Technology Based Gait Rehabilitation in Spinal Cord Injury
Original Editor - Sehriban Ozmen
Top Contributors - Sehriban Ozmen and Ewa Jaraczewska
Introduction[edit | edit source]
Spinal cord injury (SCI) is a neurological condition that affects thousands of people globally every year [1] and causes varying degrees of disability depending on the level of lesion in the spinal cord. One of the main goals in the treatment of individuals with SCI is to restore ambulation. To achieve this, gait rehabilitation is planned by a multidisciplinary team and can be supported by growing technologies. [2] Some of these technologies and their supporting evidence are described below.
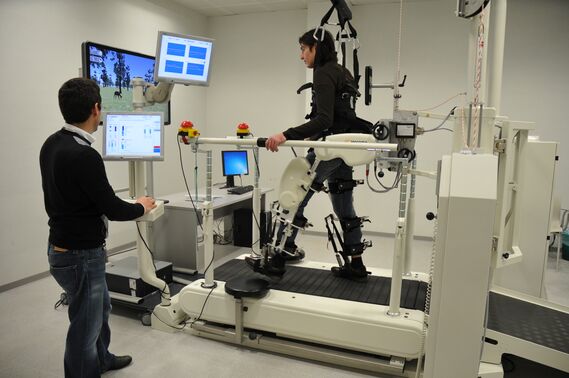
Robotic Assisted Gait Training[edit | edit source]
This novel approach uses robotic devices developed based on the body weight-supported treadmill (BWST) method. Still, unlike BWST, they do not require the physiotherapist to manually support the lower extremity [3]. Some of the advantages of robotic-assisted gait training are listed below:
- Allows a symmetrical and natural walking pattern. [3]
- Allows intensity and duration to increase during training sessions. [3]
- It directs lower extremity movements partially or completely through adaptive controllers, thus allowing the patient to start and eventually finish the movement. [3]
- Helps earlier walking recovery and a better scheme of gait pattern with respect to conventional gait rehabilitation. [4]
- Significantly improves the velocity, distance, and Walking Index Spinal Cord Injury (WISCI) compared to conventional physical therapy in the acute phase. [5]
Robotic Exoskeletons[edit | edit source]
These wearable devices have been developed in the last decade for task-specific, ambulatory overground walking training. [6]
They actuate hip and knee joints and help with movement and mobility. [7]
The research around the use of robotic exoskeletons in SCI has mainly focused on three devices: ReWalk, Ekso and Indego. They all require the patient to support their weight with a walking aid, such as crutches or a walking frame. [7]
Possible improvements are in bladder and bowel function, pain, spasticity, bone density, lean body mass, muscle tone, and improved walking speed within the device. [7]
Functional Electrical Stimulation[edit | edit source]
Functional Electrical Stimulation (FES) is a treatment approach in which electrical stimulation is given via an electrode to stimulate the paralyzed nerve or muscle, but unlike Neuromuscular Electrical Stimulation (NMES), it also involves completing a functional task. Its use in SCI is mainly to restore extremity functions; it has been proven in many studies that it improves upper extremity functions and has also been applied to the lower extremity to improve gait parameters. [8]
According to a systematic review study [5] in which 17 randomised controlled studies were analyzed to compare the interventions used for gait rehabilitation in SCI, the FES method was found to be the most effective method in increasing walking velocity and distance for incomplete SCI, followed by treadmill, FES plus treadmill, robotic-assisted gait training, and conventional physical therapy, respectively.
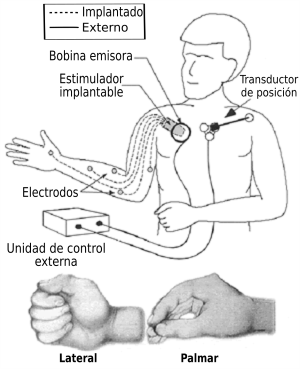
Neuroprosthesis[edit | edit source]
It is a treatment approach in which FES technology is integrated into neuroprostheses. The working mechanism can be explained through its four major parts: the electrical stimulator, electrodes, sensors, and an orthosis. [9]
The electrical stimulator generates electricity to cause muscle contraction, electricity is transmitted to the tissues through transcutaneous or implantable electrodes, sensors provide biofeedback in achieving the targeted movement, and thus simulation parameters can be altered in real-time. The main role of orthoses is to prevent muscle fatigue and help the patient maintain energy by applying structural assistance. [9]
Studies showed that the use of neuroprostheses in people with SCI;
- Allow to produce actions such as grasp, overhead reach, trunk posture, standing, stepping, bladder/bowel/sexual, and respiratory functions. [10]
- Have a significant impact on the health, function, and quality of life. [10]
- When applied continuously to the muscles that provide trunk and hip extension, allow to maintain standing for more than ten minutes. [11]
- Reduce the torque and power output needed to initiate walking movement. [12]
Virtual Reality[edit | edit source]
Virtual Reality (VR) is a technology that provides a life-like experience by creating an interactive three-dimensional environment. The equipment used in VR to enhance the level of reality includes a head-mounted display (HMD), tracking system, sound device, and haptic-feedback gloves or wearable sleeves. VR can be divided into three categories according to the degree of immersion: non-immersive (includes solely monitor, keyboard, and mouse), semi-immersive (uses a larger monitor-to-body ratio to depict a virtual scenario), and immersive (uses an HMD). [13]
A recent systematic review and meta-analysis study [14] concluded that the use of VR therapy in SCI rehabilitation can improve gait as well as standing and sitting balance. However, it also stated the need for more randomized controlled studies to confirm the effects of VR in SCI rehabilitation.
