Obstructed Defecation Syndrome: Difference between revisions
No edit summary |
No edit summary |
||
| Line 17: | Line 17: | ||
== Clinical Presentation == | == Clinical Presentation == | ||
The patient will have symptoms of the need to strain with bowel movement, episodes of incomplete evacuation, fragmented stool, pelvic heaviness, and sometimes accidental bowel leakage. | |||
Frequent, prolonged straining becomes the prime mover. may cause stretch on the pudendal nerve and pudendal neuropathy causing rectal hyposensation, internal organ descends (prolapse), muscle weakness, and spending too much time than usual in toilet. Lower abdominal/rectal pain, feeling of incomplete evacuation of the rectum. The patient will tend to use perineal manipulation to help with the evacuation. | |||
Pat with ODS will have a small, more hard stool and difficulty to evacuate, responses to laxatives and enema, and less effective to trigger the peristaltic reflex. | |||
[[Fecal Incontinence|Fecal incontinence]] one of the symptoms of ODS. | |||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
Revision as of 00:16, 22 April 2021
Top Contributors - Khloud Shreif, Temitope Olowoyeye, Kim Jackson and Aminat Abolade
Clinically Relevant Anatomy[edit | edit source]
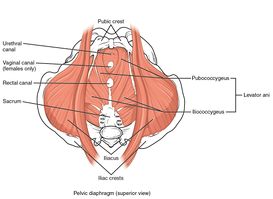
The levator ani muscles as a component of pelvic floor diaphragm ( the iliococcygeus, the pubococcygeal, and the puborectalis muscles) in addition to its role as a supportive structure and keeping visceral and internal organs in place. levator ani muscles specifically puborectalis have a role to maintain the urinary and fecal continence, contraction, and relaxation of puborectalis, lower abdominal muscles, and anal sphincter work synchronically for normal and smooth defecation.
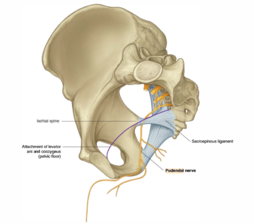
The pudendal nerve innervates the external anal sphincter and part of the puborectalis muscle, with frequent and prolonged straining that may stretch the pudendal nerve causing pudendal neuropathy.
While we have voluntary control over the external anal sphincter the internal anal sphincter muscles are involuntary muscles affected by the rectum, it is relaxed if the rectum filled with stool and vice versa, so the sensitivity of the rectum is important for normal physiology.
Mechanism of Injury / Pathological Process[edit | edit source]
Obstructive defecation syndrome ODS is a term related to constipation, and one of the underlying causes of fecal incontinence, it is a common condition of inability of a person to evacuate the rectum properly/ reduce bowel movement.
Clinical Presentation[edit | edit source]
The patient will have symptoms of the need to strain with bowel movement, episodes of incomplete evacuation, fragmented stool, pelvic heaviness, and sometimes accidental bowel leakage.
Frequent, prolonged straining becomes the prime mover. may cause stretch on the pudendal nerve and pudendal neuropathy causing rectal hyposensation, internal organ descends (prolapse), muscle weakness, and spending too much time than usual in toilet. Lower abdominal/rectal pain, feeling of incomplete evacuation of the rectum. The patient will tend to use perineal manipulation to help with the evacuation.
Pat with ODS will have a small, more hard stool and difficulty to evacuate, responses to laxatives and enema, and less effective to trigger the peristaltic reflex.
Fecal incontinence one of the symptoms of ODS.
Diagnostic Procedures[edit | edit source]
add text here relating to diagnostic tests for the condition
Outcome Measures[edit | edit source]
add links to outcome measures here (see Outcome Measures Database)
Management / Interventions[edit | edit source]
add text here relating to management approaches to the condition
Differential Diagnosis[edit | edit source]
add text here relating to the differential diagnosis of this condition
Resources[edit | edit source]
add appropriate resources here