Bladder Considerations with Spinal Cord Injury
Original Editor - Wendy Oelofse
Top Contributors - Ewa Jaraczewska and Jess Bell
Introduction[edit | edit source]
The bladder becomes neurogenic when it no longer receives an input from the brain to empty or store urine. This interruption in communication can occur after a spinal cord injury (SCI) as the brain is not able to send or receive signals to and from the organs below the level of injury. Urologic complications following spinal cord injury can be severe and life-threatening, so developing an optimal bladder management programme for each individual is essential. This article supplies additional information on managing bladder dysfunction after spinal cord injury for the Plus course: Bladder and Bowel Considerations with Spinal Cord Injury.
Bladder Dysfunction in Spinal Cord Injury[edit | edit source]
The location of the spinal cord lesion defines bladder dysfunction.
Spastic Bladder[edit | edit source]
- Observed in people with a spinal cord injury above T12 (upper motor neuron SCI)
- Limited/no ability to feel bladder fullness
- Limited/no control of the sphincter muscle to hold urine
- Spastic/overactive bladder causing involuntary reflex voiding and incontinence – the voiding reflex is intact between the spinal cord and bladder
- Detrusor sphincter dyssynergia (DSD) may also be present
- in DSD, the bladder contracts to void, but the sphincter remains tight
- this causes increased pressure in the bladder, which can result in urine being forced back up the ureters to the kidney, which, in turn, can result in kidney damage
- May experience incomplete bladder emptying
Flaccid Bladder[edit | edit source]
- Observed in people with a spinal cord injury below T12 (lower motor neuron SCI)
- Limited/no ability to feel bladder fullness
- The bladder muscle cannot contract to empty the bladder, which causes overfilling of the bladder (urinary retention)
- The voiding reflex is not intact between the bladder and spinal cord
- The sphincter muscle can also be relaxed, causing urine to leak out of the bladder when it overfills or during activities such as transfers, sneezing, coughing, etc.
- Unable to empty bladder voluntarily
Table 1 summarises storage and voiding dysfunction based on the level of the spinal cord lesion.
| Level of spinal cord lesion | Bladder dysfunction |
|---|---|
| Suprasacral (upper motor neuron injury) |
|
| Mix (upper and lower motor neuron injury) |
|
| Sacral (lower motor neuron injury) |
|
Management of Bladder Dysfunction[edit | edit source]
Spastic Bladder Management[edit | edit source]
Goals:[2]
- To reduce overactivity in the bladder wall muscle, which causes accidents, leaking, and wetness
- To prevent high detrusor pressure and damage to the upper urinary tract
Draining the Bladder[edit | edit source]
The following methods can be used to drain the bladder.[3][2]
- Indwelling catheters:[3]
- an indwelling urethral catheter is not recommended unless a patient has difficulty self-catheterising. Example: patient with quadriplegia or in the presence of urethral abnormalities
- regular follow-up with imaging and cystoscopy is required due to an increased risk of urinary tract infection, renal impairment, bladder stone formation, urethral stricture, urethral erosion, and bladder cancer
- a suprapubic catheter is easier to manage and is an option for patients with quadriplegia
- Condom catheters
- used to catch leaks, but not for emptying the bladder
- Intermittent catheterisation
- Clean Intermittent Catheterisation (CIC)
- Sterile Intermittent Catheterisation (much higher cost)
- CIC is "the preferred form of management of the bladder when adequate low intravesical pressure and acceptable bladder capacity are achievable."[4] However, Wu et al.[4] note that over 45% of patients who initially rely on CIC switch to urethral or suprapubic catheters after 11 years of follow-up based on their preference and physician recommendation.[4]
Intermittent catheterisation (CIC)[edit | edit source]
Females: It can be difficult for female patients to find the right hole (meatus) when they are learning to perform CIC. The meatus is located just below the clitoris and above the vagina. A magnified mirror may help patients see the area. If the catheter is mistakenly inserted into the vagina, it should be left there as a landmark when the new catheter is being inserted. A clean catheter should be inserted ABOVE the vagina into the meatus.
