Theories of Pain
Top Contributors - Venus Pagare, Kim Jackson, Andeela Hafeez, WikiSysop, Jasrah Javed and Admin
Introduction[edit | edit source]
Humans have provided reasons for pain's existence and sought soothing medicines to diminish or stop the unpleasant sensation for as long as they can remember.[1] Physiotherapists are often confronted by patient's experiencing pain and patient's expectations of being cured are very high. A physiotherapist's approach to pain will often depend on their knowledge and their client's perception of pain and it's causes.[2] Several theoretical frameworks have been proposed to explain the physiological basis of pain, although none yet completely accounts for all aspects of pain perception. A number of theories have been postulated to describe mechanisms underlying pain perception. These theories date back several centuries and even millennia (Kenins 1988; Perl 2007; Rey 1995) [3]
Cartesian Dualistic Theory (1596-1650)[edit | edit source]
Pain, according to the dualism idea, is a mutually exclusive reality. Pain can be caused by a physical or psychological harm. The two forms of harm, on the other hand, have no impact on each other, and they were never meant to mix and generate a synergistic effect on pain, making pain a mutually exclusive phenomenon. Descartes added the concept that suffering has a relationship to the soul in his theory in order to appease the church. He said that his studies revealed that the pineal gland is the soul of pain, implying that the brain is the moderator of painful experiences. Many recognized elements that contribute to pain are not taken into consideration by the dualistic approach to pain theory.[4]
Intensive Theory (Erb, 1874)[edit | edit source]
An Intensive (or Summation) Theory of Pain (now referred to as the Intensity Theory) has been postulated at several different times throughout history. First, conceptualized in the fourth century BCE by Plato in his oeuvre Timaeus (Plato 1998), the theory defines pain, not as a unique sensory experience but rather, as an emotion that occurs when a stimulus is stronger than usual[5]. This theory is based on Aristotle’s concept that pain resulted from excessive stimulation of the sense of touch. Both stimulus intensity and central summation are critical determinants of pain. It was implied that the summation occurred in the dorsal horn cells.Arthur Goldscheider further advanced the Intensity Theory, based on an experiment performed by Bernhard Naunyn in 1859 [cited in Dallenbach (1939)].[5] These experiments showed that repeated tactile stimulation (below the threshold for tactile perception) produced pain in patients with syphilis who had degenerating dorsal columns. When this stimulus was presented to patients 60–600 times/s, they rapidly developed what they described as unbearable pain. Naunyn reproduced these results in a series of experiments with different types of stimuli, including electrical stimuli. It was concluded that there must be some form of summation that occurs for the sub-threshold stimuli to become unbearably painful.
Specificity Theory (Von Frey, 1895)[edit | edit source]
Specificity theory is one of the first modern theories for pain. It holds that specific pain receptors transmit signals to a "pain center" in the brain that produces the perception of pain[6]Von Frey (1895) argued that the body has a separate sensory system for perceiving pain—just as it does for hearing and vision. This theory considers pain as an independent sensation with specialized peripheral sensory receptors [nociceptors], which respond to damage and send signals through pathways (along nerve fibers) in the nervous system to target centers in the brain. These brain centers process the signals to produce the experience of pain. Thus, it is based on the assumption that the free nerve endings are pain receptors and that the other three types of receptors are also specific to a sensory experience.
