Glioblastoma: Difference between revisions
No edit summary |
No edit summary |
||
| (One intermediate revision by the same user not shown) | |||
| Line 40: | Line 40: | ||
== Management == | == Management == | ||
[[Image:Surgery.jpg|frame|right|Surgical resection of GBM tumor]]Biopsy and tumor debulking with postoperative adjuvant radiotherapy and chemotherapy (temozolomide) are the most commonly carried out treatment. Newer therapies include antiangiogenesis (e.g. bevacizumab) and immunotherapy.<ref name=":0" /> | |||
< | |||
There are many experimental treatment techniques being developed in hopes to rid patients of GBM tumors. Some of these treatment options are not yet FDA approved. An example of an experimental treatment is: an MRI-guided laser interstitial thermal therapy system called [http://medgadget.com/archives/2008/04/autolitt_laser_interstitial_thermal_therapy_system.html AutoLITT]. | There are many experimental treatment techniques being developed in hopes to rid patients of GBM tumors. Some of these treatment options are not yet FDA approved. An example of an experimental treatment is: an MRI-guided laser interstitial thermal therapy system called [http://medgadget.com/archives/2008/04/autolitt_laser_interstitial_thermal_therapy_system.html AutoLITT]. | ||
Despite this, it carries a poor prognosis with a median survival of fewer than 2 years <ref name=":0" /> | |||
==Physical Therapy Management == | ==Physical Therapy Management == | ||
No universal restrictions on activity are necessary for patients with glioblastomas. The patient's activity depends on his or her overall neurologic status. The presence of seizures may prevent the patient from driving. In many circumstances, physical therapy and/or rehabilitation are extremely beneficial. Activity is encouraged to reduce the risk of deep venous thrombosis.<ref name="treatment" /> | No universal restrictions on activity are necessary for patients with glioblastomas. The patient's activity depends on his or her overall neurologic status. The presence of seizures may prevent the patient from driving. In many circumstances, physical therapy and/or rehabilitation are extremely beneficial. Activity is encouraged to reduce the risk of deep venous thrombosis.<ref name="treatment">Glioblastoma Multiforme Treatment & Management (medical care). Medscape. Available at http://emedicine.medscape.com/article/283252-treatment. Accessed April 3, 2011.</ref> | ||
A physical therapist may be consulted to assess functional status and provide treatment aimed at maximizing independence and functional capacity. Home or out-patient physical therapy may be recommended to continue to maximize functional mobility. If intensive physical therapy is required, patients may benefit from an inpatient stay at a rehabilitation hospital. Physical therapy evaluation includes identifying what areas may be limiting function: strength, balance, endurance, pain. The physical therapist may prescribe individualized exercises to address the above areas, and may recommend adaptive equipment.<ref name="brain">Glioblastoma multiforme and anaplastic gliomas: A patient guide. Massachusetts General Hospital (Brain Tumor Center). Available at http://brain.mgh.harvard.edu/patientguide.htm. Accessed March 31, 2011.</ref> | A physical therapist may be consulted to assess functional status and provide treatment aimed at maximizing independence and functional capacity. Home or out-patient physical therapy may be recommended to continue to maximize functional mobility. If intensive physical therapy is required, patients may benefit from an inpatient stay at a rehabilitation hospital. Physical therapy evaluation includes identifying what areas may be limiting function: strength, balance, endurance, pain. The physical therapist may prescribe individualized exercises to address the above areas, and may recommend adaptive equipment.<ref name="brain">Glioblastoma multiforme and anaplastic gliomas: A patient guide. Massachusetts General Hospital (Brain Tumor Center). Available at http://brain.mgh.harvard.edu/patientguide.htm. Accessed March 31, 2011.</ref> | ||
| Line 81: | Line 57: | ||
==Case Reports / Case Studies== | ==Case Reports / Case Studies== | ||
*Well-Circumscribed, Minimally Enhancing Glioblastoma Multiforme of the Trigone: A Case Report and Review of the Literature [view article in the [http://www.ajnr.org/cgi/content/full/26/6/1475 ''American Journal of Neuroradiology'']] | *Well-Circumscribed, Minimally Enhancing Glioblastoma Multiforme of the Trigone: A Case Report and Review of the Literature [view article in the [http://www.ajnr.org/cgi/content/full/26/6/1475 ''American Journal of Neuroradiology'']] | ||
*Case-Control Study of Use of NSAIDs and GBM [view case study in the ''[http://aje.oxfordjournals.org/content/159/12/1131.full American Journal of Epidemiology]''] | *Case-Control Study of Use of NSAIDs and GBM [view case study in the ''[http://aje.oxfordjournals.org/content/159/12/1131.full American Journal of Epidemiology]''] | ||
Latest revision as of 04:59, 11 May 2022
Original Editors - Simone Potts from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Simone Potts, Lucinda hampton, Admin, Kim Jackson, Elaine Lonnemann, 127.0.0.1, Wendy Walker and WikiSysop
Introduction[edit | edit source]
Glioblastomas (GBM) are the most common adult primary brain tumor and are aggressive, relatively resistant to therapy, and have a poor prognosis.
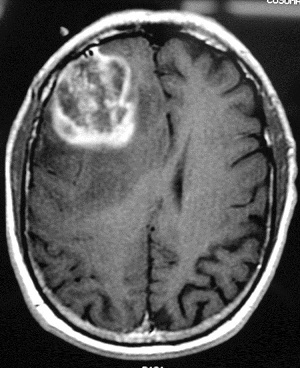
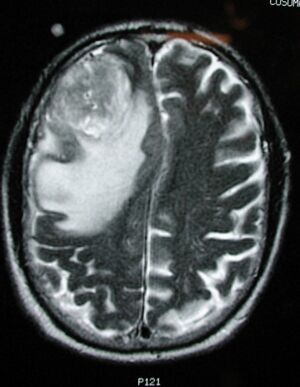
- They typically appear as heterogeneous masses centered in the white matter with irregular peripheral enhancement, central necrosis and are surrounded by vasogenic edema.
