Gastroesophageal Reflux Disease: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) (Review - Formatting, grammar, images and references) |
||
| (37 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox">'''Original Editors '''- [http://www.physio-pedia.com/index.php5?title=User:Tessa_Puckett Tessa Puckett] [[Pathophysiology of Complex Patient Problems|from Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | |||
'''Original Editors '''- [http://www.physio-pedia.com/index.php5?title=User:Tessa_Puckett Tessa Puckett] [[Pathophysiology of Complex Patient Problems|from Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | |||
''' | |||
</div> | </div> | ||
== Definition/Description == | == Definition/Description == | ||
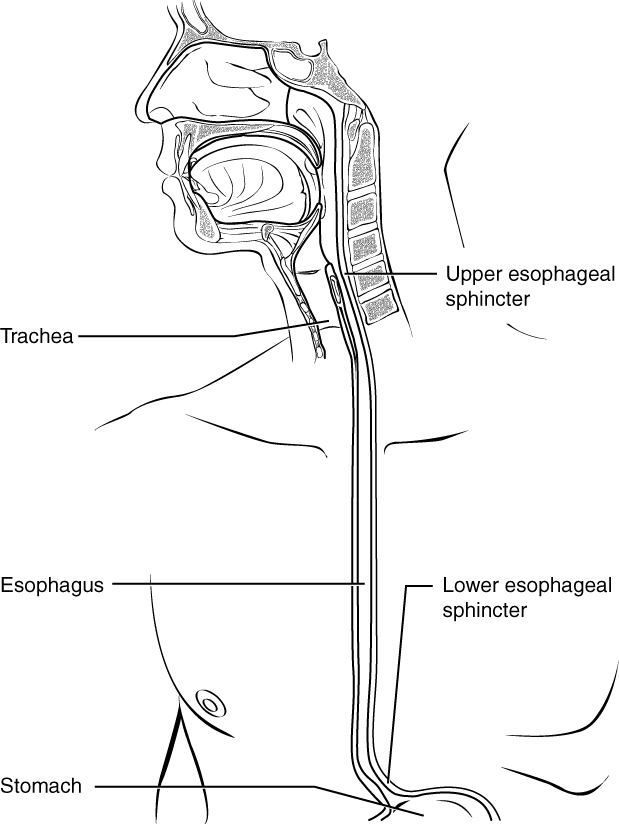
[[Image:Esophagus.jpg|frame|right|200x200px]]Gastroesophageal reflux disease (GERD), sometimes referred to as esophagitis, is a | [[Image:Esophagus.jpg|frame|right|200x200px]]Gastroesophageal reflux disease (GERD), sometimes referred to as esophagitis, is a complex disease with serious complications. It results from reflux (backward flow) of the stomach contents into the esophagus and causes trouble symptoms at least two times a week. Reflux of infectious agents, chemical irritants, physical agents, such as radiation and nasogastric intubation can cause GERD and can irritate and inflame the esophagus causing heartburn, belching, sore throat and other symptoms. <ref name="Pathology">Goodman CC, Fuller KS. Pathology: Implications for the Physical Therapist. 3rd ed. St. Louis: Saunders Elsevier; 2009.</ref><ref name="Differential Diagnosis">Goodman, Snyder. Differential Diagnosis for Physical Therapists: Screening for Referral. 4th Ed. Philadelphia: WB Saunders; 2003.</ref><ref name="PUB med">National Center for Biotechnology Information, U.S. National Library of Medicine. Gastroesophageal reflux disease. http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001311/ (accessed 17 March 2011).</ref><ref name="NEW" /> | ||
< | Heartburn is not another word for GERD, but is the most common symptom of the condition.<ref name="Pathology" /> GERD is the most common cause of heartburn, but there are other disorders that contribute to heartburn.<ref name="NEW" /> | ||
GERD can occur in infants and children. Infants typically grow out of the disease, and children with GERD present the same as adults.<ref name="Differential Diagnosis" /> | Although GERD is common in our society, it is rarely life-threatening, but can severely limit daily activities and productivity.<ref name="Shaker">Medical College of Wisconsin. Gastroenterology & Hepatology. http://www.mcw.edu/gastrohep.htm (accessed 21 April 2011).</ref> GERD can occur in infants and children. Infants typically grow out of the disease, and children with GERD present the same as adults.<ref name="Differential Diagnosis" /> | ||
< | {{#ev:youtube|o8iShP84HP4|300}} <ref>HealthGuru. Understanding GERD (GERD #1). http://www.youtube.com/watch?v=o8iShP84HP4&feature=youtu.be. Accessed on April 20, 2011.</ref> {{#ev:youtube|TdK0jRFpWPQ|300}}<ref>Mayoclinic. Heartburn, Acid Reflux, GERD-Mayo Clinic. http://www.youtube.com/watch?v=TdK0jRFpWPQ&feature=youtu.be. Accessed on April 20, 2011.</ref> | ||
== Prevalence == | == Prevalence == | ||
GERD is the most common gastrointestinal diagnosis recorded during visits to outpatient clinics. It is estimated that 14-20% of adults are affected, but the estimates are based on self-reported chronic heartburn. <ref name="NEW">Kahrilas, P.J. Gastroesophageal Reflux Disease. The New England Journal of Medicine.[serial on the Internet. (2006, Oct), [cited April 21, 2011]; 359(16): 1700-1707. Available from: PubMed.]</ref> | GERD is the most common gastrointestinal diagnosis recorded during visits to outpatient clinics. It is estimated that 14-20% of adults are affected, but the estimates are based on self-reported chronic heartburn. <ref name="NEW">Kahrilas, P.J. Gastroesophageal Reflux Disease. The New England Journal of Medicine.[serial on the Internet. (2006, Oct), [cited April 21, 2011]; 359(16): 1700-1707. Available from: PubMed.]</ref> Studies have shown that GERD is clinically silent in 24% of cases in which patients had difficult to control asthma<ref name="Prev" />. It can often be seen in:<ref name="Prev">Bor S., Kitapciogle G., Solak Z.A., et al. Prevalence of gastroesophageal reflux disease in patients with asthma and chronic obstructive pulmonary disease. JGHF [serial on the Internet. (2009), [cited April 21, 2011]; 25: 309-313. Available from: PubMed.]</ref> | ||
Studies have shown that GERD is clinically silent in 24% of cases in which patients had difficult to control asthma<ref name="Prev" /> | |||
*Patients with asthma | *Patients with asthma | ||
| Line 33: | Line 20: | ||
*Body Mass Index <u>></u> 25 with asthma and COPD<u></u> | *Body Mass Index <u>></u> 25 with asthma and COPD<u></u> | ||
== Characteristics/Clinical Presentation == | |||
Pain in the lower substernal area can arise as a result of relfux or GERD; it is commonly described as "heartburn" or "indigestion". GERD is also described as gripping, squeezing or burning sensations in the substernal area.<ref name="Differential Diagnosis" /><ref name="PUB med" /> | |||
Pain in the lower substernal | |||
