Diaphragmatic Breathing and Ventilator-Induced Diaphragmatic Dysfunction: Difference between revisions
(minor edits as suggested by Grammarly) |
No edit summary |
||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Carin Hunter|Carin Hunter]] based on the course by [https://members.physio-pedia.com/course_tutor/rina-pandya/ Rina Pandya]<br> '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | <div class="editorbox"> '''Original Editor '''- [[User:Carin Hunter|Carin Hunter]] based on the course by [https://members.physio-pedia.com/course_tutor/rina-pandya/ Rina Pandya]<br> '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== Effects of | == Effects of Diaphragmatic Breathing == | ||
# '''Detoxifies and | # '''Detoxifies and releases toxins:''' | ||
#* Our body is designed to release 70% of its toxins through breathing. At least 3x times per day for 39 seconds | #* Our body is designed to release 70% of its toxins through breathing. At least 3x times per day for 39 seconds | ||
# '''Anti-stress:'''<ref>Hunt MG, Rushton J, Shenberger E, Murayama S. [https://journals.humankinetics.com/view/journals/jcsp/12/1/article-p27.xml Positive effects of diaphragmatic breathing on physiological stress reactivity in varsity athletes.] Journal of Clinical Sport Psychology. 2018 Mar 1;12(1):27-38.</ref> | # '''Anti-stress:'''<ref>Hunt MG, Rushton J, Shenberger E, Murayama S. [https://journals.humankinetics.com/view/journals/jcsp/12/1/article-p27.xml Positive effects of diaphragmatic breathing on physiological stress reactivity in varsity athletes.] Journal of Clinical Sport Psychology. 2018 Mar 1;12(1):27-38.</ref> | ||
| Line 11: | Line 11: | ||
# '''Relaxation and mood elevation:'''<ref>Hamasaki H. [https://www.mdpi.com/2305-6320/7/10/65 Effects of Diaphragmatic Breathing on Health: A Narrative Review.] Medicines. 2020 Oct;7(10):65.</ref> | # '''Relaxation and mood elevation:'''<ref>Hamasaki H. [https://www.mdpi.com/2305-6320/7/10/65 Effects of Diaphragmatic Breathing on Health: A Narrative Review.] Medicines. 2020 Oct;7(10):65.</ref> | ||
#* Diaphragmatic breathing stimulates the vagus nerve which is parasympathetic, thus inducing relaxation. | #* Diaphragmatic breathing stimulates the vagus nerve which is parasympathetic, thus inducing relaxation. | ||
# '''Deep | # '''Deep breathing relieves pain:''' | ||
#* Breathing into pain will increase circulation to that specific area, relieves tension and increase oxygenation. This triggers the release of endorphins, thus affecting pain relief. | #* Breathing into pain will increase circulation to that specific area, relieves tension and increase oxygenation. This triggers the release of endorphins, thus affecting pain relief. | ||
# '''Deep | # '''Deep breathing enhances the immune system:''' | ||
#* Deep breathing enhances the body’s ability to metabolize nutrients and vitamins. Deep breathing aids in digestion which helps strengthen immunity. | #* Deep breathing enhances the body’s ability to metabolize nutrients and vitamins. Deep breathing aids in digestion which helps strengthen immunity. | ||
# '''Lowers blood pressure:''' | # '''Lowers blood pressure:''' | ||
#* With relaxation blood vessels dilate, which improves circulation and lowers blood pressure. Deep breathing also slows and regulates the heart rate, which also helps with lowering BP. | #* With relaxation blood vessels dilate, which improves circulation and lowers blood pressure. Deep breathing also slows and regulates the heart rate, which also helps with lowering BP. | ||
# '''Deep | # '''Deep breathing improves cellular regeneration:''' | ||
#* With [[Diaphragmatic Breathing Exercises|deep breathing]] the body is better oxygenated and has better circulation which enhances the body’s efforts of cellular regeneration. | #* With [[Diaphragmatic Breathing Exercises|deep breathing]] the body is better oxygenated and has better circulation which enhances the body’s efforts of cellular regeneration. | ||
