Wrist Sprain: Difference between revisions
No edit summary |
(Updated examination section) |
||
| (33 intermediate revisions by 8 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor '''- | '''Original Editor ''' - [[User:Rachael Lowe|Rachael Lowe]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Definition/Description == | |||
A '''wrist sprain''' is an injury to the ligaments of the wrist region, including the ligaments connecting the carpal bones and the ligaments connecting the proximal row of carpal bones with the radius and the ulna. By injury we mean that the [https://physio-pedia.com/Ligament_Sprain?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal#share ligaments are partially or completely torn].<ref name=":0">Morgan WJ, Slowman LS. Acute hand and wrist injuries in athletes: Evaluation and management. Journal of the American Academy of Orthopaedic surgeons, nov.-dec. 2001, vol. 9, n°: 6, 389-400. Evidence level: 2A</ref><ref name=":1">Roald Bahr, Sverre Maehlum. Clinical Guide To Sports Injuries. 2004.</ref> | |||
There are three grades:<ref name=":0" /><br>1. A mild overstretching of the ligaments, without joint instability.<br>2. A partial rupture of the ligaments, with no or mild joint instability.<br>3. A complete rupture of a ligament with severe joint instability. | |||
== Clinically Relevant Anatomy == | |||
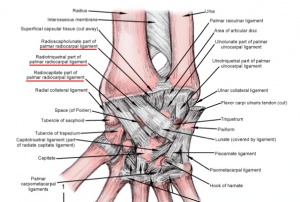
[[Image:Volar wrist ligament.jpg|thumb|right|Representation of the various ligaments susceptible to sprain at the wrist joint.]] | [[Image:Volar wrist ligament.jpg|thumb|right|Representation of the various ligaments susceptible to sprain at the wrist joint.]] | ||
There are two types of wrist sprains, namely radial and ulnar wrist sprain. | There are two types of wrist sprains, namely '''[https://physio-pedia.com/Radius?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal#share radial] and [https://physio-pedia.com/Ulna?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal#share ulnar] wrist sprain.''' | ||
* The '''radial wrist sprain''' is most common, with mostly an injury of the [https://physio-pedia.com/Wrist_and_Hand#share ligaments connecting the lunate with the scaphoid, including the scapholunate ligament and the radioscapholunate ligament.]<ref>Rettig, A. Elbow, forearm and wrist injuries in athlete. Sports Med, 25(2):115-130, 1998. Evidence level: 2C</ref> | |||
In case of an ulnar wrist sprain, it can be a torn of the ligaments of the triangular fibrocartilagenous complex or the luno-triquetrum complex. | * In case of an '''ulnar wrist sprain''', it can be a torn of the [https://physio-pedia.com/Wrist_and_Hand#share ligaments of the triangular fibrocartilagenous complex or the luno-triquetrum complex.]<ref name=":2">Prof. Dr. R. Meeusen. Praktijkgids pols- en handletsels. Vrije Universiteit Brussel. Dienst uitgaven, 2006.</ref> | ||
== Epidemiology/ | == Epidemiology/Etiology == | ||
The most common mechanism of injury is a fall on an outstretched arm/hand, with an important impact on the thenar eminence, combined with a dorsiflexion, an ulnar deviation and intercarpal supination-stress. The gravity and the pattern of the injury are depending on the angle, power and the length of the impact during the fall.<ref name=":2" /><ref name=":1" /> | |||
The most common | The most common type of wrist sprain involves injury to the scapholunte ligament after a hyperextension event and can lead to carpal instability<ref name=":10">May Jr DD, Varacallo M. [https://www.ncbi.nlm.nih.gov/books/NBK551514/ Wrist Sprain.] 2021 Jul 18. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan–.</ref>. | ||
= | Wrist sprains involving injury to the TFCC can be due to axial load or distraction of the forearm or a result of repetitive motions<ref name=":10" />. | ||
== Differential Diagnosis == | |||
< | When a patient has functional disorders and pain after an acute wrist trauma, we want to know whether there is a fracture or not. In most cases, they will take an X-ray to set up a diagnosis. At this moment a group of scientists is trying to set up the ‘Amsterdam Wrist Rules’, like we already know the ‘[[Ottawa Ankle Rules|Ottawa ankle rules]]’. The purpose of their study is to set up guidelines that should be followed in making a decision whether you should take an X-ray of the wrist or not.<ref>Bentohami, et al. Amsterdam wrist rules: A clinical decision aid. BMC Musculoskeletal Disorders. 17 october 2011. Evidence level: 1B Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3229467/?tool=pubmed</ref> | ||