Onset of GERD can occur when lying flat on the back, after meals, or bending forward and is usually worse at night. It is important to note that reflux or GERD is often confused with angina or a heart attack and should be reported to the doctor. GERD is not typically exercise induced and is relieved with antacids; this can help differentiate between angina/heart attack and reflux. | Onset of GERD can occur when lying flat on the back, after meals, or bending forward and is usually worse at night. It is important to note that reflux or GERD is often confused with angina or a heart attack and should be reported to the doctor. GERD is not typically exercise induced and is relieved with antacids; this can help differentiate between angina/heart attack and reflux. | ||
Chest pain referred from the upper gastrointestinal tract can radiate from the chest posteriorly to the upper back or interscapular or subscapular regions from vertebrae T10 - L2. | Chest pain referred from the upper gastrointestinal tract can radiate from the chest posteriorly to the upper back or interscapular or subscapular regions from vertebrae T10 - L2. | ||
'''Common Symptoms:''' | '''Common Symptoms:''' | ||
| Line 49: | Line 32: | ||
*[http://www.nlm.nih.gov/medlineplus/heartburn.html Heartburn ] | *[http://www.nlm.nih.gov/medlineplus/heartburn.html Heartburn ] | ||
*Bitter/sour taste in the back of the throat | *Bitter/sour taste in the back of the throat | ||
*Sense of a lump in the throat | *Sense of a lump in the throat | ||
*Abdominal bloating/Abdominal discomfort | *Abdominal bloating/Abdominal discomfort | ||
*Gas | *Gas | ||
*Chronic Cough | *Chronic Cough | ||
| Line 58: | Line 41: | ||
*Intense sharp pain behind sternum with radiation to the back | *Intense sharp pain behind sternum with radiation to the back | ||
<br> | <br>'''Less Common Symptoms:''' | ||
'''Less Common Symptoms:''' | |||
*Difficulty swallowing (dysphagia) | *Difficulty swallowing (dysphagia) | ||
| Line 66: | Line 47: | ||
*Hoarseness or change in voice | *Hoarseness or change in voice | ||
*Sore throat | *Sore throat | ||
*Wheezing | *Wheezing | ||
*Ear Ache | *Ear Ache | ||
== Associated Co-morbidities == | == Associated Co-morbidities == | ||
Patients with a past medical history of alcoholism, cirrhosis of the liver, peptic ulcers, esophageal varices, esophageal cancer, and long term use of NSAID's are more likely to have symptoms of GERD and should have diagnostic tests performed to rule out more severe conditions or diagnose GERD. It is typical for patients with GERD to have multiple risk factors. Some of the factors that predispose patients to pathologic reflux are: <ref name="NEW" /><ref name="Pathology" /> | |||
' | |||
*Lower esophageal Sphincter hypotension | *Lower esophageal Sphincter hypotension | ||
*Loss of esophagel peristaltic function | *Loss of esophagel peristaltic function | ||
| Line 84: | Line 57: | ||
*Increased compliance of the hiatal canal | *Increased compliance of the hiatal canal | ||
*Gastric hypersecretory states | *Gastric hypersecretory states | ||
*[http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001342/ Delayed gastric emptying] | *[http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001342/ Delayed gastric emptying] | ||
*[http://www.gerd.net/Basics/pregnancy.html Pregnancy] | *[http://www.gerd.net/Basics/pregnancy.html Pregnancy] | ||
*[http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001465/ Scleroderma] | *[http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001465/ Scleroderma] | ||
*[http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0002122/ Hiatal hernia] | *[http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0002122/ Hiatal hernia] <ref name="Differential Diagnosis" /> | ||
== Medications == | |||
'''<u> | Medications used to treat symptoms of GERD include: Antacids, Histamine 2 Receptor Blockers, and Proton Pump Inhibitors. Indefinite treatment with proton-pump inhibitors or H<sub>2</sub>-blockers as needed to maintain symptom control<ref name="Differential Diagnosis" />.There are risks associated with long term use of proton-pump inhibitors.<ref name="NEW" /><sub></sub>'''<u></u>''' | ||
=== Antacids === | |||
*Neutralizes the acid | *Neutralizes the acid | ||
*Does not reduce it (same amount of acid is produced) | *Does not reduce it (same amount of acid is produced) | ||
| Line 108: | Line 72: | ||
*Includes Mylanta, Maalox, Tums, Rolaids | *Includes Mylanta, Maalox, Tums, Rolaids | ||
=== Histamine-2 Receptor Blockers'''<u><sub></sub></u>''' === | |||
'''<u> | |||
*Reduce stomach acid produced by the stomach | *Reduce stomach acid produced by the stomach | ||
*Some are sold over the counter | *Some are sold over the counter | ||
*Over the Counter H2 Blockers: Pepcid, Zantac, Tagamet, and Axid | *Over the Counter H2 Blockers: Pepcid, Zantac, Tagamet, and Axid | ||
'''<u></u>''' | '''<u></u>''' | ||
=== Proton Pump Inihibitors === | |||
*Most potent acid-suppressing agent | *Most potent acid-suppressing agent | ||
*Stops acid from forming, instead of neutralizing it | *Stops acid from forming, instead of neutralizing it | ||
| Line 136: | Line 84: | ||
*PPI's can mask more serious conditions in the esophagus and stomach | *PPI's can mask more serious conditions in the esophagus and stomach | ||
*Over the counter PPI's: Prilosec (omeprazole) and Zegerid | *Over the counter PPI's: Prilosec (omeprazole) and Zegerid | ||
*PPI's requiring a prescription: Prevacid, Protonix, Nexium (esomperalzole), and Aciphex<br> | *PPI's requiring a prescription: Prevacid, Protonix, Nexium (esomperalzole), and Aciphex<br><span id="fck_dom_range_temp_1302025510728_222"></span><span id="fck_dom_range_temp_1302025510728_532"></span>People taking the above listed medications should report to the doctor if they have complaints of headache, constipation, diarrhoea, abdominal pain, or dizziness. | ||
