PAIVMs of the Cervical Spine - Assessment
Background[edit | edit source]
Assessment of passive intervertebral movements form an important part of the physical assessment of people with musculoskeletal spinal conditions and serves to localise and characterise impairments of individual motion segments. Assessment of passive intervertebral movements can be divided into PPIVMs of the Cervical Spine - Assessment (PPIVMs) and Passive Accessory Intervertebral Movements (PAIVMs). Although these terms originated with the Maitland Approach, they can be used to describe assessment techniques used in a variety of approaches.
There is some contention about whether limitations of segmental mobility actually exist and, if they do, whether their assessment is relevant. At least in the cervical spine, specifically targeted treatment produces superior results to general treatment.[1] In order to specifically target one’s treatment, it is necessary to assess individual motion segments.
PPIVMs are defined as passively producing movements in directions that can be performed actively. Like active movements, PPIVMs usually involve rotation around at least one axis.
PAIVMs are defined as producing movements in directions that can not be produced actively in isolation but nonetheless need to be available for active movements to occur. In the periphery, these movements are generally glides produced by a linear force and result in translational rather than rotational movement. In the spine, PAIVMs are produced by applying a translational force, but unlike in the periphery, the movements that are produced are not purely translational.
This article will consider four PAIVM techniques. Different approaches to manual therapy use different terminology and variations of techniques. This article I will use the terminology from the Maitland Approach. The article will primarily discuss and provide a rationale and the evidence for one approach to performing these techniques that has evolved from research as well as clinical and teaching experiences since the author studied, taught and worked with Maitland nearly 40 years ago and is described as Active Manual Therapy. The techniques that will be considered are: Central posterior-anterior movements (PAs), Unilateral posterior-anterior movements (Unilateral PAs) and anterior -posterior movements (APs). Other directions such as transverse or lateral glides can also be performed, but will not be discussed here.
History[edit | edit source]
PAs are the most commonly used PAIVM across all regions of the spine. They were originally thought of as analogous to accessory movements in the periphery. That is the moving vertebrae was thought to translate in the direction of the applied force. A PA movement was originally described[2] as being in a posterior to anterior direction. Later, others suggested PAs should be produced by a force directed along the lines of the facets as shown in the figure below.
The original concepts of PA movements[2]. Left image. PA movements were originally thought to produce a translational movement in a posterior to anterior direction of one vertebrae on another. Right image. Others suggested that the force should be directed along the planes of the facets. The facets in fact separate as in the left image, nor do the discs compress as in the right.
"It is now clear however from both in vivo [3].[4][5][6][7][8] and in vitro [9] [10]studies that the spinal movement produced by PA movements is neither localised, nor primarily accessory. Rather the movement produced spans a number of intervertebral levels, is primarily physiological movement in the sagittal plane, and is potentially influenced by a number of non-articular factors. [11][12][13][14]" Quote from Tuttle and Hazle (2018) [15]
In spite of PAs producing regional movement, segmental movement can be perceivable in an individual motion segment due to two factors ([15]. First that the moment or torque is produced preferentially under the applied force and secondly, the intervertebral stiffness is non-linear - there is a low resistance neutral or lax zone followed by an increase in resistance (often referred to as starting at R1) and endfeel.
Our modelling indicates that the amount of PA force to reach the end of the neutral zone (R1) at the targeted level is less than 10 Newtons (about the force needed to click a pen) while after 25 Newtons (about the force needed to push the plunger of a hand sanitiser[16]) almost all of the remaining displacement is accounted for by levels above or below the target location. Both forces are much lower than the forces usually applied in clinical practice. For example, the force used in grade II treatment techniques in the cervical spine which are defined as occurring short of R1 is about 40 Newtons. [17] Similarly most physiotherapists applied considerably more than 50 newtons when assessing PAs of the cervical spine.[18]
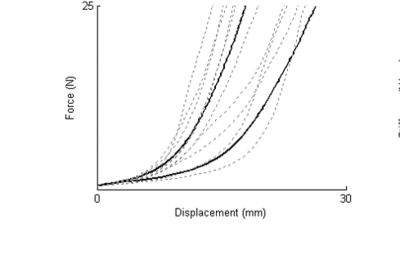
Humans can discriminate differences in stiffness of 5%, [19] to 10%.[20] at the levels of force used to assess PA movements. The differences in stiffness between symptomatic and asymptomatic locations in the cervical spine at forces below 10 Newtons should be easily perceivable since the differences can be up to 100% while at forces approaching 25 Newtons the differences can be much smaller and therefore harder to perceive[15].