== | Ulnar sided pain for patients with wrist sprains may have injured their TFCC<ref name=":10" />.Replication of pain with palpation of the [[Fovea Sign|ulnar fovea]] may indicate this region was involved in the injury<ref name=":10" />. | ||
We will start the examination with the anamnesis. During this questionnaire we want to learn more about the origin of the injury and we can already ask if there are (according to the patient) any functional disorders. Let the patient describe the symptoms, the most frequent complaint is ‘pain’, let the patient define this pain. It will also be important to ask about the expectations of the therapy. And you can gather information about previous injuries and any possible factors that can hamper the healing | Dorsal-radial pain with an inability to weight bear through an extended wrist (such as a push up) may indicate involvement of the scapholunate ligament<ref name=":10" />. Pain to palpation over the dorsal-radial wrist, [[scaphoid shift test]], and plain radiographs can indicate injury to this region<ref name=":10" />. | ||
== Examination == | |||
* We will start the [https://physio-pedia.com/Wrist_and_Hand_Examination?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal#share examination] with the anamnesis. During this questionnaire, we want to learn more about the origin of the injury and we can already ask if there are (according to the patient) any functional disorders. Let the patient describe the symptoms, the most frequent complaint is ‘pain’, let the patient define this pain. It will also be important to ask about the expectations of the therapy. And you can gather information about previous injuries and any possible factors that can hamper the healing proces <ref name=":7">Christian Dumontier. Physical Examination of wrist instabilities. [INTERNET] Evidence level: 5 | |||
< | http://www.maitrise-orthop.com/corpusmaitri/orthopaedic/dumontier_synth/dumontier_us.shtml | ||
</ref><ref name=":8">Peter Vaes, Eric Kerckhofs, David Beckwée. Het Gezondheidsprofiel. Standaard uitgeverij.</ref><ref name=":5">Honing, E. Wrist injuries – pinpointing pathology in a complex joint. Phys sportsmed, 26(9): 41-49, 1998a. Evidence level: 5</ref> | |||
* After the anamnesis, you should do an inspection of the injured wrist, by comparing it to the other wrist. A sprained wrist can be swollen, red, tender and warm to touch.<ref name=":0" /><ref name=":7" /><ref name=":8" /><ref name=":5" /> | |||
* When you have finished the inspection, you can palpate the wrist with all their structures. Most of the structures in the wrist are very good palpable, but swelling can hinder your palpation and the palpation can be painful for the patient.<ref name=":2" /><ref name=":6">Prosser R, Harvey L, Lastayo P, Hargreaves I, Scougall P, Herbert RD. Provocative wrist tests and MRI are of limited diagnostic value for suspected wrist ligament injuries: a cross-sectional study. Australian Physiotherapy Association. Evidence level: 1B</ref> | |||
* After palpation, you should test each articulation in search of pain, abnormal motion or crepitus. The physiological movement of the wrist can be examined by simple tests of the [https://physio-pedia.com/Goniometry:_Wrist_Flexion?utm_source=physiopedia&utm_medium=related_articles&utm_campaign=ongoing_internal#share palmar flexion], [https://physio-pedia.com/Goniometry:_Wrist_Extension?utm_source=physiopedia&utm_medium=related_articles&utm_campaign=ongoing_internal#share dorsiflexion], [https://physio-pedia.com/Goniometry:_Wrist_Radial_Deviation?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal#share radial deviation] and [https://physio-pedia.com/Goniometry:_Wrist_Ulnar_Deviation?utm_source=physiopedia&utm_medium=related_articles&utm_campaign=ongoing_internal#share ulnar deviation].<ref name=":5" /> | |||
* You should also test the functional movement by letting the patient do things like catching, pinching, holding and managing simple objects.<ref name=":5" /> | |||
* When there is a severe swelling, you can expect that even the smallest mobilizations will be very painful for the patient.<ref name=":7" /><ref name=":5" /> | |||
