The Basics of MRI for Physiotherapy Students
Original Author - User:Dinu Dixon
Top Contributors - Dinu Dixon and Kim Jackson
Introduction[edit | edit source]
Magnetic resonance imaging, or MRI, is a noninvasive medical imaging test that produces detailed images of almost every internal structure in the human body, including the organs, bones, muscles and blood vessels.
Magnetic resonance imaging (MRI) is a type of scan that uses strong magnetic fields and radio waves to produce detailed images of the inside of the body.
unlike X-rays, MRI scanners create images of the body using a large magnet and radio waves. No radiation is produced during an MRI exam. Because ionizing radiation is not used.
The first MRI scanner used to image the human body was built in New York in 1977.
The MRI scanner is essentially a giant magnet. The strength of the magnet is measured in a unit called Tesla (T). Most MRI scanners used in hospitals and medical research clinics are 1.5 or 3 T. Putting that in to perspective, the earth’s magnetic field is around 0.00006T. A 3 T MRI scanner is around 60,000 times stronger than the earth’s magnetic field!
Basic Principles[edit | edit source]
MRI uses magnetic fields and radio waves to measures how much water is in different tissues of the body, maps the location of the water and then uses this information to generate a detailed image. The images are so detailed because our bodies are made up of around 65% water, so we have lots of signal to measure. The water molecule (H2O) is made up of two hydrogen atoms and one oxygen atom. The hydrogen (H) atoms are the part that makes water interesting for MRI, and what we use to measure the signal from the body when we do an MRI scan.
The magnet embedded within the MRI scanner can act on these positively charged hydrogen ions (H+ ions) and cause them to ‘spin’ in an identical manner. By varying the strength and direction of this magnetic field, we can change the direction of ‘spin’ of the protons, enabling us to build layers of detail.
When the magnet is switched off, the protons will gradually return to their original state in a process known as precession. Fundamentally, the different tissue types within the body return at different rates and that allows us to visualise and differentiate between the different tissues of the body.
MRI IMAGING SEQUENCES[edit | edit source]
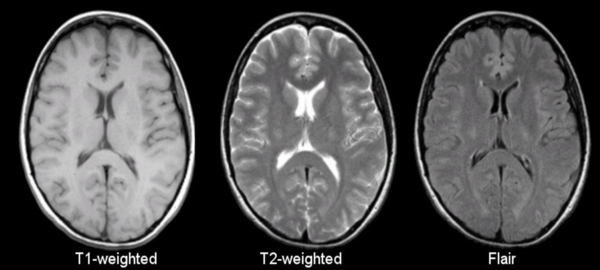
The most common MRI sequences are T1-weighted and T2-weighted scans.
T1-weighted images are produced by using short TE (Time to echo) and TR (Repetition Time). The contrast and brightness of the image are predominately determined by T1 properties of tissue. Conversely, T2-weighted images are produced by using longer TE and TR times. In these images, the contrast and brightness are predominately determined by the T2 properties of tissue.
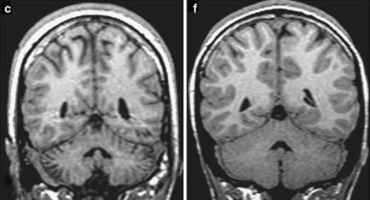
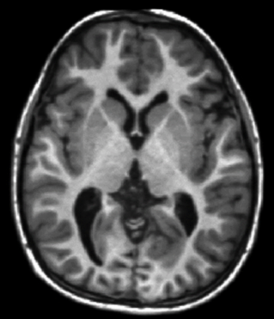
In general, T1- and T2-weighted images can be easily differentiated by looking the CSF. CSF is dark on T1-weighted imaging and bright on T2-weighted imaging.
T1 weighted sequences:[edit | edit source]
T1 weighted (T1W) sequences are part of almost all MRI protocols and are best thought of as the most 'anatomical' of images.
(historically the T1W sequence was known as the anatomical sequence), resulting in images that most closely approximate the appearances of tissues macroscopically, although even this is a gross simplification.
The dominant signal intensities of different tissues are:
- Fluid (e.g. urine, CSF): low signal intensity - Black
- Muscle: intermediate signal intensity - Grey
- Fat : high signal intensity - White
- Brain:
- grey matter: intermediate signal intensity (grey)
- white matter: hyperintense compared to grey matter (white-ish)
1. Contrast enhanced[edit | edit source]
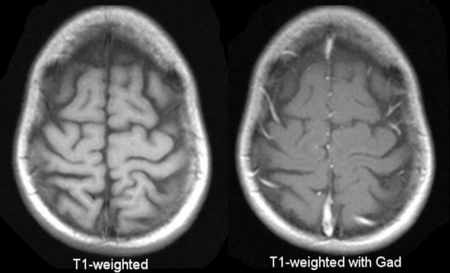
The most commonly used contrast agents in MRI are gadolinium based.
At the concentrations used, these agents have the effect of causing T1 signal to be increased (this is sometimes confusingly referred to as T1 shortening).
