Maternal Obstetric Palsy: Difference between revisions
Kim Jackson (talk | contribs) No edit summary |
Rosie Swift (talk | contribs) (Updated information with more current references and linked to other relevant articles on pysiopedia page - not finished yet!) |
||
| Line 4: | Line 4: | ||
<div class="editorbox"> '''Original Editor '''- [[User:User Name|Onigbinde Omotola Adam]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | <div class="editorbox"> '''Original Editor '''- [[User:User Name|Onigbinde Omotola Adam]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== Introduction == | == Introduction == | ||
Maternal obstetric palsy or obstetric maternal palsy or obstetric maternal lumbosacral plexopathy refers to an injury to the lumbosacral plexus whose signs and symptoms become evident during labor or after childbirth. | Maternal obstetric palsy or obstetric maternal palsy or obstetric maternal lumbosacral plexopathy refers to an injury to the lumbosacral plexus whose signs and symptoms become evident during labor or after childbirth. This differs to obstetric palsy (also called [[Erb's Palsy]]) which involves brachial plexus injury of the infant during delivery. | ||
== Epidemiology == | == Epidemiology == | ||
The population of women with maternal obstetrical palsy are relatively small, hence the absence of the condition in many textbooks<ref name=":0">2 | The population of women with maternal obstetrical palsy are relatively small, hence the absence of the condition in many textbooks<ref name=":0">2 | ||
</ref>. Feasby et al. reported | </ref>. Feasby et al. reported 2 cases in 1992<ref name=":0" />, Katirji et al. had 7 women reported in 2002<ref name=":1">4 | ||
</ref> | </ref>. | ||
== Risk factors<ref name=":0" /> == | == Risk factors<ref name=":0" /> == | ||
Macrosomia | * Short stature | ||
* Macrosomia | |||
Cephalopelvic disproportion | * Cephalopelvic disproportion | ||
* Delayed/Prolonged labor | |||
Delayed/Prolonged labor | * Static position of the lower extremities during a prolonged second stage of labour<ref>Boyce H and Plaat F. Post-natal neurological problems. Continuing Education on Anaesthesia Critical Care & Pain. 2013;13:2,63-66. Available from https://academic.oup.com/bjaed/article/13/2/63/283709 [Accessed 2 Dec 2021]</ref> | ||
* Mid forceps rotation | |||
Mid forceps rotation | * Fetal malpositioning | ||
Fetal malpositioning | |||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
| Line 30: | Line 27: | ||
== Mechanism of Injury / Pathological Process == | == Mechanism of Injury / Pathological Process == | ||
The position of the | The position of the lumbosacral plexus predisposes itself to compression during prolonged labour, especially in women who are of short stature with cephalopelvic disproportion. Any trauma, or compression or injury to the trunks of the lumbosacral plexus causes clinical signs and symptoms in the mother that may result during or after labour. | ||
The peroneal nerve is frequently affected and | Katirji et al. (2002) concluded that intrapartum foot drop occurs mostly in short women and is caused by lumbosacral trunk compression by the fetal head at the pelvic brim primary pathology being predominantly demyelination and recovery is complete in up to 5 months.<ref name=":1" /> | ||
The peroneal nerve is frequently affected and Hunerman (1892) attributed its frequency to its position in the lumbosacral plexus." | |||
== Types == | == Types == | ||
| Line 48: | Line 47: | ||
== Clinical Presentation == | == Clinical Presentation == | ||
For the upper palsy: | For the upper palsy: | ||
* pain | |||
* paraesthesia, sensory loss in the L‐5 dermatome | |||
* weakness of ankle dorsiflexion, eversion, and inversion causing [[foot drop]] | |||
For the lower palsy:<ref name=":2" /> | |||
Sexual dysfunction | * Perineal sensori-neuropathy | ||
* Urinary incontinence | |||
* Fecal incontinence | |||
* Sexual dysfunction | |||
== Diagnostic Procedures == | |||
A detailed subjective history should be taken from the patient. Intrapartum palsy would have been observed during parturition. | |||
Objective diagnostic procedures include the use of Electrodiagnostic devices vis a vis: EMG in determining the level of affectation. Compound Muscle Action Potential (CMAP), Sensory Nerve Action Potential (SNAP) are recorded to know the exact site of injury. | Objective diagnostic procedures include the use of Electrodiagnostic devices vis a vis: EMG in determining the level of affectation. Compound Muscle Action Potential (CMAP), Sensory Nerve Action Potential (SNAP) are recorded to know the exact site of injury. | ||
Revision as of 11:30, 2 December 2021
This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! (2/12/2021)
Introduction[edit | edit source]
Maternal obstetric palsy or obstetric maternal palsy or obstetric maternal lumbosacral plexopathy refers to an injury to the lumbosacral plexus whose signs and symptoms become evident during labor or after childbirth. This differs to obstetric palsy (also called Erb's Palsy) which involves brachial plexus injury of the infant during delivery.
Epidemiology[edit | edit source]
The population of women with maternal obstetrical palsy are relatively small, hence the absence of the condition in many textbooks[1]. Feasby et al. reported 2 cases in 1992[1], Katirji et al. had 7 women reported in 2002[2].