<br> | * you can do a resistance examination, to examine whether the muscle strength is still normal. You should do this for flexion (Fig.5), extension and ulnar and radial deviation.<ref name=":5" /><br>Beware this can be very painful or even impossible for patients with a severe wrist sprain when the passive mobilizations are already painful and not fully practicable. | ||
* The results of your tests and thus the functional disorders will depend on the severity of the injury.<ref name=":2" /><ref name=":7" /><ref name=":5" /> | |||
You can also run some more specific provocative wrist tests.<ref name=":2" /><ref name=":7" /><ref name=":6" /> | |||
*[https://physio-pedia.com/Scaphoid_shift_test?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal#share Scaphoid Watson shift test] | |||
*Lunotriquetral-ballotement-test | |||
*Finger extensions against resistance | |||
*Midcarpal test | |||
*Distal radioulnar joint test | |||
*Triangular fibrocartilage complex stress test | |||
*Triangular fibrocartilage complex stress test with compression | |||
*Gripping rotatory impaction test | |||
These tests will give you more information about which ligaments are (partially) ruptured and instability of the wrist.<ref name=":2" /> | |||
Prosser et al<ref name=":6" />compared provocative wrist testing and MRI diagnostics to arthroscopic findings to assess their diagnostic value in 105 patients. The scaphoid shift test, midcarpal test, and DRUJ test had mild diagnostic usefulness. MRI was considered moderately useful for TFCC injury diagnostics and mildly useful for scapholunate ligament injury diagnostics<ref name=":6" />. | |||
== Physical Therapy Management == | |||
Mild wrist sprains should follow the RICE method (discussed below) and may feel better in 24-48 hours<ref name=":10" />. | |||
Moderate to severe wrist sprains may need bracing to promote protection and healing of the area before, or while, progressing through the phases discussed below<ref name=":10" />. | |||
==='''Phase 1'''=== | |||
==== At first, you should follow the '''[https://physio-pedia.com/RICE?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal#share RICE] method:'''==== | |||
# '''Rest''': Stop the activity and use of the injured wrist for 48 hours or until the pain and the swelling has subsided.<ref name=":0" /> | |||
# '''Ice:''' Apply a cold pack (wrapped in a towel) or a bag of crushed ice to the sprained wrist, for about 15 minutes, several a day for several days. Don’t ice it for more than 20 minutes at a time! <ref name=":0" /> | |||
#* [https://physio-pedia.com/Cryotherapy?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal#share Cryotherapy] will create a superficial vasoconstriction, so that the local blood flow and haemorrhage decrease.<ref name=":2" />There is some discussion about the effectiveness of cryotherapy, most studies approve the fact that cryotherapy has a pain-decreasing effect. There are also indications that cryotherapy would influence the inflammation, but more and bigger studies are required to prove evidence.<ref name=":2" /><ref>Tricia J. Hubbard; Craig R. Denegar. Does Cryotherapy Improve Outcomes With Soft Tissue Injury? Pennsylvania State University, University Park, PA. Journal of Athletic Training. Volume 39. Number 3. September 2004. Evidence level: 1A. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC522152/?tool=pubmed </ref> | |||
# '''Compression:''' Wrap the wrist with an elastic compression bandage and limit swelling. The bandage should push the edema fluid away from the injured tissue. Start wrapping at the base of the fingers and stop just below the elbow, so that you wrap in the direction of the heart. The wrap should be snug, but be careful not cutting off circulation.<ref name=":0" /><ref name=":9">Wolfe MW, Uhl TL, Mattacola CG, McCluskey LC. Management of ankle sprains. Erratum in Am Fam Physician 2001 Aug1;64(3):386. Evidence level: 2C</ref> | |||
# '''Elevate:''' Try to keep the wrist above heart level as often as possible, during two days. This will help drain fluid and reduce swelling around the wrist. [https://physio-pedia.com/NSAID_Gastropathy?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal#share Nonsteroidal anti-inflammatory drugs (NSAID)] are also recommended.<ref name=":0" /><ref name=":9" /> | |||
In case of a severe wrist sprain it can be recommended to immobilize the wrist. In some rare cases a surgery may be needed to repair a ligament that was torn completely.<ref name=":2" /> | |||
==='''Phase 2'''=== | |||
===='''In a second phase the patient should do gradual retraining exercises, including'''==== | |||