People taking the above listed medications should report to the doctor if they have complaints of headache, constipation, | |||
It is essential for the physical therapist to take note of the patient's medications; listen for complaints of headache, constipation, diarrhoea, abdominal pain and dizziness; and report those findings to the doctor. | |||
== Diagnostic Tests/Lab Tests/Lab Values == | |||
Diagnostic tests are not typically needed unless the symptoms are severe. Physicians will order diagnostic tests to diagnose GERD or other complications if there are severe symptoms, the symptoms are not relieved with medications or the symptoms returned. Severe symptoms include dysphagia, odynophagia, bleeding, weight loss, anemia, and those at risk for Barrett's esophagus.<ref name="PUB med" /><ref name="NEW" /> Commonly used diagnostic tests used to diagnose GERD are discussed below. | |||
=== Esophagogastroduodenoscopy === | |||
A procedure where a small camera is placed at the end of flexible tube; the tube is inserted into the mouth and down the throat and examines the lining of the esophagus, stomach and upper duodenum<ref name="Shaker" /><ref name="EGD">National Center for Biotechnology Information, U.S. National Library of Medicine. EGD - esophagogastroduodenoscopy. http://www.nlm.nih.gov/medlineplus/ency/article/003888.htm (accessed 19 April 2011).</ref> | |||
=== Barium Swallow === | |||
This is a special type of imaging that requires the patient to drink barium before undergoing an x-ray. This produces clear images of the upper digestive tract.<ref name="Harvard">Harvard Health Publications. Harvard Medical School. Barium Swallow (Upper Gastrointestinal Series or "Upper GI Series"). http://www.health.harvard.edu/diagnostic-tests/barium-swallow.htm (accessed 21 April 2011).</ref> | |||
=== Continuous Esophageal pH Monitoring === | |||
This procedure involves a thin tube being inserted into the esophagus, through the mouth, to measure acid levels and the pH<ref name="Shaker" /> | |||
=== Esophageal Manometry === | |||
This procedure requires a thin tube to be inserted into the esophagus, through the mouth or nose, to measure the pressure of the esophagus<ref name="Shaker" /> | |||
== Etiology/Causes == | == Etiology/Causes == | ||
[[File:GERD.png|right|frameless|360x360px]] | |||
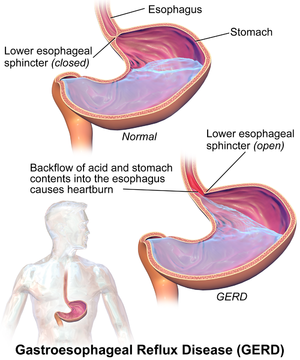
The lower esophageal sphincter (LES) is a ring of muscle fibers that functions to close the opening between the esophagus and the stomach. When the LES is not functioning properly, the stomach contents (food, liquid, and stomach acid) can move backward into the esophagus causing damage to the esophagus. The backward flow of food from the stomach into the esphophagus is called reflux. <ref name="PUB med" /><br> | |||
*Obesity | *Obesity | ||
*Smoking | *Smoking | ||
*Alcohol | *Alcohol | ||
*Medications | *Medications | ||
*Lower Esophageal Sphincter (LES) Dysfunction | *Lower Esophageal Sphincter (LES) Dysfunction | ||
Some of the medications that can cause GERD or make it worse are:<ref name="PUB med" /> | |||
* Nonsteroidal anti-inflammatory drugs (NSAID's) - Advil (ibruprofen), Motrin, Aleve | |||
* Anticholinergics - Bentyl | |||
* Beta Blockers - Toprol XL | |||
* Bronchodilators - Advair | |||
* Calcium Channel Blockers - Norvasc | |||
* Hormone Replacement Therapy - Progesterone | |||
* Sedatives (benzodiazepines) - Valium, Xanax | |||
* Tricyclic Antidepressants: Doxepin | |||
== Systemic Involvement == | == Systemic Involvement == | ||
=== Musculoskeletal === | |||
Untreated ulcers can cause biomechanical changes in muscular contractions and spinal movement. Patient may present with musculoskeletal deficits or dysfunctions because of the untreated ulcer. It is important for the physical therapist to take a good medical history to reveal actual cause of musculoskeletal dysfunction. Patients may think that heartburn while lying flat, difficulty swallowing, or chronic cough is unrelated to their recent onset of midscapular pain or thoracic back pain; thus, it is imperative to ask the patient if they have had any symptoms of GERD and if they are being treated by a medical doctor for the diagnosis.<ref name="Differential Diagnosis" /> <br> | |||
Untreated ulcers can cause biomechanical changes in muscular contractions and spinal movement. Patient may present with musculoskeletal deficits or dysfunctions because of the untreated ulcer. It is important for the physical therapist to take a good medical history to reveal actual cause of musculoskeletal dysfunction. Patients may think that heartburn while lying flat, difficulty swallowing, or chronic cough is unrelated to their recent onset of midscapular pain or thoracic back pain; thus, it is imperative to ask the patient if they have had any symptoms of GERD and if they are being treated by a medical doctor for the diagnosis.<ref name="Differential Diagnosis" / | |||
=== Dental === | |||
GERD can cause irreversible dental erosion of the posterior surface of the teeth. Possible symptoms associated with dental erosion included vomiting, experiencing sour taste, belching, heartburn, stomach ache and pain on awakening. Oral Symptoms include: burning mouth syndrome, tooth sensitivity, loss of the vertical dimension of cculsion and aesthetic disfigurement.<ref name="Dental" /> | |||
| === Respiratory === | ||