Mean force/displacement curves of unilateral PAs to the cervical spine comparing tender (left solid line) and less tender (right solid line) sides. Dashed lines indicate individual curves. The greatest differences occur below about 10 newtons. Above 15 Newtons the curves are nearly parallel. From Tuttle, N., Barrett, R., & Laakso, L. (2009). [21]
Reliability[edit | edit source]
Studies suggest that the reliability of motion palpation is limited, but there are two main difficulties with these studies. First, the quality of these studies has been less than adequate. [22] Interestingly the studies with lower risk of bias tended to find better reliability. The reliability of PAIVMs as provocation tests has sometimes been considered to be superior to PAIVMs as mobility tests, however the differences between the reliability of using mobility and provocation are quite small.[23]
Secondly, the studies had participants classify whether each location in isolation was limited or not. Clinicians, however, do not consider what they feel in one location in isolation, but compare side to side as well as above and below because humans are much better at comparisons than classifications. Two studies that have not yet been published assessed the reliability of comparisons. In one a therapist assessed unilateral PAs on 20 patients after taking a history and performing a PAIVM assessment where they included questions about symptoms. A second blinded therapist was then asked to compare the selected location with another arbitrarily selected location only assessing mobility without any information on pain. They agreed on 18 out of 20 patients or 90% of the time. In the other, pre-clinical student physiotherapy students comparing the mobility of three thoracic vertebrae on PA movements demonstrated a 68% agreement without any information about pain provocation.
In summary, although the evidence for the reliability of motion palpation is inconclusive, as will be seen below, the measurable differences in mobility are easily large enough to be perceptible.
This article will advocate a hybrid approach where a very gentle ‘first pass’ assessing mobility is used to screen to determine which levels might be relevant. Ideally this first pass should produce minimal if any symptoms. The therapist then explores the relevant levels in more detail to localise the source/s of the patient’s symptoms and determine the characteristics of the movement at the symptomatic location.
Techniques[edit | edit source]
PAIVMs in the cervical spine are sometimes performed quite strongly and conceived as simply pushing on a vertebra with the thumbs as shown in the video below. This approach may be useful if the techniques are perceived as being predominantly provocation tests.
If, as the authors would suggest, a therapist is interested in segmental mobility, then it would seem reasonable to perform the techniques in such a way to maximize their ability to perceive the mobility in a way that is as comfortable as possible.
We will discuss three aspects of the techniques before putting it all together
Reduce force[edit | edit source]
Starting with low force is one of the most challenging aspects of these techniques. Most students and therapists, when they can’t feel something, press harder. It is important for students and therapists to develop the ability to perform these techniques with low force early in their career because the changing the amount of force applied is one of the most difficult things for experienced therapists to unlearn.
Use the whole hands to control the movement.[edit | edit source]
Using the whole hands to produce the movement is not a new concept. Jull described using a ‘lumbrical grip’ (Jull, G. (2011). Towards preventing thumb pain from application of cervical manual therapy: A point of view. Man Ther, 16(3), 207-208. doi:10.1016/j.math.2011.02.004) to reduce the incidence of therapist thumb pain and increase patient comfort. From personal observation this is also what Maitland did in practice, although it was not necessarily communicated to those who studies with him. We advocate taking this somewhat further. Rather than using the IP joints of the fingers on the side of the transverse process, if the therapist adopts soft hands (this seems to be the most difficult for students), they can 'hold' slightly anterior to the transverse process with the pads of their fingers. This enables them to gently hold the vertebra with their index (or middle) fingers and thumbs to control the movement of the vertebra including lifting slightly in an anterior direction as well as moving with the whole hands in a posterior direction.
The images below show how using the whole hands effect the movement of the vertebra while doing unilateral PAs. The setup had the ultrasound transducer on the side of the vertebra being moved. The ultrasound video on the left shows how, when just the thumbs are used to produce the movement, that there is more lateral than PA movement. Also note the amount of soft tissue deformation which could increase the likelihood of treatment soreness. The right side shows how, when the whole hand is used to support the vertebra, that the movement is now more vertical and the soft tissue deformation is reduced.