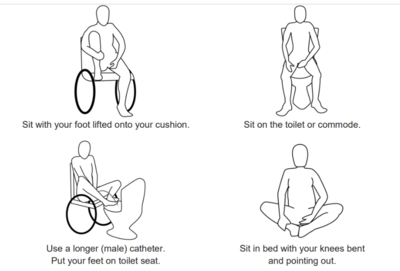
Recommended positions for self-catheterisation for females are shown in Figure 1.
Please watch this video if you want to learn more about self-catheterisation for women with spinal cord injuries. This video shows self-catheterisation performed in bed.
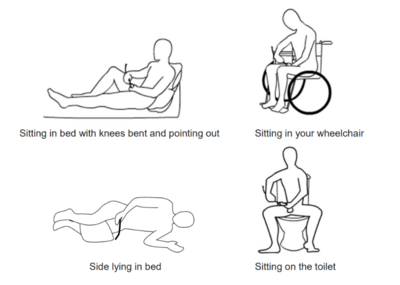
Males: Inserting the catheter can be done in different positions, including sitting in bed, side lying in bed, sitting in the wheelchair or on the toilet.
Recommended positions for self-catheterisation for males are shown in Figure 2.
Please watch the following video if you would like to learn about intermittent catheterisation for males with spinal cord injuries.
Medications[edit | edit source]
- Anticholinergic medications (sometimes called antimuscarinic medications) may help relax the bladder muscles[2]
- This can help to reduce pressure within the bladder, increase the ability of the bladder to hold urine, reduce incontinence and improve compliance and quality of life[3][2]
- Side effects depend on the choice of medication, but may include memory / cognitive impairment, visual blurring, oral dryness, constipation, tachycardias and arrhythmias[3]
Botulin Injections[edit | edit source]
- Injecting small doses of some strains of botulinum toxin (Botox) can help to reduce muscle spasms
- Injections into the bladder wall muscle or the external sphincter muscle can help relax these muscles - this can help prevent leaking and incontinence and may improve bladder emptying
- The effects of these injections can last for 6 to 12 months
Surgical Management[edit | edit source]
- Bladder augmentation surgery can increase the capacity of the bladder to hold urine[3]
- Types of augmentation surgery include:
- augmentation cystoplasty with a detubularised intestinal segment
- augmentation cystoplasty with an ileal segment
- augmentation cystoplasty with a colonic patch
- Incompetent sphincters can be treated with an artificial urinary sphincter (AUS), abdominal slings, or a transobturator tape procedure[3]
Flaccid Bladder Management[edit | edit source]
Goals:[2]
- To prevent overfilling and increased pressure in the bladder
- To prevent leaking and wetness
Draining the Bladder[edit | edit source]
- Intermittent catheterisation or indwelling catheters
- Condom catheters or pouches may be used to catch leaks, but not for emptying
Please see Spastic Bladder Management for more information.
Medication[edit | edit source]
- Alpha-adrenergic blockers are used to encourage the bladder sphincter muscles to relax to allow urine to flow out of the body
- This can help with bladder emptying and help prevent urinary retention
Botulin Injections[edit | edit source]
See Spastic Bladder Management for more information.
Surgical Management[edit | edit source]
- Transurethral sphincterotomy[7]
- Stents:
Bladder Irrigation[edit | edit source]
Bladder irrigation is a procedure that flushes the bladder using sterile liquid. Water, saline, acetic acid, or chlorhexidine can be used for this procedure. Please watch this video if you would like to understand more about bladder irrigation:
Complications of Bladder Dysfunction[edit | edit source]
The most common primary complications include urinary tract infection (UTI), urinary stones, and renal impairment:
- urinary tract infection is an infection of part of the urinary tract (kidneys, bladder or the connecting tubes
- bladder or kidney stones can cause reoccurring UTIs[9]
- renal impairment can be caused by reflux and high pressure in the bladder
Other primary complications include:
- incontinence
- bladder cancer[10]
Secondary complications include:
- skin irritation and skin breakdown due to wetness from bladder complications
- increased spasticity
- autonomic dysreflexia, which is characterised by a sudden rise in blood pressure in response to an irritating stimulus below the level of injury. It typically occurs in people with an injury at T6 and above
Resources[edit | edit source]
- Perez NE, Godbole NP, Amin K, Syan R, Gater DR Jr. Neurogenic Bladder Physiology, Pathogenesis, and Management after Spinal Cord Injury. J Pers Med. 2022 Jun 14;12(6):968.