Gastric acid in the airways can cause bronchoconstriction which increases bronchial activity. Acid in the esophagus releases substance P and neurokinin A in the bronchial mucosa causing a neuroinflammatory reflex mechanism and airway edema. An increase in asthma severity is caused from an increase in vagal efferent impulses and the results of acid being in the esophagus and the airways.<ref name="LUNG">Böcskei C, Viczián M, Böcskei R, Horváth I. The influence of gastroesophageal reflux disease and its treatment on asthmatic cough. Lung. [serial on the Internet. (2005 Jan-Feb), [cited April 21, 2011]; 183(1): 53–62. Available from: PubMed.]</ref> | |||
| === Gastrointestinal === | ||
GERD is a risk factor for Barrett's esophagus and is linked to esophageal adenocarcinoma. Barrett's esophagus is a precancerous condition, in which the normal squamous epithelium is replaced by specialized metaplastic columnar cell-lined eipthelium.<ref name="ESO">Veugelers PJ, Porter GA, Guernsey DL, Casson AG. Obesity and lifestyle risk factors for gastroesophageal reflux disease, Barrett esophagus and esophageal adenocarcinoma.Diseases of the Esophagus.[serial on the Internet. (2006), [cited April 21, 2011]; 19(5): 321–328. Available from: PubMed.]</ref> Chronic GERD is a major risk for esophageal adenocarcinoma.<ref name="Differential Diagnosis" /> | |||
== Medical Management == | |||
If lifestyle changes and medications do not help the symptoms of GERD, the individual may be considered for surgical management.<br> | |||
< | === Nissen Fundoplication === | ||
A surgical intevention, in which the proximal stomach is wrapped around the distal esophagus to create and antireflux barrier and is used as an alternative treatment for chronic GERD when conservative management has not been successful. It was a very common procedure in 1990's, recently not as common due to poor outcomes and patient dissatisfaction<ref name="NEW" />. Some associated risks are: | |||
* Severe dysphagia | |||
* Inability to belch | |||
* Increased flatulence | |||
* Diarrhoea | |||
* Bloating | |||
* Abdominal pain | |||
* Constipation | |||
{{#ev:youtube|X840-6PyO4c|300}} | |||
--& | <ref>Mayoclinic. Anti-reflux Surgery, Fundoplication-Mayo Clinic . http://www.youtube.com/watch?v=X840-6PyO4c&feature=youtu.be. Accessed on April 20, 2011.</ref> | ||
== Physical Therapy Management == | |||
Patients with GERD occasionally present to the clinic with atypical head and neck symptoms without complaints of heartburn.<ref name="Pathology" /> It is important for the Physical Therapist to be aware of pain referral patterns for the esophagus. With an atypical presentation, the Physical Therapist may need to ask if the patient has a history of difficulty swallowing, difficulty speaking, chronic dry cough, etc. | |||
There are also those patients who attend physiotherapy for other conditions, but have a history of GERD. In this case the Physical Therapist has to be aware of positioning and education on lifestyle modifications if necessary.<ref name="Pathology" /> When treating a patient with GERD<ref name="Pathology" />: | |||
* Assist the patient in implementing changes related to the diet and exercise | |||
* Educate and encourage the patient on lifestyle modifications | |||
* Educate on Positioning: | |||
** Supine interventions should be avoided after meal | |||
** Encourage the patient to sleep on the left side | |||
** Right side lying allows the acid to flow into the esophagus more easily | |||
** Head up positions minimize reflux and reduce intraabdominal pressur | |||
=== The Shaker Head-Lifting Exercise === | |||
& | Research has found that performing the Shaker exercise<ref name="Pathology" />, developed by Dr.Reza Shaker (a gastroenterologist at the Medical College of Wisconsin), can help improve pharyngeal swallowing and dysphagia.<ref>Padwal T, Gurudut P, Hajare S. Effect of shakers exercise with kinesio taping in subjects with gastroesophageal reflux disease: A randomized controlled trial. International Journal of Medical Research & Health Sciences. 2018;5(10):170-8.</ref> It is designed for patients who do not have cervical disc disease, but have dysphagia. The benefits of this technique are: | ||
* Used to strengthen the muscles of the Upper Esophageal Sphincter (UES) | |||
* Used with dysphagia, hiatal hernia, and GERD | |||
* Helps restore normal swallowing | |||
* Helps keep stomach contents from being aspirated into the lungs | |||
==== How to Perform the Technique ==== | |||
The patient should lie in the supine position on firm, flat surface, without a pillow and arms resting by their sides. They should be instructed to breathe slow and steady throughout the exercise. | |||
* Lift Head (to look at the toes) and Hold | |||
** Lift head to look at toes | |||
** Shoulders should be kept flat on the surface it is only the head that lifts up. | |||
** Hold for 1 minute then the head returns to the starting position. | |||
** Repeat 2 more times, relaxing for 1 minute between each repetition. | |||
* Head Lift and Lower | |||
** Lift head up to look toward the chin and then put return to the start position. (It resembles a sit up but with the head). | |||
** Repeat 30 times. | |||
** Relax | |||
== Lifestyle Changes == | |||
Changing eating habits and lifestyle along with avoiding foods that may trigger symptoms can help decrease the symptoms of GERD. <ref name="Pathology" /><ref name="PUB med" /> | |||
Changing eating habits and lifestyle along with avoiding foods that may trigger symptoms can help decrease the symptoms of GERD. | |||