# Active [https://physio-pedia.com/Wrist_and_Hand_Mobilisations?utm_source=physiopedia&utm_medium=related_articles&utm_campaign=ongoing_internal#categories mobilizations], to increase flexibility and range of motion, | |||
# Exercises for the strengthening of the injured wrist. | |||
#* We have to start these exercises early in the rehabilitation, to prevent stiffness and weakness from developing and to ensure the wrist is functioning correctly. You can start exercising as soon as pain allows. It is very important that the patient is guided by the treating physiotherapist during the exercises.<ref>Levine W. Rehabilitation techniques for ligament injuries of the wrist. Hand Clin 8(4):669-681, 1992. Evidence level: 5</ref> | |||
===='''We prefer active mobilizations above the passive ones, but in some cases we can do passive mobilizations to treat hypomobility, by adding traction.<ref name=":2" />'''==== | |||
# First you can perform radiocarpal and midcarpal traction, to see whether this movement provokes pain. This handling can be used to treat hypomobility in different directions.<ref name=":2" /><ref name=":3">Wadsworth C. The wrist and hand. In: Malone T., McPoil T., Nitz A.. Orthopedic and sports physical therapy. Mosby, St. Louis, USA.pp. 327-378,1997</ref> | |||
#* To stimulate flexion you should do the dorsal sliding technique. During this technique the convex carpal bones will move in dorsal direction over the concave surface of the distal radius. <ref name=":2" /><ref name=":3" /> | |||
#* To stimulate extension you have to do the volar sliding technique. This will cause a sliding of the convex carpal bones in the volar direction over the concave surface of the radius. <ref name=":2" /><ref name=":3" /> | |||
#* The ulnar sliding technique will stimulate radial deviation.<ref name=":2" /><ref name=":3" /> | |||
#* The radial sliding technique will stimulate ulnar deviation.<ref name=":2" /><ref name=":3" /> | |||
===='''After these passive mobilizations you can go to the active mobilizations.'''<ref name=":2" />==== | |||
* There are many exercises you can give to your patients, here are some examples.<ref name=":2" /><ref name=":3" /> | |||
*# Turning the wrists: hook your fingers into each other and turn the wrist in different directions. | |||
*# Place your forearms on a table and perform extension (arm in pronation on table) and flexion (arm in supination on table). | |||
*# Do the same for ulnar and radial deviation, you can do this one in pro- and in supination. | |||
== | ===='''You can combine mobilizations with some stretching exercises for the extensors and flexors.<ref name=":2" />'''<ref name=":3" /><ref name=":4">Humphrey D. Flexibility for the wrist, fingers and thumbs. Phys Sportsmed, 18(12):147-148, 1990. Evidence level: 5</ref>==== | ||
* Before you start to stretch, you should perform an isometric contraction and hold this for 5 seconds.<ref name=":2" /><ref name=":3" /><ref name=":4" /> | |||
===='''After mobilizations you can start exercises to improve muscle strength.'''==== | |||
* These exercises will be very similar to the mobilizations, except from the fact that you should use some tools. By tools we mean weights, Theraband, pull machine and many others. The goal of these tools is to put a resistance on the movement. You should start with a low resistance/weight and many repetitions to train the muscle endurance first, then gradually increase resistance/weight but decrease repetitions to train muscle strength, do this depending on the possibilities of the patient.<ref name=":2" /><ref name=":3" /> | |||
* It can also be useful to do some [https://physio-pedia.com/Proprioception?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal#share proprioceptive] exercises, especially for practicing sports, like gymnastics, where the athletes frequently us the hands as weight carriers. These exercises are often performed in push-up position. You will gradually change the surface under the hands starting with flat ground, followed by, normal pillow, Airex pad, Sissel pillow and wobble board.<ref name=":2" /><ref name=":3" /> | |||