Strong's Theory (Strong, 1895) [edit | edit source]
Strong investigated physical pain, particularly that felt through the skin. He isolated pain from displeasure by focusing on cutaneous pain, where the infliction of pain carried no immediate threat, and therefore the emotional response was removed. He proposed that pain was an experience based on both the noxious stimulus and the psychic reaction or displeasure provoked by the sensation. Strong concluded that pain is the sensation: The first sensation was the experience of heat and then came the sensation of pain. He claimed that in in earlier stages of evolution sensations were merely modifications of the nervous system and it was only after the development of the ego did these sensations become projected emotions known as displeasure.[7]
Pattern Theory[edit | edit source]
In an attempt to overhaul theories of somaesthesis (including pain), J. P. Nafe postulated a “quantitative theory of feeling” (1929). This theory ignored findings of specialized nerve endings and many of the observations supporting the specificity and/or intensive theories of pain. The theory stated that any somaesthetic sensation occurred by a specific and particular pattern of neural firing and that the spatial and temporal profile of firing of the peripheral nerves encoded the stimulus type and intensity[8].Goldschneider (1920) proposed that there is no separate system for perceiving pain, and the receptors for pain are shared with other senses, such as of touch. This theory considers that peripheral sensory receptors, responding to touch, warmth and other non-damaging as well as to damaging stimuli, give rise to non-painful or painful experiences as a result of differences in the patterns [in time] of the signals sent through the nervous system. Thus, according to this view, people feel pain when certain patterns of neural activity occur, such as when appropriate types of activity reach excessively high levels in the brain. These patterns occur only with intense stimulation. Because strong and mild stimuli of the same sense modality produce different patterns of neural activity, being hit hard feels painful, but being caressed does not. It suggested that all cutaneous qualities are produced by spatial and temporal patterns of nerve impulses rather than by separate, modality specific transmission routes.
Central Summation Theory (Livingstone, 1943)[edit | edit source]
It proposed that the intense stimulation resulting from the nerve and tissue damage activates fibers that project to internuncial neuron pools within the spinal cord creating abnormal reverberating circuits with self-activating neurons. Prolonged abnormal activity bombards cells in the spinal cord, and information is projected to the brain for pain perception.
The Fourth Theory of Pain (Hardy, Wolff, and Goodell, 1940s)[edit | edit source]
It stated that pain was composed of two components: the perception of pain and the reaction one has towards it. The reaction was described as a complex biopsychosocial process involving cognition, past experience, culture and various psychological factors which influence pain perception.
Sensory Interaction Theory (Noordenbos, 1959)[edit | edit source]
It describes two systems involving transmission of pain: fast and slow system. The later presumed to conduct somatic and visceral afferents whereas the former was considered to inhibit transmission of the small fibers.
Gate Control Theory (Melzack and Wall, 1965)[edit | edit source]
Melzack has proposed a theory of pain that has stimulated considerable interest and debate and has certainly been a vast improvement on the early theories of pain. According to his theory, pain stimulation is carried by small, slow fibers that enter the dorsal horn of the spinal cord; then other cells transmit the impulses from the spinal cord up to the brain. These fibers are called T-cells. The T-cells can be located in a specific area of the spinal cord, known as the substantial gelatinosa. These fibers can have an impact on the smaller fibers that carry the pain stimulation. In some cases they can inhibit the communication of stimulation, while in other cases they can allow stimulation to be communicated into the central nervous system. For example, large fibers can prohibit the impulses from the small fibers from ever communicating with the brain. In this way, the large fibers create a hypothetical "gate" that can open or close the system to pain stimulation. According to the theory, the gate can sometimes be overwhelmed by a large number of small activated fibers. In other words, the greater the level of pain stimulation, the less adequate the gate in blocking the communication of this information.
There are 3 factors which influence the 'opening and closing' of the gate[9]:
- The amount of activity in the pain fibers. Activity in these fibers tends to open the gate. The stronger the noxious stimulation, the more active the pain fibers.
- The amount of activity in other peripheral fibers—that is, those fibers that carry information about harmless stimuli or mild irritation, such as touching, rubbing, or lightly scratching the skin. These are large-diameter fibers called A-beta fibers. Activity in A-beta fibers tends to close the gate, inhibiting the perception of pain when noxious stimulation exists. This would explain why gently massaging or applying heat to sore muscles decreases the pain.
- Messages that descend from the brain. Neurons in the brainstem and cortex have efferent pathways to the spinal cord, and the impulses they send can open or close the gate. The effects of some brain processes, such as those in anxiety or excitement, probably have a general impact, opening or closing the gate for all inputs from any areas of the body. But the impact of other brain processes may be very specific, applying to only some inputs from certain parts of the body. The idea that brain impulses influence the gating mechanism helps to explain why people who are hypnotized or distracted by competing environmental stimuli may not notice the pain of an injury.
