoulas G, Nikolakopoulos G. A new clinical test for sensorimotor function of the hand – development and preliminary validation. BMC Musculoskelet Disord. 2017;18:407.
- ↑ Goossens N, Rummens S, Janssens L, Caeyenberghs K, Brumagne S. Association between sensorimotor impairments and functional brain changes in patients with low back pain: a critical review. Am J Phys Med Rehabil. 2018;97(3):200-11.
- ↑ 22.0 22.1 22.2 Ageberg E, Roos EM. Neuromuscular exercise as treatment of degenerative knee disease. Exerc Sport Sci Rev. 2015;43(1):14-22.
- ↑ Rice DA, McNair PJ. Quadriceps arthrogenic muscle inhibition: neural mechanisms and treatment perspectives. Semin Arthritis Rheum. 2010;40(3):250-66.
- ↑ Riemann BL, Lephart SM. The sensorimotor system, part I: the physiologic basis of functional joint stability. J Athl Train. 2002;37(1):71-9.
- ↑ Professor Dave Explains. The Sensorimotor System and Human Reflexes. Available from: https://www.youtube.com/watch?v=M0PEXquyhA4 [last accessed 14/03/2022]
- ↑ Zech A, Hubscher M, Vogt L, Banzer W, Hansel F, Pfeifer K. Neuromuscular training for rehabilitation of sports injuries: a systematic review. Med Sci Sports Exerc. 2009;41(10):1831-41.
- ↑ Taulaniemi A, Kankaanpää M, Tokola K, Parkkari J, Suni JH. Neuromuscular exercise reduces low back pain intensity and improves physical functioning in nursing duties among female healthcare workers; secondary analysis of a randomised controlled trial. BMC Musculoskelet Disord. 2019;20(1):328.
- ↑ Physiopedia. Closed chain exercise.
- ↑ Physiopedia. Open chain exercise.
- ↑ PE Buddy. Learn the FITT Training Principles! Available from: https://www.youtube.com/watch?v=Qss0afEmQiY [last accessed 18/03/2022]
- ↑ Prentice WE. Regaining muscular strength, endurance, and power [Internet]. Musculoskeletal Key. 2021 [cited 13 March 2022]. Available from: https://musculoskeletalkey.com/regaining-muscular-strength-endurance-and-power/
- ↑ Goldstein RE. Exercise Capacity. In: Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition. Boston: Butterworths; 1990. Chapter 8. Available from: https://www.ncbi.nlm.nih.gov/books/NBK404/
- ↑ Johnson AM, Sandage MJ. Exercise science and the vocalist. J Voice. 2021;35(4):668-77.
- ↑ Dr. Jacob Goodin. Scientific Training Principles for Strength & Conditioning. Available from: https://www.youtube.com/watch?v=X-zQ5hKB_G8 [last accessed 14/03/2022]
- ↑ The Principles of Exercise Therapy (PET). Lecture 4 - The Principles of Exercise Therapy. Available from: https://www.youtube.com/watch?v=wMbp1ZVUNKc [last accessed 18/03/2022]