- Treatment primarily consists of surgery and concurrent radiotherapy and temozolomide.[1]
Etiology[edit | edit source]
Despite studies looking for genetic and environmental factors in glioblastoma multiforme, but no risk factor in most instances of GBM has been identified. Like many other cancers, GBM is sporadic, although a study showed a high prevalence (17%) of prior therapeutic irradiation among patients with GBM[2].
Although concerns have been raised regarding cell phone use as a potential risk factor for development of gliomas, study results have been inconsistent, and this possibility remains controversial. The largest studies have not supported cell phone use as a cancer risk factor. However, a recently released multinational report concluded that studies that are independent of the telecom industry show that cell phone use may pose a significant risk for brain tumors, and some European countries have taken steps to limit cell phone use by children[3].
Epidemiology[edit | edit source]
Glioblastomas usually occur after the age of 40 years (peak incidence between 65 and 75 years of age). There is a slight male preponderance with a 3:2 M:F ratio. Caucasians are affected more frequently than other ethnicities. Approximately 60% of the estimated 17,000 primary brain tumors diagnosed in the United States each year are gliomas. [3]
- The majority of glioblastomas are sporadic.
- Rarely found to be related to prior radiation exposure (radiation-induced GBM).
- They can also occur as part of rare inherited tumor syndromes eg neurofibromatosis type1 (NF1)
Characteristics / Clinical Presentation[edit | edit source]
Presentation is usually in one of the ways listed below:
- Focal neurological deficit
- Symptoms of increased intracranial pressure
- Seizures[1]
Diagnosis[edit | edit source]
Tests and procedures used to diagnose glioblastoma include:
- Neurological exam
- Imaging tests. MRI is often used to diagnose brain tumors, may be used along with specialized MRI imaging, eg functional MRI and magnetic resonance spectroscopy.
- Removing a sample of tissue for biopsy[4].
Management[edit | edit source]
Biopsy and tumor debulking with postoperative adjuvant radiotherapy and chemotherapy (temozolomide) are the most commonly carried out treatment. Newer therapies include antiangiogenesis (e.g. bevacizumab) and immunotherapy.[1]
There are many experimental treatment techniques being developed in hopes to rid patients of GBM tumors. Some of these treatment options are not yet FDA approved. An example of an experimental treatment is: an MRI-guided laser interstitial thermal therapy system called AutoLITT.
Despite this, it carries a poor prognosis with a median survival of fewer than 2 years [1]
Physical Therapy Management[edit | edit source]
No universal restrictions on activity are necessary for patients with glioblastomas. The patient's activity depends on his or her overall neurologic status. The presence of seizures may prevent the patient from driving. In many circumstances, physical therapy and/or rehabilitation are extremely beneficial. Activity is encouraged to reduce the risk of deep venous thrombosis.[5]
A physical therapist may be consulted to assess functional status and provide treatment aimed at maximizing independence and functional capacity. Home or out-patient physical therapy may be recommended to continue to maximize functional mobility. If intensive physical therapy is required, patients may benefit from an inpatient stay at a rehabilitation hospital. Physical therapy evaluation includes identifying what areas may be limiting function: strength, balance, endurance, pain. The physical therapist may prescribe individualized exercises to address the above areas, and may recommend adaptive equipment.[6]
Exercise is good for GBM patients as long as it is to the patient's tolerance. Functional strengthening and aerobic training should be progressed slowly. These patients will benefit greatly from low intensity exercise. Physical therapists should establish the patient's pulmonary function and fitness level (especially if the patient becomes deconditioned after surgery and/or diagnosis).
Patient and family education is crucial to the improvement of each case of GBM. Each patient needs to be made aware of the symptoms, progression and treatment of this cancer.
Case Reports / Case Studies[edit | edit source]
- Well-Circumscribed, Minimally Enhancing Glioblastoma Multiforme of the Trigone: A Case Report and Review of the Literature [view article in the American Journal of Neuroradiology]
- Case-Control Study of Use of NSAIDs and GBM [view case study in the American Journal of Epidemiology]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Radiopedia Glioblastoma Available: https://radiopaedia.org/articles/glioblastoma-idh-wildtype?lang=us(accessed 11.5.2022)
- ↑ Kanderi T, Gupta V. Glioblastoma multiforme. InStatPearls [Internet] 2021 Feb 6. StatPearls Publishing.Available:https://www.ncbi.nlm.nih.gov/books/NBK558954/ (accessed 11.5.2022)
- ↑ 3.0 3.1 Glioblastoma Multiforme (background). Medscape. Available at http://emedicine.medscape.com/article/283252-overview. Accessed March 29, 2011.
- ↑ Mayo clinic Glioma Available;https://www.mayoclinic.org/diseases-conditions/glioblastoma/cdc-20350148 (accessed 11.5.2022)
- ↑ Glioblastoma Multiforme Treatment & Management (medical care). Medscape. Available at http://emedicine.medscape.com/article/283252-treatment. Accessed April 3, 2011.
- ↑ Glioblastoma multiforme and anaplastic gliomas: A patient guide. Massachusetts General Hospital (Brain Tumor Center). Available at http://brain.mgh.harvard.edu/patientguide.htm. Accessed March 31, 2011.