It is difficult to give information about the repetitions and the duration of the exercises, because this is strongly related to the patient and his advancement. It is also important to know what the final goal of the patient will be, does he just have to return to [https://physio-pedia.com/ADLs?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal#share ADL-activities] or is he an athlete who has to return to his sport and on which level? You will have to consider all these things when you set up a personal training program for a specific patient.<ref name=":2" /><ref name=":3" /> | |||
When returning to sports activities, the therapist can prepare the patient by taping the wrist or adjust a brace.<ref name=":0" /><ref name=":2" /><br> | |||
When returning to | |||
{{#ev:youtube|0AMIVnkcR0U|300}}<ref>Mathew Hawkes. Hawkes Physiotherapy Wrist sprain video. Available from: https://youtu.be/0AMIVnkcR0U [Accessed 2 Apr 2015]</ref> | {{#ev:youtube|0AMIVnkcR0U|300}}<ref>Mathew Hawkes. Hawkes Physiotherapy Wrist sprain video. Available from: https://youtu.be/0AMIVnkcR0U [Accessed 2 Apr 2015]</ref> | ||
== | == Surgical Intervention == | ||
Surgery may be indicated if patient struggles to improve with conservative management or if there is a full ligament tear. Surgical interventions may include surgical fixation, arthroscopic debridement, or open debridement<ref name=":10" />. | |||
= | |||
== References == | == References == | ||
# Morgan WJ, Slowman LS. Acute hand and wrist injuries in athletes: Evaluation and management. Journal of the American Academy of Orthopaedic surgeons, nov.-dec. 2001, vol. 9, n°: 6, 389-400. Evidence level: 2A | |||
# Prof. Dr. R. Meeusen. Praktijkgids pols- en handletsels. Vrije Universiteit Brussel. Dienst uitgaven, 2006. | |||
# Tricia J. Hubbard; Craig R. Denegar. Does Cryotherapy Improve Outcomes With Soft Tissue Injury? Pennsylvania State University, University Park, PA. Journal of Athletic Training. Volume 39. Number 3. September 2004. Evidence level: 1A. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC522152/?tool=pubmed | |||
# Roald Bahr, Sverre Maehlum. Clinical Guide To Sports Injuries. 2004. | |||
# Christian Dumontier. Physical Examination of wrist instabilities. [INTERNET] Evidence level: 5 http://www.maitrise-orthop.com/corpusmaitri/orthopaedic/dumontier_synth/dumontier_us.shtml | |||
# Bentohami, et al. Amsterdam wrist rules: A clinical decision aid. BMC Musculoskeletal Disorders. 17 october 2011. Evidence level: 1B Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3229467/?tool=pubmed | |||
# Wolfe MW, Uhl TL, Mattacola CG, McCluskey LC. Management of ankle sprains. Erratum in Am Fam Physician 2001 Aug1;64(3):386. Evidence level: 2C | |||
# Peter Vaes, Eric Kerckhofs, David Beckwée. Het Gezondheidsprofiel. Standaard uitgeverij. | |||
# Honing, E. Wrist injuries – pinpointing pathology in a complex joint. Phys sportsmed, 26(9): 41-49, 1998a. Evidence level: 5 | |||
# Prosser R, Harvey L, Lastayo P, Hargreaves I, Scougall P, Herbert RD. Provocative wrist tests and MRI are of limited diagnostic value for suspected wrist ligament injuries: a cross-sectional study. Australian Physiotherapy Association. Evidence level: 1B | |||
# Rettig, A. Elbow, forearm and wrist injuries in athlete. Sports Med, 25(2):115-130, 1998. Evidence level: 2C | |||
# Levine W. Rehabilitation techniques for ligament injuries of the wrist. Hand Clin 8(4):669-681, 1992. Evidence level: 5 | |||
# Wadsworth C. The wrist and hand. In: Malone T., McPoil T., Nitz A.. Orthopedic and sports physical therapy. Mosby, St. Louis, USA.pp. 327-378,1997 | |||
# Humphrey D. Flexibility for the wrist, fingers and thumbs. Phys Sportsmed, 18(12):147-148, 1990. Evidence level: 5 | |||
<references /> | <references /> | ||
[[Category:Sports_Injuries]] | |||
[[Category:Wrist]] | |||
[[Category:Wrist - Conditions]] | |||
[[Category: | [[Category:Conditions]] | ||
[[Category:Wrist - Conditions]] | |||
[[Category:Musculoskeletal/Orthopaedics]] | |||
[[Category:Primary Contact]] | |||
[[Category:Sports Medicine]] | |||
Latest revision as of 19:54, 27 December 2021
Original Editor - Rachael Lowe
Top Contributors - Anas Mohamed, Admin, Patti Cavaleri, Rachael Lowe, Kim Jackson, Richard Benes, Evan Thomas, Eva Huysmans, Naomi O'Reilly, WikiSysop, Claire Knott, Wanda van Niekerk and Amanda Ager
Definition/Description[edit | edit source]
A wrist sprain is an injury to the ligaments of the wrist region, including the ligaments connecting the carpal bones and the ligaments connecting the proximal row of carpal bones with the radius and the ulna. By injury we mean that the ligaments are partially or completely torn.[1][2]
There are three grades:[1]
