Medial Meniscus
Original Editor - Aarti Sareen
Top Contributors - Aarti Sareen, Maram Salem, Kim Jackson, Admin, WikiSysop, Rachael Lowe, Evan Thomas, Oyemi Sillo, Fasuba Ayobami and Jonathan Wong
Introduction[edit | edit source]
The menisci are fibrocartilaginous structures that function to deepen the tibial plateau, improve articulation of the femur on the tibia, stabilize the knee, and assist with shock absorption.[1] The medial meniscus specifically forms almost a semicircular shape and covers 50-60% of the articular surface between the medial femoral condyle and the medial tibial plateau.[2] It has a vascular supply and receives innervation from the posterior tibial, obturator, and femoral nerves.[3] The medial meniscus is located on the medial portion of the tibial plateau.
Anatomy and Attachment[edit | edit source]
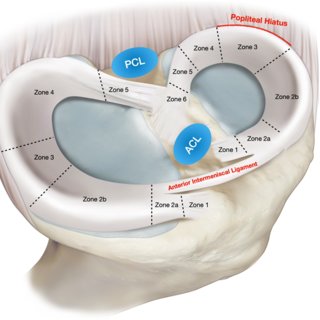
The medial meniscus is approximately 1.4 in (3.5cm) in length. It maintains the same thickness from posterior to anterior.[1] The medial meniscus can be divided into five anteroposterior zones. Zone 1 refers to the anterior root attachment. Zones 2a and 2b refer to the anteromedial zone between the posterior border of the anterior root and the anterior border of the superficial medial collateral ligament. Zone 3 refers to the portion of the medial meniscus that is next to the medial collateral ligament. Zone 4 refers to the posterior horn, and zone 5 refers to the posterior root.[1]
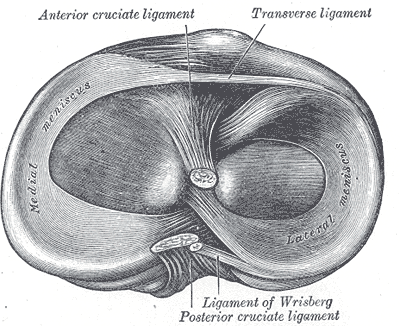
The medial meniscus is attached to the tibial plateau via its anterior horn and posterior horn. The anterior horn of the medial meniscus is attached to the anterior surface of the tibia at the tibial plateau. The anterior horn merges with the fibers of the transverse ligament and the ACL ligament on the tibia.[3] The posterior horn of the medial meniscus is firmly attached to the posterior aspect of the joint capsule. Medially, the medial meniscus is attached to the medial collateral ligament, limiting its mobility. The medial meniscus has no direct attachment to any muscle, but indirect capsule connections to the semimembranosus may provide some retraction of the posterior horn. [3]
Compared to the lateral meniscus, the medial meniscus is a definitive crescent "C" shape, has less variability with size and thickness, and covers a smaller part of the tibial plateau.[3] Anteriorly, it is attached to lateral meniscus by transverse ligament and patella directly or by anterior capsular thickenings called patellomeniscal ligaments [5].
Vascular Supply[edit | edit source]
The vascular supply of the menisci originates predominately from the medial, lateral, and middle genicular arteries. These three arteries are branches of the popliteal artery. The primary areas of vascularity are the superior and inferior portions of the meniscus, making only 10-30% of the meniscus a recipient of direct blood supply. The remaining portion of the medial meniscus is replenished with nutrients via diffusion of the synovial fluid.[6] Due to the lack of direct blood supply to most of the structure, the medial meniscus has difficulty healing after an injury or during the post-operative process.
Nerve Supply[edit | edit source]
The medial meniscus is innervated by branches of the posterior tibial nerve and the terminal branches of the obturator and femoral nerves. The nerve fibers joint together and innervate the joint capsule.[3] The anterior and posterior horns of the medial meniscus innervated with free nerve endings (nociceptors) and three different mechanoreceptors (Ruffini corpuscles, Pacinian corpuscles, and Golgi tendon organs).[7][8][9] These different mechanoreceptors help the knee joint support and adapt to various movements.
Injury/Tear[edit | edit source]
Meniscal injuries can occur in both the younger and older patient population. Injuries in the younger population occur as a result of an acute traumatic injury. The common complaint among patients is an immediate, sharp pain at the medial knee after a "pop" sensation. The most common mechanism of meniscal injury with this population is a twisting injury with the foot anchored on the ground, which can happen either through play during sport or through a direct collision with another person. Damage to the meniscus is due to rotational forces directed at a flexed knee[10][11]. Injuries in the older population are due to degenerative changes over time.