There are several foods and beverages that are linked to causing symptoms of GERD (i.e. heartburn) and linked to making the symptoms worse. Physicians suggest people with GERD should avoid these foods along with other foods or activities that have been linked to causing symptoms in the specific individual. Foods and beverages known to cause an increase in symptoms: | |||
*Alcohol | *Alcohol | ||
*Caffeine | *Caffeine | ||
| Line 334: | Line 199: | ||
*Full-fat dairy products | *Full-fat dairy products | ||
*Peppermint | *Peppermint | ||
*Spearmint | *Spearmint | ||
*Peppermint flavors and tobacco can decrease saliva production. Greater saliva production helps soothe the esophagus by washing the stomach contents back down to the stomach. <ref name="Pathology" /><br> | |||
[[Image:Esophagus4.gif|right|290x250px]]Lifestyle and eating habit changes that can help decrease the onset of heartburn and other GERD symptoms: | |||
*Do not smoke | *Do not smoke | ||
*Do not lie down 2-3 hours after a meal, especially lying flat | *Do not lie down 2-3 hours after a meal, especially lying flat | ||
| Line 349: | Line 212: | ||
*Chewing sugar less gum after meals can help promote saliva production and neutralize acid | *Chewing sugar less gum after meals can help promote saliva production and neutralize acid | ||
*Keep a food diary to record foods that trigger GERD and avoid those foods | *Keep a food diary to record foods that trigger GERD and avoid those foods | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
| Line 359: | Line 220: | ||
*Peptic ulcer disease | *Peptic ulcer disease | ||
*Esophageal motility disorders | *Esophageal motility disorders | ||
*Eosinophilic, infectious, or pill | *Eosinophilic, infectious, or pill esophagitis | ||
== Case Reports/ Case Studies == | == Case Reports/ Case Studies == | ||
* Chronic gastroesophageal reflux disease and its effect on laryngeal visualization and intubation: [http://www.ncbi.nlm.nih.gov/pubmed/12425126 a case report.] <ref name="Case 1">Stevens L. Chronic gastroesophageal reflux disease and its effect on laryngeal visualization and intubation: a case report. AANA Journal [serial on the Internet. (2002, Oct), [cited March 17, 2011]; 70(5): 373-375. Available from: MEDLINE.]</ref> | |||
* A Randomized Study Comparing the Shaker Exercise with Traditional Therapy: [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2895999/?tool=pubmed A Preliminary Study] <ref name="Case 2">Logemann, JA, Rademaker, A, Pauloski, BR, et al. A Randomized Study Comparing the Shaker Exercise with Traditional Therapy: A Preliminary Study. Dysphagia. [serial on the Internet. (2009 December), [cited March 31, 2011]; 24(4): 403–411. Available from: PubMed.]</ref> | |||
* Dental erosion caused by silent [http://www.adajournal.com/cgi/content/abstract/133/6/734 gastroesophageal reflux disease]<ref name="Dental">Dena A. Ali, D.D.S., Ronald S. Brown, D.D.S., M.S., Luciano O. Rodriguez, D.D.S., et al. Dental erosion caused by silent gastroesophageal reflux disease. JADA [serial on the Internet. (2002 June), [cited March 31, 2011]; 133(6): 734–737. Available from: PubMed.]</ref> | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Bellarmine_Student_Project]] | [[Category:Bellarmine_Student_Project]] | ||
Latest revision as of 22:54, 17 November 2019
Top Contributors - Tessa Puckett, Admin, Kim Jackson, 127.0.0.1, Elaine Lonnemann, WikiSysop, Bruce Tan and Wendy Walker
Definition/Description[edit | edit source]
Gastroesophageal reflux disease (GERD), sometimes referred to as esophagitis, is a complex disease with serious complications. It results from reflux (backward flow) of the stomach contents into the esophagus and causes trouble symptoms at least two times a week. Reflux of infectious agents, chemical irritants, physical agents, such as radiation and nasogastric intubation can cause GERD and can irritate and inflame the esophagus causing heartburn, belching, sore throat and other symptoms. [1][2][3][4]
Heartburn is not another word for GERD, but is the most common symptom of the condition.[1] GERD is the most common cause of heartburn, but there are other disorders that contribute to heartburn.[4]
Although GERD is common in our society, it is rarely life-threatening, but can severely limit daily activities and productivity.[5] GERD can occur in infants and children. Infants typically grow out of the disease, and children with GERD present the same as adults.[2]
Prevalence[edit | edit source]
GERD is the most common gastrointestinal diagnosis recorded during visits to outpatient clinics. It is estimated that 14-20% of adults are affected, but the estimates are based on self-reported chronic heartburn. [4] Studies have shown that GERD is clinically silent in 24% of cases in which patients had difficult to control asthma[8]. It can often be seen in:[8]
- Patients with asthma
- Middle aged group (45-54 years old)
- Body Mass Index > 25 with asthma and COPD
Characteristics/Clinical Presentation[edit | edit source]
Pain in the lower substernal area can arise as a result of relfux or GERD; it is commonly described as "heartburn" or "indigestion". GERD is also described as gripping, squeezing or burning sensations in the substernal area.[2][3]
Onset of GERD can occur when lying flat on the back, after meals, or bending forward and is usually worse at night. It is important to note that reflux or GERD is often confused with angina or a heart attack and should be reported to the doctor. GERD is not typically exercise induced and is relieved with antacids; this can help differentiate between angina/heart attack and reflux.