Resources[edit | edit source]
References[edit | edit source]
- ↑ WHO Spinal cord injury. https://www.who.int/news-room/fact-sheets/detail/spinal-cord-injury. Accessed 23 Jul 2021
- ↑ La Rosa G, Avola M, Di Gregorio T, Calabrò RS, Onesta MP. Gait Recovery in Spinal Cord Injury: A Systematic Review with Metanalysis Involving New Rehabilitative Technologies. Brain Sciences. 2023 Apr 22;13(5):703.
- ↑ 3.0 3.1 3.2 3.3 Mikolajczyk T, Ciobanu I, Badea DI, Iliescu A, Pizzamiglio S, Schauer T, Seel T, Seiciu PL, Turner DL, Berteanu M. Advanced technology for gait rehabilitation: An overview. Advances in Mechanical Engineering. 2018 Jul;10(7):1687814018783627.
- ↑ Stampacchia G, Gazzotti V, Olivieri M, Andrenelli E, Bonaiuti D, Calabro RS, Carmignano SM, Cassio A, Fundaro C, Companini I, Mazzoli D. Gait robot-assisted rehabilitation in persons with spinal cord injury: A scoping review. NeuroRehabilitation. 2022 Jan 1(Preprint):1-39.
- ↑ 5.0 5.1 Patathong T, Klaewkasikum K, Woratanarat P, Rattanasiri S, Anothaisintawee T, Woratanarat T, Thakkinstian A. The efficacy of gait rehabilitation for the treatment of incomplete spinal cord injury: a systematic review and network meta-analysis. Journal of Orthopaedic Surgery and Research. 2023 Jan 23;18(1):60.
- ↑ Gil-Agudo Á, Megía-García Á, Pons JL, Sinovas-Alonso I, Comino-Suárez N, Lozano-Berrio V, Del-Ama AJ. Exoskeleton-based training improves walking independence in incomplete spinal cord injury patients: results from a randomized controlled trial. Journal of NeuroEngineering and Rehabilitation. 2023 Dec;20(1):1-1.
- ↑ 7.0 7.1 7.2 Postol N, Spratt NJ, Bivard A, Marquez J. Physiotherapy using a free-standing robotic exoskeleton for patients with spinal cord injury: a feasibility study. Journal of NeuroEngineering and Rehabilitation. 2021 Dec;18(1):1-0.
- ↑ Karamian BA, Siegel N, Nourie B, Serruya MD, Heary RF, Harrop JS, Vaccaro AR. The role of electrical stimulation for rehabilitation and regeneration after spinal cord injury. Journal of Orthopaedics and Traumatology. 2022 Dec;23(1):2.
- ↑ 9.0 9.1 Karamian BA, Siegel N, Nourie B, Serruya MD, Heary RF, Harrop JS, Vaccaro AR. The role of electrical stimulation for rehabilitation and regeneration after spinal cord injury. Journal of Orthopaedics and Traumatology. 2022 Dec;23(1):2.
- ↑ 10.0 10.1 Kilgore KL, Anderson KD, Peckham PH. Neuroprosthesis for individuals with spinal cord injury. Neurological research. 2023 Oct 3;45(10):893-905.
- ↑ Triolo RJ, Bailey SN, Foglyano KM, Kobetic R, Lombardo LM, Miller ME, Pinault G. Long-term performance and user satisfaction with implanted neuroprostheses for upright mobility after paraplegia: 2-to 14-year follow-up. Archives of physical medicine and rehabilitation. 2018 Feb 1;99(2):289-98.
- ↑ Ha KH, Murray SA, Goldfarb M. An approach for the cooperative control of FES with a powered exoskeleton during level walking for persons with paraplegia. IEEE Transactions on Neural Systems and Rehabilitation Engineering. 2015 Apr 23;24(4):455-66.
- ↑ Yeo E, Chau B, Chi B, Ruckle DE, Ta P. Virtual reality neurorehabilitation for mobility in spinal cord injury: A structured review. Innovations in clinical neuroscience. 2019 Jan 1;16(1-2):13.
- ↑ Abou L, Malala VD, Yarnot R, Alluri A, Rice LA. Effects of virtual reality therapy on gait and balance among individuals with spinal cord injury: A systematic review and meta-analysis. Neurorehabilitation and Neural Repair. 2020 May;34(5):375-88.