# '''Helps support correct posture.''' | # '''Helps support correct posture.''' | ||
| Line 28: | Line 28: | ||
{{#ev:youtube|v=1vXlTkrNxyw}} | {{#ev:youtube|v=1vXlTkrNxyw}} | ||
== Evidence Based Practice | == Evidence Based Practice == | ||
Moreover, patients with chronic lower back pain have often been reported to have defects in posture and motor control.<ref>O’Sullivan P. [https://www.sciencedirect.com/science/article/abs/pii/S1356689X05001104 Diagnosis and classification of chronic low back pain disorders: maladaptive movement and motor control impairments as underlying mechanism.] Manual therapy. 2005 Nov 1;10(4):242-55.</ref><ref>Hodges PW, Moseley GL. [https://www.sciencedirect.com/science/article/abs/pii/S1050641103000427 Pain and motor control of the lumbopelvic region: effect and possible mechanisms]. Journal of electromyography and kinesiology. 2003 Aug 1;13(4):361-70.</ref> | * Allison et al.<ref>Allison G, Kendle K, Roll S, Schupelius J, Scott Q, Panizza J. [https://www.sciencedirect.com/science/article/pii/S000495141460369X The role of the diaphragm during abdominal hollowing exercises.] Australian Journal of Physiotherapy. 1998 Jan 1;44(2):95-102.</ref> reported that during lumbopelvic motion control tests, diaphragmatic activity increases in healthy subjects. | ||
* O’Sullivan and Beales<ref name=":0" /> concluded in their case studies that lumbopelvic movements decrease in patients with diaphragmatic injuries. | |||
* Moreover, patients with chronic lower back pain have often been reported to have defects in posture and motor control.<ref name=":0">O’Sullivan P. [https://www.sciencedirect.com/science/article/abs/pii/S1356689X05001104 Diagnosis and classification of chronic low back pain disorders: maladaptive movement and motor control impairments as underlying mechanism.] Manual therapy. 2005 Nov 1;10(4):242-55.</ref><ref>Hodges PW, Moseley GL. [https://www.sciencedirect.com/science/article/abs/pii/S1050641103000427 Pain and motor control of the lumbopelvic region: effect and possible mechanisms]. Journal of electromyography and kinesiology. 2003 Aug 1;13(4):361-70.</ref> | |||
== Effect of | == Effect of Mechanical Ventilation on Diaphragm == | ||
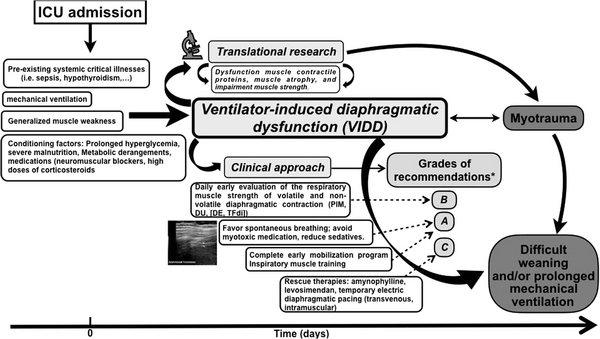
* '''Ventilator-induced diaphragmatic dysfunction(VIDD):''' | *'''Ventilator-induced diaphragmatic dysfunction(VIDD):''' | ||
** Loss of diaphragmatic force-generating capacity as a consequence to use of [[Ventilation and Weaning|mechanical ventilation]] due to suppressed inspiratory effort.<ref>Kim WY, Lim CM. [http://rc.rcjournal.com/content/62/11/1485.short Ventilator-induced diaphragmatic dysfunction: diagnosis and role of pharmacological agents.] Respiratory care. 2017 Nov 1;62(11):1485-91.</ref><ref>Peñuelas O, Keough E, López-Rodríguez L, Carriedo D, Gonçalves G, Barreiro E, Lorente JÁ. [https://icm-experimental.springeropen.com/articles/10.1186/s40635-019-0259-9 Ventilator-induced diaphragm dysfunction: translational mechanisms lead to therapeutical alternatives in the critically ill.] Intensive care medicine experimental. 2019 Jul;7(1):1-25.</ref> | ** Loss of diaphragmatic force-generating capacity as a consequence to use of [[Ventilation and Weaning|mechanical ventilation]] due to suppressed inspiratory effort.<ref>Kim WY, Lim CM. [http://rc.rcjournal.com/content/62/11/1485.short Ventilator-induced diaphragmatic dysfunction: diagnosis and role of pharmacological agents.] Respiratory care. 2017 Nov 1;62(11):1485-91.