Chest pain referred from the upper gastrointestinal tract can radiate from the chest posteriorly to the upper back or interscapular or subscapular regions from vertebrae T10 - L2.
Common Symptoms:
- Heartburn
- Bitter/sour taste in the back of the throat
- Sense of a lump in the throat
- Abdominal bloating/Abdominal discomfort
- Gas
- Chronic Cough
- Feeling the food is trapped behind the breastbone or in the throat
- Nausea after eating
- Burning sensation that begins at the xiphoid processs and radiates up toward the neck
- Intense sharp pain behind sternum with radiation to the back
Less Common Symptoms:
- Difficulty swallowing (dysphagia)
- Hiccups
- Hoarseness or change in voice
- Sore throat
- Wheezing
- Ear Ache
Associated Co-morbidities[edit | edit source]
Patients with a past medical history of alcoholism, cirrhosis of the liver, peptic ulcers, esophageal varices, esophageal cancer, and long term use of NSAID's are more likely to have symptoms of GERD and should have diagnostic tests performed to rule out more severe conditions or diagnose GERD. It is typical for patients with GERD to have multiple risk factors. Some of the factors that predispose patients to pathologic reflux are: [4][1]
- Lower esophageal Sphincter hypotension
- Loss of esophagel peristaltic function
- Abdominal obesity
- Increased compliance of the hiatal canal
- Gastric hypersecretory states
- Delayed gastric emptying
- Pregnancy
- Scleroderma
- Hiatal hernia [2]
Medications[edit | edit source]
Medications used to treat symptoms of GERD include: Antacids, Histamine 2 Receptor Blockers, and Proton Pump Inhibitors. Indefinite treatment with proton-pump inhibitors or H2-blockers as needed to maintain symptom control[2].There are risks associated with long term use of proton-pump inhibitors.[4]
Antacids[edit | edit source]
- Neutralizes the acid
- Does not reduce it (same amount of acid is produced)
- Available over the counter, do not require a prescription
- Includes Mylanta, Maalox, Tums, Rolaids
Histamine-2 Receptor Blockers[edit | edit source]
- Reduce stomach acid produced by the stomach
- Some are sold over the counter
- Over the Counter H2 Blockers: Pepcid, Zantac, Tagamet, and Axid
Proton Pump Inihibitors[edit | edit source]
- Most potent acid-suppressing agent
- Stops acid from forming, instead of neutralizing it
- Some PPI's are sold over the counter
- Use caution when used without medial supervision
- PPI's can mask more serious conditions in the esophagus and stomach
- Over the counter PPI's: Prilosec (omeprazole) and Zegerid
- PPI's requiring a prescription: Prevacid, Protonix, Nexium (esomperalzole), and Aciphex
People taking the above listed medications should report to the doctor if they have complaints of headache, constipation, diarrhoea, abdominal pain, or dizziness.
It is essential for the physical therapist to take note of the patient's medications; listen for complaints of headache, constipation, diarrhoea, abdominal pain and dizziness; and report those findings to the doctor.
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
Diagnostic tests are not typically needed unless the symptoms are severe. Physicians will order diagnostic tests to diagnose GERD or other complications if there are severe symptoms, the symptoms are not relieved with medications or the symptoms returned. Severe symptoms include dysphagia, odynophagia, bleeding, weight loss, anemia, and those at risk for Barrett's esophagus.[3][4] Commonly used diagnostic tests used to diagnose GERD are discussed below.