- Chen YC, Ou YC, Hu JC, Yang MH, Lin WY, Huang SW, Lin WY, Lin CC, Lin VC, Chuang YC, Kuo HC; Taiwan Continence Society Spinal Cord Injury Study Group. Bladder Management Strategies for Urological Complications in Patients with Chronic Spinal Cord Injury. J Clin Med. 2022 Nov 20;11(22):6850.
- UHN Toronto Rehabilitation Institute. Spinal Cord Essentials. Handouts.
- University of Michigan Health. Decision Aid: Bladder Management After Spinal Cord Injury (SCI).
- Spinal Cord Injury Research Evidence (SCIRE). Bladder management following spinal cord injury.
- Vancouver Coastal Health. Bladder management after a spinal cord injury infographic.
- Consortium for Spinal Cord Medicine and Paralyzed Veterans of America. Bladder management following spinal cord injury: what you should know. A guide for people with spinal cord injury.
- SCIRE Community. Bladder changes after spinal cord injury.
- SCIRE Community. Urinary catheters.
- SCIRE Community. Urinary tract infections.
References[edit | edit source]
- ↑ Perez NE, Godbole NP, Amin K, Syan R, Gater DR Jr. Neurogenic Bladder Physiology, Pathogenesis, and Management after Spinal Cord Injury. J Pers Med. 2022 Jun 14;12(6):968.
- ↑ 2.0 2.1 2.2 2.3 2.4 Oelofse W. Bladder and Bowel Dysfunction in Spinal Cord Injury Course. Plus, 2024.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Taweel WA, Seyam R. Neurogenic bladder in spinal cord injury patients. Res Rep Urol. 2015 Jun 10;7:85-99.
- ↑ 4.0 4.1 4.2 Wu SY, Jhang JF, Liu HH, Chen JT, Li JR, Chiu B, Chen SL, Kuo HC. Long-Term Surveillance and Management of Urological Complications in Chronic Spinal Cord-Injured Patients. J Clin Med. 2022 Dec 9;11(24):7307.
- ↑ CortreeTV. Self-catheterisation demo in bed | Spinal cord injury neurogenic bladder. Available from: https://www.youtube.com/watch?v=kxybiDtc-u0 [last accessed 19/01/2024]
- ↑ Craig Hospital. Bladder Management Tools for Men with Spinal Cord Injuries. Available from: https://www.youtube.com/watch?v=KxgjU41JVV8 [last accessed 19/01/2024]
- ↑ 7.0 7.1 7.2 7.3 Sphincterotomy, Artificial Sphincters, Stents and Related Approaches for Bladder Emptying. Available from https://scireproject.com/evidence/bladder-management/therapeutic-interventions-for-detrusor-overactivity-with-dsd-in-sci/enhancing-bladder-emptying-non-pharmacologically/sphincterotomy-artificial-sphincters-stents-and-related-approaches-for-bladder-emptying/ [last access 19.01.2024]
- ↑ Craig Hospital. Bladder Irrigation Procedure. Available from: https://www.youtube.com/watch?v=13eHF0BqBmY [last accessed 19/01/2024]
- ↑ Park YI, Linsenmeyer TA. A method to minimize indwelling catheter calcification and bladder stones in individuals with spinal cord injury. J Spinal Cord Med. 2001 Summer;24(2):105-8.
- ↑ Hess MJ, Zhan EH, Foo DK, Yalla SV. Bladder cancer in patients with spinal cord injury. J Spinal Cord Med. 2003;26(4):335–338.