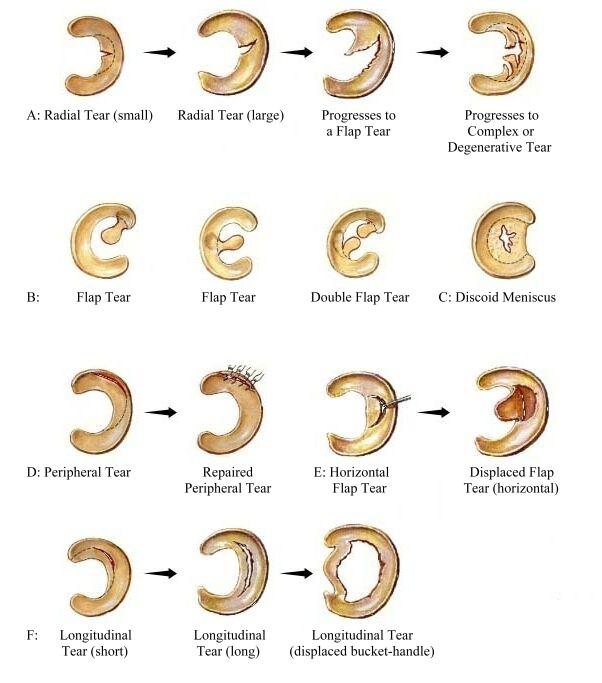
The types of meniscal tears are listed below:
- Longitudinal
- Radial
- Bucket handle
- Flap
- Horizontal cleavage
- Degenerative
Medical meniscus tears can occur as a result of a lateral blow to the knee. Patients commonly present with complaints of medial knee pain along the joint line, medial swelling, and locking of the knee (cannot fully extend the knee). Swelling can range from near instant for larger tears, to swelling that progresses gradually over 24 hours for smaller tears. Concomitant MCL and ACL injuries often occur alongside injuries to the medial meniscus (i.e., the "unhappy triad") due to the meniscus' proximity to these ligaments. Generally, meniscal root tears are less common than meniscal body tears.
The diagnosis of an medial meniscus injury is considered to be fairly certain if three or more of the following findings are present:[10]
- Tenderness at one point over the medial joint line
- Pain in the area of the medial joint line during hyperextension of the knee joint
- Pain in the area of the medial joint line during hyperflexion of the knee joint
- Pain during external rotation of the foot and the lower leg when the knee is flexed at different angles around 70–90°
- Weakened or atrophied quadriceps muscle
A diagnosis can be made on the basis of special tests (listed below), x-rays, or an MRI.
Special Tests[edit | edit source]
The most commonly used special tests are
- McMurray's Test (non-weight bearing)
- Apley’s Test (non-weight bearing)
- Thessaly Test (weight-bearing)
For diagnosis, palpation is also used where the knee is placed in a flexed position to expose the medial and lateral tibiofemoral joint lines. Tenderness over the medial or lateral joint lines can suggest medial or lateral meniscal tears respectively, with this finding being more diagnostically accurate for lateral meniscal tears[12].
Resources[edit | edit source]
Clinical Practice Guideline: Meniscal and Articular Cartilage Lesions
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Mameri ES, Dasari SP, Fortier LM, Verdejo FG, Gursoy S, Yanke AB, Chahla J. Review of meniscus anatomy and biomechanics. Current Reviews in Musculoskeletal Medicine. 2022 Oct;15(5):323-35.
- ↑ Śmigielski R, Becker R, Zdanowicz U, Ciszek B. Medial meniscus anatomy—from basic science to treatment. Knee Surgery, Sports Traumatology, Arthroscopy. 2015 Jan;23:8-14.
- ↑ 3.0 3.1 3.2 3.3 3.4 Farrell C, Shamrock AG, Black AC, Kiel J. Anatomy, Bony Pelvis and Lower Limb: Medial Meniscus. InStatPearls [Internet] 2023 Apr 4. StatPearls Publishing.
- ↑ Review of Meniscus Anatomy and Biomechanics - Scientific Figure on ResearchGate. Available from: https://www.researchgate.net/figure/Medial-and-lateral-meniscus-zones-and-relevant-anatomical-relations-ACL-anterior_fig1_362618200 [accessed 20 Jan, 2024]
- ↑ Tuxoe JI, Teir M, Winge S, et al.: The medial patellofemoral ligament: A dissection study. Knee Surg Sports Traumatol Arthrosc 10:138–140, 2002.
- ↑ McCarty EC, Marx RG, DeHaven KE: Meniscus repair: Considerations in treatment and update of clinical results. Clin Orthop 402:122–134, 2002.
- ↑ Gray JC: Neural and vascular anatomy of the menisci of the human knee. J Orthop Sports Phys Ther 29:23–30, 1999.
- ↑ Zimny ML, Albright DJ, Dabezies E: Mechanoreceptors in the human medial meniscus. Acta Anat (Basel) 133:35–40, 1988.
- ↑ Mine T, Kimura M, Sakka A, et al.: Innervation of nociceptors in the menisci of the knee joint: An immunohistochemical study. Arch Orthop Trauma Surg 120:201–204, 2000.
- ↑ 10.0 10.1 Peterson,Renström. SPORTS INJURIES:Their Prevention and Treatment.Third Edition.
- ↑ Brunker,Khan.Clinical Sports Medicine.3rd Edition.
- ↑ Eren OT. The accuracy of joint line tenderness by physical examination in the diagnosis of meniscal tears. Arthroscopy. 2003 Oct;19(8):850-4. doi: 10.1016/s0749-8063(03)00736-9. PMID: 14551547.