Esophagogastroduodenoscopy[edit | edit source]
A procedure where a small camera is placed at the end of flexible tube; the tube is inserted into the mouth and down the throat and examines the lining of the esophagus, stomach and upper duodenum[5][9]
Barium Swallow[edit | edit source]
This is a special type of imaging that requires the patient to drink barium before undergoing an x-ray. This produces clear images of the upper digestive tract.[10]
Continuous Esophageal pH Monitoring[edit | edit source]
This procedure involves a thin tube being inserted into the esophagus, through the mouth, to measure acid levels and the pH[5]
Esophageal Manometry [edit | edit source]
This procedure requires a thin tube to be inserted into the esophagus, through the mouth or nose, to measure the pressure of the esophagus[5]
Etiology/Causes[edit | edit source]
The lower esophageal sphincter (LES) is a ring of muscle fibers that functions to close the opening between the esophagus and the stomach. When the LES is not functioning properly, the stomach contents (food, liquid, and stomach acid) can move backward into the esophagus causing damage to the esophagus. The backward flow of food from the stomach into the esphophagus is called reflux. [3]
- Obesity
- Smoking
- Alcohol
- Medications
- Lower Esophageal Sphincter (LES) Dysfunction
Some of the medications that can cause GERD or make it worse are:[3]
- Nonsteroidal anti-inflammatory drugs (NSAID's) - Advil (ibruprofen), Motrin, Aleve
- Anticholinergics - Bentyl
- Beta Blockers - Toprol XL
- Bronchodilators - Advair
- Calcium Channel Blockers - Norvasc
- Hormone Replacement Therapy - Progesterone
- Sedatives (benzodiazepines) - Valium, Xanax
- Tricyclic Antidepressants: Doxepin
Systemic Involvement[edit | edit source]
Musculoskeletal[edit | edit source]
Untreated ulcers can cause biomechanical changes in muscular contractions and spinal movement. Patient may present with musculoskeletal deficits or dysfunctions because of the untreated ulcer. It is important for the physical therapist to take a good medical history to reveal actual cause of musculoskeletal dysfunction. Patients may think that heartburn while lying flat, difficulty swallowing, or chronic cough is unrelated to their recent onset of midscapular pain or thoracic back pain; thus, it is imperative to ask the patient if they have had any symptoms of GERD and if they are being treated by a medical doctor for the diagnosis.[2]
Dental[edit | edit source]
GERD can cause irreversible dental erosion of the posterior surface of the teeth. Possible symptoms associated with dental erosion included vomiting, experiencing sour taste, belching, heartburn, stomach ache and pain on awakening. Oral Symptoms include: burning mouth syndrome, tooth sensitivity, loss of the vertical dimension of cculsion and aesthetic disfigurement.[11]
Respiratory[edit | edit source]
Gastric acid in the airways can cause bronchoconstriction which increases bronchial activity. Acid in the esophagus releases substance P and neurokinin A in the bronchial mucosa causing a neuroinflammatory reflex mechanism and airway edema. An increase in asthma severity is caused from an increase in vagal efferent impulses and the results of acid being in the esophagus and the airways.[12]
Gastrointestinal[edit | edit source]
GERD is a risk factor for Barrett's esophagus and is linked to esophageal adenocarcinoma. Barrett's esophagus is a precancerous condition, in which the normal squamous epithelium is replaced by specialized metaplastic columnar cell-lined eipthelium.[13] Chronic GERD is a major risk for esophageal adenocarcinoma.[2]
Medical Management[edit | edit source]
If lifestyle changes and medications do not help the symptoms of GERD, the individual may be considered for surgical management.
Nissen Fundoplication[edit | edit source]
A surgical intevention, in which the proximal stomach is wrapped around the distal esophagus to create and antireflux barrier and is used as an alternative treatment for chronic GERD when conservative management has not been successful. It was a very common procedure in 1990's, recently not as common due to poor outcomes and patient dissatisfaction[4]. Some associated risks are:
- Severe dysphagia
- Inability to belch
- Increased flatulence
- Diarrhoea
- Bloating
- Abdominal pain
- Constipation
Physical Therapy Management[edit | edit source]
Patients with GERD occasionally present to the clinic with atypical head and neck symptoms without complaints of heartburn.[1] It is important for the Physical Therapist to be aware of pain referral patterns for the esophagus. With an atypical presentation, the Physical Therapist may need to ask if the patient has a history of difficulty swallowing, difficulty speaking, chronic dry cough, etc.
There are also those patients who attend physiotherapy for other conditions, but have a history of GERD. In this case the Physical Therapist has to be aware of positioning and education on lifestyle modifications if necessary.[1] When treating a patient with GERD[1]:
- Assist the patient in implementing changes related to the diet and exercise
- Educate and encourage the patient on lifestyle modifications
- Educate on Positioning:
- Supine interventions should be avoided after meal
- Encourage the patient to sleep on the left side
- Right side lying allows the acid to flow into the esophagus more easily
- Head up positions minimize reflux and reduce intraabdominal pressur
The Shaker Head-Lifting Exercise[edit | edit source]
Research has found that performing the Shaker exercise[1], developed by Dr.Reza Shaker (a gastroenterologist at the Medical College of Wisconsin), can help improve pharyngeal swallowing and dysphagia.[15] It is designed for patients who do not have cervical disc disease, but have dysphagia. The benefits of this technique are:
- Used to strengthen the muscles of the Upper Esophageal Sphincter (UES)
- Used with dysphagia, hiatal hernia, and GERD
- Helps restore normal swallowing
- Helps keep stomach contents from being aspirated into the lungs
How to Perform the Technique[edit | edit source]
The patient should lie in the supine position on firm, flat surface, without a pillow and arms resting by their sides. They should be instructed to breathe slow and steady throughout the exercise.
- Lift Head (to look at the toes) and Hold
- Lift head to look at toes
- Shoulders should be kept flat on the surface it is only the head that lifts up.
- Hold for 1 minute then the head returns to the starting position.
- Repeat 2 more times, relaxing for 1 minute between each repetition.
- Head Lift and Lower
- Lift head up to look toward the chin and then put return to the start position. (It resembles a sit up but with the head).
- Repeat 30 times.