Displace soft tissue[edit | edit source]
Displace the soft tissue to enable a more direct contact with the vertebra. This augments the therapist’s ability to feel the movement with less force and thereby increase patient comfort. The video below used a similar setup to the previous video but with the ultrasound transducer replacing the thumbs and being used to produce the unilateral PA movement. The left side shows the amount of soft tissue deformation that occurs when the force is applied through the soft tissue while on the right is when the soft tissue is displaced prior to doing the movement. Note how when the soft tissue is displaced that the movement of the 'thumbs' more closely mirrors the movement of the vertebra.
A video of putting a PAIVM assessment together is shown below. Note that this also includes Anterior-Posterior (APs). APs are the ‘go to’ technique for many experienced clinicians because of their effectiveness and the ease of both communicating with the patient and modifying their position during the techniques. APs are avoided by other therapists because they are more difficult to do effectively and unless they are done gently and sensitively, they can be quite uncomfortable for the patient.
The approach is described more completely elsewhere[24]. Basically it starts with a very gentle (~ 10 Newtons) first pass across all levels feeling primarily for the location of R1. Ideally this can be performed without patient discomfort and without questioning about of symptoms. The location of R1 indicated the size of the neutral or lax zone. In other words it indicates whether there is a limitation of the amount of available movement. This first pass narrows the likely symptomatic locations down to 3 or 4 locations (including side, level and technique) so that only these need to be assessed more fully. The therapist then explores these locations more completely to determine production or reproduction of symptoms, and the behaviour of pain and stiffness. Maitland describes the importance of finding comparable (or concordant) signs at an appropriate location. A comparable sign is a level of dysfunction that is consistent with the patients symptoms. For example, a pain-free stiffness on PAIVMs would not be comparable if the patient has severe or irritable symptoms; nor would a highly sensitive response to PAIVMs be comparable if the patient has limited active movement with minimal pain.
Once a location is selected as being relevant to the patient's symptoms, a movement diagram can be used to communicate the clinician's findings and inform the grade and parameters of a treatment technique. Alternatively a simplified classification can be used indicating the predominance of pain or stiffness. More advanced clinicians will also explore variations in direction such as angling medial/lateral or superior/inferior.
Clinical implications[edit | edit source]
As mentioned above, at least in the cervical spine the effectiveness of treatment has been found to be improved when it is specifically targeted. Some schools of thought suggest that the selection of treatment techniques are determined by the limitations of active movement or the shape of articular structures. For example, if one was going to use unilateral PAs for a patient with C4-5 symptoms and limited active right rotation that treatment would be either unilateral PAs to right C5 or left C4 because those are the directions limitations would be expected in the facets. Whether fortunately or unfortunately, limitations of passive movements do not necessarily predict the direction or extent of active movements. Therefore we propose an empirical[24] rather than a theoretical approach where limitations of segmental passive movements, rather than the limitations of active movements be used to inform treatment selection. In other words treatment, although informed by pathology and clinical pattern, is generally directed towards the limitations in segmental movement that are actually found rather than what they might be expected to be because of the limitations in AROM or the concave-convex rule. According to the concepts of Active Manual Therapy the selected technique is only a first approximation which undergoes continual modification in real time to maximize changes in the targeted segmental impairment.
- ↑ Slaven, E. J., Goode, A. P., Coronado, R. A., Poole, C., & Hegedus, E. J. (2013). The relative effectiveness of segment specific level and non-specific level spinal joint mobilization on pain and range of motion: results of a systematic review and meta-analysis. Journal of Manual & Manipulative Therapy, 21(1), 7-17.
- ↑ 2.0 2.1 Grieve, G. P. (1981). Common vertebral joint problems. Melbourne: Churchill Livingstone.
- ↑ Caling B, Lee M. Effect of direction of applied mobilization force on the posteroanterior response in the lumbar spine. Journal of Manipulative and Physiological Therapeutics. 2001;24(2):71-8
- ↑ Kulig K, Landel R, Powers CM. Assessment of lumbar spine kinematics using dynamic MRI: a proposed mechanism of sagittal plane motion induced by manual posterior-to-anterior mobilization. J Orthop Sports Phys Ther. 2004;34(2):57-64.
- ↑ Lee R, Evans J. An in vivo study of the intervertebral movements produced by posteroanterior mobilization. Clin Biomech. 1997;12(6):400-8.
