Clinical Frailty Scale: Difference between revisions
No edit summary |
No edit summary |
||
| Line 24: | Line 24: | ||
=== Reliability === | === Reliability === | ||
Clinical Frailty Scale is a reliable instrument to identify frailty in the emergency department. It might provide ED clinicians with useful information for decision-making with triage, disposition, and treatment.<ref>Kaeppeli T, Rueegg M, Dreher-Hummel T, Brabrand M, Kabell-Nissen S, Carpenter CR, Bingisser R, Nickel CH. [https://www.sciencedirect.com/science/article/abs/pii/S0196064420302183#:~:text=Among%202%2C393%20patients%2C%20the%20Clinical,and%20demonstrated%20good%20interrater%20reliability. Validation of the clinical frailty scale for prediction of thirty-day mortality in the emergency department.] Annals of emergency medicine. 2020 Sep 1;76(3):291-300.</ref> | Clinical Frailty Scale is a reliable instrument to identify frailty in the emergency department. It might provide ED clinicians with useful information for decision-making with triage, disposition, and treatment.<ref>Kaeppeli T, Rueegg M, Dreher-Hummel T, Brabrand M, Kabell-Nissen S, Carpenter CR, Bingisser R, Nickel CH. [https://www.sciencedirect.com/science/article/abs/pii/S0196064420302183#:~:text=Among%202%2C393%20patients%2C%20the%20Clinical,and%20demonstrated%20good%20interrater%20reliability. Validation of the clinical frailty scale for prediction of thirty-day mortality in the emergency department.] Annals of emergency medicine. 2020 Sep 1;76(3):291-300.</ref> Applying the CFS to patients requires a clinical judgment of the examining clinician and thus may lead to inter-observer variation<ref name=":1" />. The inter-rater reliability of the CFS is generally very good however a number of biases may play a role in scoring, especially with clinicians who are inexperienced using the scale<ref>https://www.physiospot.com/research/frailty-scale-classification-tree/ Accessed on 27/2/21</ref>. In light of this a new classification tree to improve CFS scoring by inexperienced raters has been created. | ||
=== Validity === | === Validity === | ||
CFS score is a valid diagnostic instrument to measure frailty in older hospitalized patients and patients in emergency department.<ref>Stille K, Temmel N, Hepp J, Herget-Rosenthal S. [https://link.springer.com/article/10.1007/s41999-020-00370-7 Validation of the Clinical Frailty Scale for retrospective use in acute care]. European Geriatric Medicine. 2020 Dec;11(6):1009-15.</ref> CFS-Korean version is a valid scale for measuring frailty in older Korean patients | CFS score is a valid diagnostic instrument to measure frailty in older hospitalized patients and patients in the emergency department.<ref>Stille K, Temmel N, Hepp J, Herget-Rosenthal S. [https://link.springer.com/article/10.1007/s41999-020-00370-7 Validation of the Clinical Frailty Scale for retrospective use in acute care]. European Geriatric Medicine. 2020 Dec;11(6):1009-15.</ref> CFS-Korean version is a valid scale for measuring frailty in older Korean patients | ||
=== Responsiveness === | === Responsiveness === | ||
Revision as of 14:05, 27 February 2021
Original Editor - User Name
Top Contributors - Vidya Acharya, Lucinda hampton and Aminat Abolade
Objective[edit | edit source]
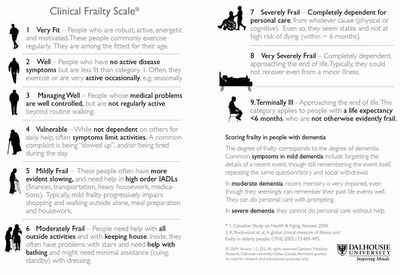
Clinical Frailty Scale (CFS) is used commonly to assess frailty. The CFS is utilized to predict the outcomes of older people hospitalized with acute illnesses.[1] The CFS is commonly used to predict health outcomes that are significantly associated are mortality, comorbidity, functional decline, mobility, and cognitive decline.
The scale was developed from the Canadian Study of Health and Aging, and it provides a summary tool for clinicians to assess frailty and fitness. Initially, it was scored on a scale from 1 (very fit) to 7 (severely frail). It was modified to a 9-point scale to include very severely frail and terminally ill.[1] It evaluates specific domains, including comorbidity, function, and cognition, to generate a frailty score ranging from 1 (very fit) to 9 (terminally ill).[2]
Intended Population[edit | edit source]
The frail elderly population, all individuals over the age of 70 years should be screened for frailty.[2]
Method of Use[edit | edit source]
It can be readily be administered in a clinical setting. Applying the CFS to patients is quick and requires data collection by watching the patient (mobilize), inquiring about their habitual physical activity and ability. The clinicians assess whether the patient can independently perform tasks such as bathing, dressing, housework, going upstairs, going out alone, going shopping, taking care of finances, taking medications, and preparing meals[2].
Technique[edit | edit source]
Evidence[edit | edit source]
Reliability[edit | edit source]
Clinical Frailty Scale is a reliable instrument to identify frailty in the emergency department. It might provide ED clinicians with useful information for decision-making with triage, disposition, and treatment.[3] Applying the CFS to patients requires a clinical judgment of the examining clinician and thus may lead to inter-observer variation[1]. The inter-rater reliability of the CFS is generally very good however a number of biases may play a role in scoring, especially with clinicians who are inexperienced using the scale[4]. In light of this a new classification tree to improve CFS scoring by inexperienced raters has been created.
Validity[edit | edit source]
CFS score is a valid diagnostic instrument to measure frailty in older hospitalized patients and patients in the emergency department.[5] CFS-Korean version is a valid scale for measuring frailty in older Korean patients
Responsiveness[edit | edit source]
Miscellaneous[edit | edit source]
Links[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Mendiratta P, Latif R. Clinical Frailty Scale. StatPearls [Internet]. 2020 Jun 22.
- ↑ 2.0 2.1 2.2 Church S, Rogers E, Rockwood K, Theou O. A scoping review of the Clinical Frailty Scale. BMC geriatrics. 2020 Dec;20(1):1-8.
- ↑ Kaeppeli T, Rueegg M, Dreher-Hummel T, Brabrand M, Kabell-Nissen S, Carpenter CR, Bingisser R, Nickel CH. Validation of the clinical frailty scale for prediction of thirty-day mortality in the emergency department. Annals of emergency medicine. 2020 Sep 1;76(3):291-300.
- ↑ https://www.physiospot.com/research/frailty-scale-classification-tree/ Accessed on 27/2/21
- ↑ Stille K, Temmel N, Hepp J, Herget-Rosenthal S. Validation of the Clinical Frailty Scale for retrospective use in acute care. European Geriatric Medicine. 2020 Dec;11(6):1009-15.