The contrast is injected intravenously (typically 5-15 mL) and scans are obtained a few minutes after administration.
Pathological tissues (tumors, areas of inflammation/infection) will demonstrate accumulation of contrast (mostly due to leaky blood vessels) and therefore appear as brighter than surrounding tissue.
2. Fat suppression[edit | edit source]
Fat suppression (or attenuation or saturation) is a tweak performed on many T1 weighted sequences, to suppress the bright signal from fat. This is performed most commonly in two scenarios:
Firstly, and most commonly, after the administration of gadolinium contrast. This has the advantage of making enhancing tissue easier to appreciate.
Secondly, if you think that some particular tissue is fatty and want to prove it, showing that it becomes dark on fat suppressed sequences is handy.
T2 weighted sequences:[edit | edit source]
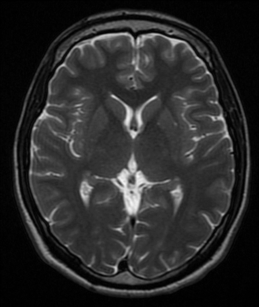
T2 weighted (T2W) sequences are part of almost all MRI protocols.
Without modification the dominant signal intensities of different tissues are:
- Fluid (e.g. urine, CSF): high signal intensity (white)
- Muscle: intermediate signal intensity (grey)
- Fat: high signal intensity (white)
- Brain:
- grey matter: intermediate signal intensity (grey)
- white matter: hypointense compared to grey matter (dark-ish)
1. Fat suppressed[edit | edit source]
In many instances one wants to detect edema in soft tissues which often have significant components of fat.
As such suppressing the signal from fat allows fluid, which is of high signal, to stand out. This can be achieved in a number of ways (e.g. chemical fat saturation or STIR) but the end result is the same.
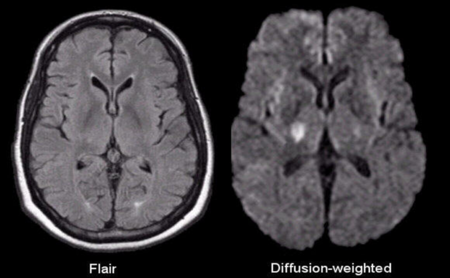
2. Fluid attenuated[edit | edit source]
Similarly in the brain, we often want to detect parenchymal edema without the glaring high signal from CSF. To do this we suppress CSF.
This sequence is called FLAIR. Importantly, at first glance FLAIR images appear similar to T1 (CSF is dark). The best way to tell the two apart is to look at the grey-white matter.
T1 sequences will have grey matter being darker than white matter.
T2 weighted sequences, whether fluid attenuated or not, will have white matter being darker than grey matter.
Diffusion weighted sequences:[edit | edit source]
Diffusion weighted imaging assess the ease with which water molecules move around within a tissue (mostly representing fluid within the extracellular space) and gives insight into cellularity (e.g. tumors), cell swelling (e.g. ischemia) and edema.
1.DWI[edit | edit source]
Acute pathology (ischemic stroke, cellular tumor, pus) usually appears as increased signal denoting restricted diffusion
It is a relatively low resolution image with the following appearance:
- grey matter: intermediate signal intensity (grey)
- white matter: slightly hypointense compared to grey matter
- CSF: low signal (black)
- fat: little signal due to paucity of water
- other soft tissues: intermediate signal intensity (grey)
because there is a component of the image derived from T2 signal, some tissues that are bright on T2 will appear bright on DWI images without there being an abnormal restricted diffusion. This phenomenon is known as T2 shine through.
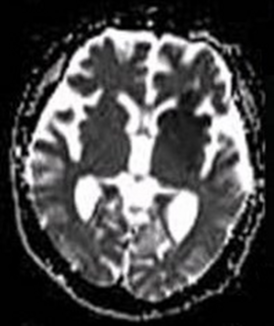
2.ADC[edit | edit source]
Acute pathology (ischemic stroke, cellular tumor, pus) usually appears as decreased signal denoting restricted diffusion.
Apparent diffusion coefficient maps (ADC) are images representing the actual diffusion values of the tissue without T2 effects.
They appear basically as grayscale inverted DWI images.
They are relatively low resolution images with the following appearances:
- grey matter: intermediate signal intensity (grey)
- white matter: slightly hyperintense compared to grey matter
- CSF: high signal (white)
- fat: little signal due to paucity of water
- other soft tissues: intermediate signal intensity (grey)
References[edit | edit source]
- https://case.edu/med/neurology/NR/MRI%20Basics.htm
- https://radiopaedia.org/articles/mri-sequences-overview
- https://www.mayoclinic.org/tests-procedures/mri/about/pac-20384768#:~:text=Magnetic%20resonance%20imaging%20(MRI)%20is,large%2C%20tube%2Dshaped%20magnets.
- https://en.wikipedia.org/wiki/Magnetic_resonance_imaging
- https://www.radiologyinfo.org/en/info/bodymr