- ↑ Lee RY, McGregor AH, Bull AM, Wragg P. Dynamic response of the cervical spine to posteroanterior mobilisation. Clin Biomech. 2005;20(2):228-31.
- ↑ McGregor AH, Wragg P, Gedroyc WM. Can interventional MRI provide an insight into the mechanics of a posterior-anterior mobilisation? Clin Biomech. 2001;16(10):926-9.
- ↑ Powers CM, Kulig K, Harrison J, Bergman G. Segmental mobility of the lumbar spine during a posterior to anterior mobilization: assessment using dynamic MRI. Clin Biomech. 2003;18(1):80-3.
- ↑ Gay RE, Ilharreborde B, Zhao K, Zhao C, An KN. Sagittal plane motion in the human lumbar spine: Comparison of the in vitro quasistatic neutral zone and dynamic motion parameters. Clin Biomech. 2006;21(9):914-9.
- ↑ Sran MM, Khan KM, Zhu Q, Oxland TR. Posteroanterior stiffness predicts sagittal plane midthoracic range of motion and three-dimensional flexibility in cadaveric spine segments. Clin Biomech. 2005;20(8):806-12.
- ↑ Caling B, Lee M. Effect of direction of applied mobilization force on the posteroanterior response in the lumbar spine. Journal of Manipulative and Physiological Therapeutics. 2001;24(2):71-8
- ↑ Chansirinukor W, Lee M, Latimer J. Contribution of ribcage movement to thoracolumbar posteroanterior stiffness. Journal of Manipulative and Physiological Therapeutics. 2003;26(3):176-83.
- ↑ Kawchuk GN, Fauvel OR. Sources of variation in spinal indentation testing: indentation site relocation, intraabdominal pressure, subject movement, muscular response, and stiffness estimation. Journal of Manipulative and Physiological Therapeutics. 2001;24(2):84-91.
- ↑ Lee R, Evans J. An in vivo study of the intervertebral movements produced by posteroanterior mobilization. Clin Biomech. 1997;12(6):400-8.
- ↑ 15.0 15.1 15.2 Tuttle, N., & Hazle, C. (2018). Spinal PA movements behave ‘as if’ there are limitations of local segmental mobility and are large enough to be perceivable by manual palpation: A synthesis of the literature. Musculoskeletal Science and Practice, 36, 25-31.
- ↑ ADA requirements for soap dispensers (cavalierva.com
- ↑ Snodgrass, S. J., Rivett, D. A., Robertson, V. J., & Stojanovski, E. (2010). J Orthop Sports Phys Ther, 40(7), 392-401. doi:2437 [pii] 10.2519/jospt.2010.3274
- ↑ Tuttle, N., & Hazle, C. (2010). Use of simulation tools for assessment and skill development during a two-day post-graduate course on manual therapy. Paper presented at the SimTecTHealth 2010: Education and Innovation in Healthcare, Melbourne
- ↑ Guarri, N., Okamura, A. M., & Kuchenbecker, K. J. (2017). Perception of force and stiffness in the presence of low-frequency haptic noise. PloS one, 12(6), e0178605
- ↑ Nicholson, L. L., Maher, C., & Adams, R. (1998). Hand contact area, force applied and early non-linear stiffness (toe) in a manual stiffness discrimination task. Manual Therapy, 3(4), 212-219
- ↑ Tuttle, N., Barrett, R., & Laakso, L. (2009). Posteroanterior movements in tender and less tender locations of the cervical spine. Manual Therapy, 14(1), 28-35. doi:10.1016/j.math.2007.09.003
- ↑ Jonsson, A., & Rasmussen-Barr, E. (2017). Intra-and inter-rater reliability of movement and palpation tests in patients with neck pain: A systematic review. Physiotherapy theory and practice, 1-16.
- ↑ Hollerwoger, D. (2006). Methodological quality and outcomes of studies addressing manual cervical spine examinations: a review. Manual Therapy, 11(2), 93-98. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=16483829
- ↑ 24.0 24.1 Tuttle, N., & Hazle, C. (2021). An empirical, pragmatic approach applying reflection in interaction approach to manual therapy treatments. Physiotherapy theory and practice, 37(7), 775-786. Briefly, the approach starts with a very gentle (~10 Newtons) first pass which enables the therapist to screen for levels where R1