</ref><ref>Peñuelas O, Keough E, López-Rodríguez L, Carriedo D, Gonçalves G, Barreiro E, Lorente JÁ. [https://icm-experimental.springeropen.com/articles/10.1186/s40635-019-0259-9 Ventilator-induced diaphragm dysfunction: translational mechanisms lead to therapeutical alternatives in the critically ill.] Intensive care medicine experimental. 2019 Jul;7(1):1-25.</ref> | ||
* Mechanical ventilatory assistance contributes to diaphragm muscle inactivity and unloading thus leading to diaphragmatic atrophy and fatigue.<ref>Vassilakopoulos T, Petrof BJ. [https://www.atsjournals.org/doi/full/10.1164/rccm.200304-489CP Ventilator-induced diaphragmatic dysfunction.] American journal of respiratory and critical care medicine. 2004 Feb 1;169(3):336-41.</ref> | * Mechanical ventilatory assistance contributes to diaphragm muscle inactivity and unloading thus leading to diaphragmatic atrophy and fatigue.<ref>Vassilakopoulos T, Petrof BJ. [https://www.atsjournals.org/doi/full/10.1164/rccm.200304-489CP Ventilator-induced diaphragmatic dysfunction.] American journal of respiratory and critical care medicine. 2004 Feb 1;169(3):336-41.</ref> | ||
* Diaphragm weakness is a leading cause of difficult weaning from mechanical ventilation<ref>Dres M, Dubé BP, Mayaux J, Delemazure J, Reuter D, Brochard L, Similowski T, Demoule A. [https://www.atsjournals.org/doi/full/10.1164/rccm.201602-0367OC Coexistence and impact of limb muscle and diaphragm weakness at the time of liberation from mechanical ventilation in medical intensive care unit patients.] American journal of respiratory and critical care medicine. 2017 Jan 1;195(1):57-66.</ref> and loss of thickness of diaphragm muscle, however, if there is insufficient ventilatory support and diaphragm is not unloaded adequately | * Diaphragm weakness is a leading cause of difficult weaning from mechanical ventilation<ref>Dres M, Dubé BP, Mayaux J, Delemazure J, Reuter D, Brochard L, Similowski T, Demoule A. [https://www.atsjournals.org/doi/full/10.1164/rccm.201602-0367OC Coexistence and impact of limb muscle and diaphragm weakness at the time of liberation from mechanical ventilation in medical intensive care unit patients.] American journal of respiratory and critical care medicine. 2017 Jan 1;195(1):57-66.</ref> and loss of thickness of diaphragm muscle, however, if there is insufficient ventilatory support and the diaphragm is not unloaded adequately this can lead to load-induced inflammation and injury.<ref>Orozco-Levi M, Lloreta J, Minguella J, Serrano S, Broquetas JM, Gea J. [https://www.atsjournals.org/doi/full/10.1164/ajrccm.164.9.2011150 Injury of the human diaphragm associated with exertion and chronic obstructive pulmonary disease.] American journal of respiratory and critical care medicine. 2001 Nov 1;164(9):1734-9.</ref> | ||
* Diaphragm atrophy developing during mechanical ventilation strongly impacts clinical outcomes. Targeting an inspiratory effort level similar to that of healthy subjects at rest might accelerate liberation from ventilation.<ref>Lipson DA, Barnacle H, Birk R, Brealey N, Locantore N, Lomas DA, Ludwig-Sengpiel A, Mohindra R, Tabberer M, Zhu CQ, Pascoe SJ. [https://www.atsjournals.org/doi/full/10.1164/rccm.201703-0449OC FULFIL trial: once-daily triple therapy for patients with chronic obstructive pulmonary disease.] American journal of respiratory and critical care medicine. 2017 Aug 15;196(4):438-46.</ref>[[File:VIDD Flow chart - recreated.jpg|center|thumb|600x600px|Ventilator-Induced Diaphragmatic Dysfunction Flow chart <ref>Schepens T, Dres M, Heunks L, Goligher EC. [https://journals.lww.com/co-criticalcare/Abstract/2019/02000/Diaphragm_protective_mechanical_ventilation.12.aspx Diaphragm-protective mechanical ventilation.] Current opinion in critical care. 2019 Feb 1;25(1):77-85.