- Relax
Lifestyle Changes[edit | edit source]
Changing eating habits and lifestyle along with avoiding foods that may trigger symptoms can help decrease the symptoms of GERD. [1][3]
There are several foods and beverages that are linked to causing symptoms of GERD (i.e. heartburn) and linked to making the symptoms worse. Physicians suggest people with GERD should avoid these foods along with other foods or activities that have been linked to causing symptoms in the specific individual. Foods and beverages known to cause an increase in symptoms:
- Alcohol
- Caffeine
- Carbonated beverages
- Chocolate
- Citrus fruits and beverages
- Tomatoes and tomato sauce
- Spicy or fatty foods
- Full-fat dairy products
- Peppermint
- Spearmint
- Peppermint flavors and tobacco can decrease saliva production. Greater saliva production helps soothe the esophagus by washing the stomach contents back down to the stomach. [1]
Lifestyle and eating habit changes that can help decrease the onset of heartburn and other GERD symptoms:
- Do not smoke
- Do not lie down 2-3 hours after a meal, especially lying flat
- Avoid clothes or belts that fit tightly around the bra line or waist
- Avoid bending over or exercising immediately after a meal
- Eat smaller meals
- Reduce stress
- Elevate the head of the bed about 6 inches with a wedge or by tilting the entire bed, do not use extra pillows to raise your head
- Weight loss may help decrease symptoms, if the individual is overweight.
- Chewing sugar less gum after meals can help promote saliva production and neutralize acid
- Keep a food diary to record foods that trigger GERD and avoid those foods
Differential Diagnosis[edit | edit source]
- Coronary artery disease
- Gallbladder disease
- Gastric or esophageal cancer
- Peptic ulcer disease
- Esophageal motility disorders
- Eosinophilic, infectious, or pill esophagitis
Case Reports/ Case Studies[edit | edit source]
- Chronic gastroesophageal reflux disease and its effect on laryngeal visualization and intubation: a case report. [16]
- A Randomized Study Comparing the Shaker Exercise with Traditional Therapy: A Preliminary Study [17]
- Dental erosion caused by silent gastroesophageal reflux disease[11]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Goodman CC, Fuller KS. Pathology: Implications for the Physical Therapist. 3rd ed. St. Louis: Saunders Elsevier; 2009.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Goodman, Snyder. Differential Diagnosis for Physical Therapists: Screening for Referral. 4th Ed. Philadelphia: WB Saunders; 2003.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 National Center for Biotechnology Information, U.S. National Library of Medicine. Gastroesophageal reflux disease. http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001311/ (accessed 17 March 2011).
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 Kahrilas, P.J. Gastroesophageal Reflux Disease. The New England Journal of Medicine.[serial on the Internet. (2006, Oct), [cited April 21, 2011]; 359(16): 1700-1707. Available from: PubMed.]
- ↑ 5.0 5.1 5.2 5.3 Medical College of Wisconsin. Gastroenterology & Hepatology. http://www.mcw.edu/gastrohep.htm (accessed 21 April 2011).
- ↑ HealthGuru. Understanding GERD (GERD #1). http://www.youtube.com/watch?v=o8iShP84HP4&feature=youtu.be. Accessed on April 20, 2011.
- ↑ Mayoclinic. Heartburn, Acid Reflux, GERD-Mayo Clinic. http://www.youtube.com/watch?v=TdK0jRFpWPQ&feature=youtu.be. Accessed on April 20, 2011.
- ↑ 8.0 8.1 Bor S., Kitapciogle G., Solak Z.A., et al. Prevalence of gastroesophageal reflux disease in patients with asthma and chronic obstructive pulmonary disease. JGHF [serial on the Internet. (2009), [cited April 21, 2011]; 25: 309-313. Available from: PubMed.]
- ↑ National Center for Biotechnology Information, U.S. National Library of Medicine. EGD - esophagogastroduodenoscopy. http://www.nlm.nih.gov/medlineplus/ency/article/003888.htm (accessed 19 April 2011).
- ↑ Harvard Health Publications. Harvard Medical School. Barium Swallow (Upper Gastrointestinal Series or "Upper GI Series"). http://www.health.harvard.edu/diagnostic-tests/barium-swallow.htm (accessed 21 April 2011).
- ↑ 11.0 11.1 Dena A. Ali, D.D.S., Ronald S. Brown, D.D.S., M.S., Luciano O. Rodriguez, D.D.S., et al. Dental erosion caused by silent gastroesophageal reflux disease. JADA [serial on the Internet. (2002 June), [cited March 31, 2011]; 133(6): 734–737. Available from: PubMed.]
- ↑ Böcskei C, Viczián M, Böcskei R, Horváth I. The influence of gastroesophageal reflux disease and its treatment on asthmatic cough. Lung. [serial on the Internet. (2005 Jan-Feb), [cited April 21, 2011]; 183(1): 53–62. Available from: PubMed.]
- ↑ Veugelers PJ, Porter GA, Guernsey DL, Casson AG. Obesity and lifestyle risk factors for gastroesophageal reflux disease, Barrett esophagus and esophageal adenocarcinoma.Diseases of the Esophagus.[serial on the Internet. (2006), [cited April 21, 2011]; 19(5): 321–328. Available from: PubMed.]
- ↑ Mayoclinic. Anti-reflux Surgery, Fundoplication-Mayo Clinic . http://www.youtube.com/watch?v=X840-6PyO4c&feature=youtu.be. Accessed on April 20, 2011.
- ↑ Padwal T, Gurudut P, Hajare S. Effect of shakers exercise with kinesio taping in subjects with gastroesophageal reflux disease: A randomized controlled trial. International Journal of Medical Research & Health Sciences. 2018;5(10):170-8.
- ↑ Stevens L. Chronic gastroesophageal reflux disease and its effect on laryngeal visualization and intubation: a case report. AANA Journal [serial on the Internet. (2002, Oct), [cited March 17, 2011]; 70(5): 373-375. Available from: MEDLINE.]
- ↑ Logemann, JA, Rademaker, A, Pauloski, BR, et al. A Randomized Study Comparing the Shaker Exercise with Traditional Therapy: A Preliminary Study. Dysphagia. [serial on the Internet. (2009 December), [cited March 31, 2011]; 24(4): 403–411. Available from: PubMed.]