Risk factors[1][edit | edit source]
- Short stature
- Macrosomia
- Cephalopelvic disproportion
- Delayed/Prolonged labor
- Static position of the lower extremities during a prolonged second stage of labour[3]
- Mid forceps rotation
- Fetal malpositioning
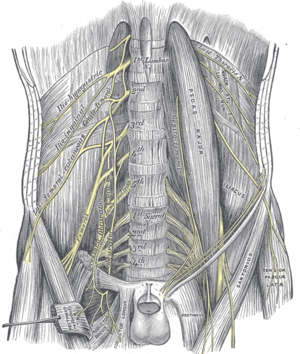
Clinically Relevant Anatomy[edit | edit source]
The lumbar plexus and sacral plexus, if taken as one entity becomes the lumbosacral plexus, the largest spinal nerve plexus. It consists of nerves originating from spinal segments L1 to S4, lumbar plexus taking its origin from L1 to L4 and sacral plexus from L5 to S4 respectively. Nerves arising from the lumbosacral plexus generally course behind the psoas major, piercing the abdominal wall antero-laterally, then course antero-medially, upon the pelvic rim or iliac crest to enter into the lower limb.
Mechanism of Injury / Pathological Process[edit | edit source]
The position of the lumbosacral plexus predisposes itself to compression during prolonged labour, especially in women who are of short stature with cephalopelvic disproportion. Any trauma, or compression or injury to the trunks of the lumbosacral plexus causes clinical signs and symptoms in the mother that may result during or after labour.
Katirji et al. (2002) concluded that intrapartum foot drop occurs mostly in short women and is caused by lumbosacral trunk compression by the fetal head at the pelvic brim primary pathology being predominantly demyelination and recovery is complete in up to 5 months.[2]
The peroneal nerve is frequently affected and Hunerman (1892) attributed its frequency to its position in the lumbosacral plexus."
Types[edit | edit source]
Presentation of signs and symptoms and electro diagnostic studies have helped in differentiating lumbosacral plexopathy into sub-groups
Types according to research articles reviewed are
1. Intrapartum maternal lumbosacral plexopathy: it involves the lumbosacral plexopathy easily recognized while the woman is in labour[2]
2. Postpartum maternal lumbosacral plexopathy: this manifests after childbirth[4]
Electrodiagnostic studies further describes postpartum maternal lumbosacral plexopathy into Upper and Lower Lumbosacral Plexopathy. Upper lumbosacral plexopathy involves the muscles of the lower limb and affectation to motor and sensory functions, while ,lower plexopathy only involves the lower part of the plexus (s2-s4).Lower postpartum lumbosacral plexopathy is evoked when perineal sensory disturbances whether or not associated with urinary or fecal incontinence persist after a history of a difficult vaginal delivery with no associated lower limb sensory or motor deficits noted[4] "The first, second and third sacral roots entering into the formation of the sacral plexus lie on the piriformis muscle and are thus unprotected against pressure on the bone"[5]
Clinical Presentation[edit | edit source]
For the upper palsy:
- pain
- paraesthesia, sensory loss in the L‐5 dermatome
- weakness of ankle dorsiflexion, eversion, and inversion causing foot drop
For the lower palsy:[4]
- Perineal sensori-neuropathy
- Urinary incontinence
- Fecal incontinence
- Sexual dysfunction
Diagnostic Procedures[edit | edit source]
A detailed subjective history should be taken from the patient. Intrapartum palsy would have been observed during parturition.
Objective diagnostic procedures include the use of Electrodiagnostic devices vis a vis: EMG in determining the level of affectation. Compound Muscle Action Potential (CMAP), Sensory Nerve Action Potential (SNAP) are recorded to know the exact site of injury.
Outcome Measures[edit | edit source]
Functional Outcome Measure Scale (see Outcome Measures Database)
Physiotherapy Management / Interventions[edit | edit source]
Electrical Muscle Stimulation
Tactile Stimulation
Proprioceptive Neuromuscular Facilitation
Prescription of ankle foot orthoses
Differential Diagnosis[edit | edit source]
Spinal Cord Injury
Guillain-Barre Syndrome
Injection Neuritis
Resources[edit | edit source]
Feasby TE, Burton SR, Hahn AF. Obstetrical lumbosacral plexus injury. Muscle & Nerve: Official Journal of the American Association of Electrodiagnostic Medicine. 1992 Aug;15(8):937-40.
Ismael SS, Amarenco G, Bayle B, Kerdraon J. Postpartum lumbosacral plexopathy limited to autonomic and perineal manifestations: clinical and electrophysiological study of 19 patients. Journal of Neurology, Neurosurgery & Psychiatry. 2000 Jun 1;68(6):771-3.
References[edit | edit source]
[1]Feasby TE, Burton SR, Hahn AF. Obstetrical lumbosacral plexus injury. Muscle & Nerve: Official Journal of the American Association of Electrodiagnostic Medicine. 1992 Aug;15(8):937-40.
[2]Katirji B, Wilbourn AJ, Scarberry SL, Preston DC. Intrapartum maternal lumbosacral plexopathy. Muscle & nerve. 2002 Sep;26(3):340-7.
[4]Ismael SS, Amarenco G, Bayle B, Kerdraon J. Postpartum lumbosacral plexopathy limited to autonomic and perineal manifestations: clinical and electrophysiological study of 19 patients. Journal of Neurology, Neurosurgery & Psychiatry. 2000 Jun 1;68(6):771-3.
[5]Tillman AJ. Traumatic neuritis in the puerperium. American Journal of Obstetrics and Gynecology. 1935 May 1;29(5):660-6.