</ref>]] | * Diaphragm atrophy developing during mechanical ventilation strongly impacts clinical outcomes. Targeting an inspiratory effort level similar to that of healthy subjects at rest might accelerate liberation from ventilation.<ref>Lipson DA, Barnacle H, Birk R, Brealey N, Locantore N, Lomas DA, Ludwig-Sengpiel A, Mohindra R, Tabberer M, Zhu CQ, Pascoe SJ. [https://www.atsjournals.org/doi/full/10.1164/rccm.201703-0449OC FULFIL trial: once-daily triple therapy for patients with chronic obstructive pulmonary disease.] American journal of respiratory and critical care medicine. 2017 Aug 15;196(4):438-46.</ref>[[File:VIDD Flow chart - recreated.jpg|center|thumb|600x600px|Ventilator-Induced Diaphragmatic Dysfunction Flow chart <ref>Schepens T, Dres M, Heunks L, Goligher EC. [https://journals.lww.com/co-criticalcare/Abstract/2019/02000/Diaphragm_protective_mechanical_ventilation.12.aspx Diaphragm-protective mechanical ventilation.] Current opinion in critical care. 2019 Feb 1;25(1):77-85.</ref>]] | ||
[[File:VIDD Clinical practice guidelines- from article.webp|center|thumb|600x600px|Peñuelas O, Keough E, López-Rodríguez L, Carriedo D, Gonçalves G, Barreiro E, Lorente JÁ. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6658639/ Ventilator-induced diaphragm dysfunction: translational mechanisms lead to therapeutical alternatives in the critically ill.] Intensive care medicine experimental. 2019 Jul;7(1):1-25.]] | [[File:VIDD Clinical practice guidelines- from article.webp|center|thumb|600x600px|Peñuelas O, Keough E, López-Rodríguez L, Carriedo D, Gonçalves G, Barreiro E, Lorente JÁ. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6658639/ Ventilator-induced diaphragm dysfunction: translational mechanisms lead to therapeutical alternatives in the critically ill.] Intensive care medicine experimental. 2019 Jul;7(1):1-25.]] | ||
Revision as of 07:20, 10 November 2021
Top Contributors - Ewa Jaraczewska, Carin Hunter, Jess Bell, Kim Jackson and Wanda van Niekerk
Effects of Diaphragmatic Breathing[edit | edit source]
- Detoxifies and releases toxins:
- Our body is designed to release 70% of its toxins through breathing. At least 3x times per day for 39 seconds
- Anti-stress:[1]
- Brain releases cortisol, the “stress hormone” under stress and anxiety.
- By taking deep breaths, heart rate slows, more oxygen enters the bloodstream and ultimately communicates with the brain to relax.
- Deep breathing increases the endorphins.
- Relaxation and mood elevation:[2]
- Diaphragmatic breathing stimulates the vagus nerve which is parasympathetic, thus inducing relaxation.
- Deep breathing relieves pain:
- Breathing into pain will increase circulation to that specific area, relieves tension and increase oxygenation. This triggers the release of endorphins, thus affecting pain relief.
- Deep breathing enhances the immune system:
- Deep breathing enhances the body’s ability to metabolize nutrients and vitamins. Deep breathing aids in digestion which helps strengthen immunity.
- Lowers blood pressure:
- With relaxation blood vessels dilate, which improves circulation and lowers blood pressure. Deep breathing also slows and regulates the heart rate, which also helps with lowering BP.
- Deep breathing improves cellular regeneration:
- With deep breathing the body is better oxygenated and has better circulation which enhances the body’s efforts of cellular regeneration.
- Helps support correct posture.
- Inspiration lengthens the spine, facilitates lumbopelvic movements, activates core muscles.[3]
Evidence Based Practice[edit | edit source]
- Allison et al.[4] reported that during lumbopelvic motion control tests, diaphragmatic activity increases in healthy subjects.
- O’Sullivan and Beales[5] concluded in their case studies that lumbopelvic movements decrease in patients with diaphragmatic injuries.