The benefit of this theory is that it provides a physiological basis for the complex phenomenon of pain. It does this by investigating the complex structure of the nervous system, which is comprised of the following two major divisions:[10]
- Central nervous system (the spinal cord and the brain)
- Peripheral nervous system (nerves outside of the brain and spinal cord, including branching nerves in the torso and extremities, as well as nerves in the lumbar spine region)
Neuromatrix Model[edit | edit source]
Ronald Melzack offered another model that contributed to the explanation of how and why humans feel pain over thirty years after establishing the gate control theory of pain. Until the mid-nineteenth century, the majority of pain theories assumed that the sensation was caused solely by a bodily lesion. The theory was that whenever a person was injured, whether from trauma, infection, or disease, a signal would be sent to the brain, which would result in the sense of pain. Melzack had contributed to prior ideas, but it was his encounters with amputees who were feeling phantom limb pain in well-healed places that motivated his investigation into this more realistic pain philosophy. Pain, according to the neuromatrix hypothesis, is a multidimensional sensation caused by characteristic "neurosignature" patterns of nerve impulses created by a widely dispersed neural network in the brain called the "body-self neuromatrix." The central nerve system, rather than the peripheral, is thought to be responsible for triggering painful feelings. According to the neuromatrix concept, there are four components in the central nervous system that cause pain. The "body-self neuromatrix, cyclic processing, and synthesis of signals, sentinel neural hub, and neuromatrix activation". The neuromatrix, according to Melzack, is made up of numerous locations within the central nervous system that contribute to the signal that permits us to sense pain.[11]
Biomedical Model[edit | edit source]
Using a biological model to treat pain suggests that pain has a unique physiological cause, which physicians should be able to identify and treat. The biological approach is, in fact, relevant and important for the management of acute pain. Treatment with competent medical care, such as medication, bracing, physical therapy, and strategies to encourage healing, for example, relieves the pain in a person with a sprained ankle. In this situation, pain is viewed as a symptom of the initial damage, and therapies are aimed at resolving the problem. The biomedical paradigm, on the other hand, is ineffective in the management of chronic pain. Traditional biomedical practice evaluated nociceptive—"sensing harmful stimuli"—elements of pain and used the acute-chronic distinction, which did not always account for emotional aspects of pain.[12]
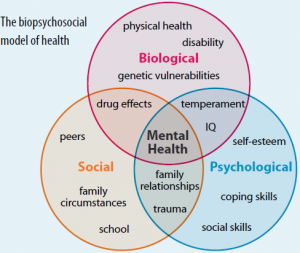
Biopsychosocial Model of Pain[edit | edit source]
The Biopsychosocial Model states that pain is not simply a neurophysiological phenomenon, but also involves social and psychological factors. It says that factors like culture, family, nociceptive stimuli and environment influence pain perception and thus ultimately affect a person’s emotions, behaviors and cognition.
Reference[edit | edit source]
- ↑ Booth, Martin. Opium a history. London: Simon & Schuster, 1996. Print.
- ↑ Barron, C. J., Klaber Moffett, J. A., & Potter, M. (2007). Patient expectations of physiotherapy: Definitions, concepts, and theories. Physiotherapy Theory and Practice, 23(1), 37–46.
- ↑ Moayedi M, Davis KD. Theories of pain: from specificity to gate control. J Neurophysiol 2013; 109:5-12
- ↑ Trachsel LA, Cascella M. Pain theory.
- ↑ 5.0 5.1 Massieh Moayedi, Karen D. Davis Journal of Neurophysiology Published 1 January 2013 Vol. 109 no. 1, 5-12 DOI:
- ↑ Temperature and Pain Theories of Pain Perception
- ↑ Strong, C. A. (1895). The psychology of pain. Psychological Review, 2(4), 329–347
- ↑ http://jn.physiology.org/content/109/1/5
- ↑ http://admedadvice.blogspot.in/2006/09/types-and-theories-of-pain-types-of.html
- ↑ Modern Ideas: The Gate Control Theory of Chronic PainfckLRBy William W. Deardorff, PhD, ABPP
- ↑ Melzack R. Pain and the neuromatrix in the brain. Journal of dental education. 2001 Dec;65(12):1378-82.
- ↑ Bendelow G. Chronic pain patients and the biomedical model of pain. AMA Journal of Ethics. 2013 May 1;15(5):455-9.