- Moreover, patients with chronic lower back pain have often been reported to have defects in posture and motor control.[5][6]
Effect of Mechanical Ventilation on Diaphragm[edit | edit source]
- Ventilator-induced diaphragmatic dysfunction(VIDD):
- Loss of diaphragmatic force-generating capacity as a consequence to use of mechanical ventilation due to suppressed inspiratory effort.[7][8]
- Mechanical ventilatory assistance contributes to diaphragm muscle inactivity and unloading thus leading to diaphragmatic atrophy and fatigue.[9]
- Diaphragm weakness is a leading cause of difficult weaning from mechanical ventilation[10] and loss of thickness of diaphragm muscle, however, if there is insufficient ventilatory support and the diaphragm is not unloaded adequately this can lead to load-induced inflammation and injury.[11]
- Diaphragm atrophy developing during mechanical ventilation strongly impacts clinical outcomes. Targeting an inspiratory effort level similar to that of healthy subjects at rest might accelerate liberation from ventilation.[12]
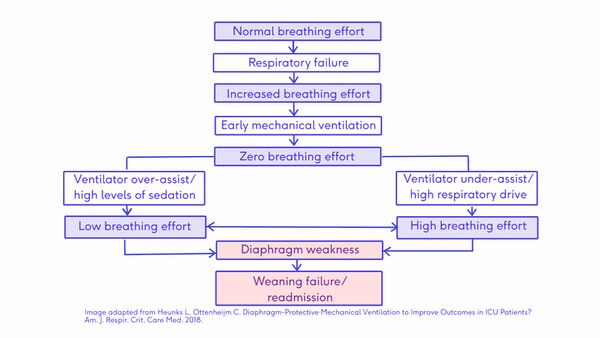 Ventilator-Induced Diaphragmatic Dysfunction Flow chart [13]
Ventilator-Induced Diaphragmatic Dysfunction Flow chart [13]
References[edit | edit source]
- ↑ Hunt MG, Rushton J, Shenberger E, Murayama S. Positive effects of diaphragmatic breathing on physiological stress reactivity in varsity athletes. Journal of Clinical Sport Psychology. 2018 Mar 1;12(1):27-38.
- ↑ Hamasaki H. Effects of Diaphragmatic Breathing on Health: A Narrative Review. Medicines. 2020 Oct;7(10):65.
- ↑ Stephens RJ, Haas M, Moore III WL, Emmil JR, Sipress JA, Williams A. Effects of diaphragmatic breathing patterns on balance: a preliminary clinical trial. Journal of manipulative and physiological therapeutics. 2017 Mar 1;40(3):169-75.
- ↑ Allison G, Kendle K, Roll S, Schupelius J, Scott Q, Panizza J. The role of the diaphragm during abdominal hollowing exercises. Australian Journal of Physiotherapy. 1998 Jan 1;44(2):95-102.
- ↑ 5.0 5.1 O’Sullivan P. Diagnosis and classification of chronic low back pain disorders: maladaptive movement and motor control impairments as underlying mechanism. Manual therapy. 2005 Nov 1;10(4):242-55.
- ↑ Hodges PW, Moseley GL. Pain and motor control of the lumbopelvic region: effect and possible mechanisms. Journal of electromyography and kinesiology. 2003 Aug 1;13(4):361-70.
- ↑ Kim WY, Lim CM. Ventilator-induced diaphragmatic dysfunction: diagnosis and role of pharmacological agents. Respiratory care. 2017 Nov 1;62(11):1485-91.
- ↑ Peñuelas O, Keough E, López-Rodríguez L, Carriedo D, Gonçalves G, Barreiro E, Lorente JÁ. Ventilator-induced diaphragm dysfunction: translational mechanisms lead to therapeutical alternatives in the critically ill. Intensive care medicine experimental. 2019 Jul;7(1):1-25.
- ↑ Vassilakopoulos T, Petrof BJ. Ventilator-induced diaphragmatic dysfunction. American journal of respiratory and critical care medicine. 2004 Feb 1;169(3):336-41.
- ↑ Dres M, Dubé BP, Mayaux J, Delemazure J, Reuter D, Brochard L, Similowski T, Demoule A. Coexistence and impact of limb muscle and diaphragm weakness at the time of liberation from mechanical ventilation in medical intensive care unit patients. American journal of respiratory and critical care medicine. 2017 Jan 1;195(1):57-66.
- ↑ Orozco-Levi M, Lloreta J, Minguella J, Serrano S, Broquetas JM, Gea J. Injury of the human diaphragm associated with exertion and chronic obstructive pulmonary disease. American journal of respiratory and critical care medicine. 2001 Nov 1;164(9):1734-9.
- ↑ Lipson DA, Barnacle H, Birk R, Brealey N, Locantore N, Lomas DA, Ludwig-Sengpiel A, Mohindra R, Tabberer M, Zhu CQ, Pascoe SJ. FULFIL trial: once-daily triple therapy for patients with chronic obstructive pulmonary disease. American journal of respiratory and critical care medicine. 2017 Aug 15;196(4):438-46.
- ↑ Schepens T, Dres M, Heunks L, Goligher EC. Diaphragm-protective mechanical ventilation. Current opinion in critical care. 2019 Feb 1;25(1):77-85.