1. A mild overstretching of the ligaments, without joint instability.
2. A partial rupture of the ligaments, with no or mild joint instability.
3. A complete rupture of a ligament with severe joint instability.
Clinically Relevant Anatomy[edit | edit source]
There are two types of wrist sprains, namely radial and ulnar wrist sprain.
- The radial wrist sprain is most common, with mostly an injury of the ligaments connecting the lunate with the scaphoid, including the scapholunate ligament and the radioscapholunate ligament.[3]
- In case of an ulnar wrist sprain, it can be a torn of the ligaments of the triangular fibrocartilagenous complex or the luno-triquetrum complex.[4]
Epidemiology/Etiology[edit | edit source]
The most common mechanism of injury is a fall on an outstretched arm/hand, with an important impact on the thenar eminence, combined with a dorsiflexion, an ulnar deviation and intercarpal supination-stress. The gravity and the pattern of the injury are depending on the angle, power and the length of the impact during the fall.[4][2]
The most common type of wrist sprain involves injury to the scapholunte ligament after a hyperextension event and can lead to carpal instability[5].
Wrist sprains involving injury to the TFCC can be due to axial load or distraction of the forearm or a result of repetitive motions[5].
Differential Diagnosis[edit | edit source]
When a patient has functional disorders and pain after an acute wrist trauma, we want to know whether there is a fracture or not. In most cases, they will take an X-ray to set up a diagnosis. At this moment a group of scientists is trying to set up the ‘Amsterdam Wrist Rules’, like we already know the ‘Ottawa ankle rules’. The purpose of their study is to set up guidelines that should be followed in making a decision whether you should take an X-ray of the wrist or not.[6]
Ulnar sided pain for patients with wrist sprains may have injured their TFCC[5].Replication of pain with palpation of the ulnar fovea may indicate this region was involved in the injury[5].
Dorsal-radial pain with an inability to weight bear through an extended wrist (such as a push up) may indicate involvement of the scapholunate ligament[5]. Pain to palpation over the dorsal-radial wrist, scaphoid shift test, and plain radiographs can indicate injury to this region[5].
Examination[edit | edit source]
- We will start the examination with the anamnesis. During this questionnaire, we want to learn more about the origin of the injury and we can already ask if there are (according to the patient) any functional disorders. Let the patient describe the symptoms, the most frequent complaint is ‘pain’, let the patient define this pain. It will also be important to ask about the expectations of the therapy. And you can gather information about previous injuries and any possible factors that can hamper the healing proces [7][8][9]
- After the anamnesis, you should do an inspection of the injured wrist, by comparing it to the other wrist. A sprained wrist can be swollen, red, tender and warm to touch.[1][7][8][9]
- When you have finished the inspection, you can palpate the wrist with all their structures. Most of the structures in the wrist are very good palpable, but swelling can hinder your palpation and the palpation can be painful for the patient.[4][10]
- After palpation, you should test each articulation in search of pain, abnormal motion or crepitus. The physiological movement of the wrist can be examined by simple tests of the palmar flexion, dorsiflexion, radial deviation and ulnar deviation.[9]
- You should also test the functional movement by letting the patient do things like catching, pinching, holding and managing simple objects.[9]
- When there is a severe swelling, you can expect that even the smallest mobilizations will be very painful for the patient.[7][9]
- you can do a resistance examination, to examine whether the muscle strength is still normal. You should do this for flexion (Fig.5), extension and ulnar and radial deviation.[9]
Beware this can be very painful or even impossible for patients with a severe wrist sprain when the passive mobilizations are already painful and not fully practicable. - The results of your tests and thus the functional disorders will depend on the severity of the injury.[4][7][9]
You can also run some more specific provocative wrist tests.[4][7][10]
- Scaphoid Watson shift test
- Lunotriquetral-ballotement-test
- Finger extensions against resistance
- Midcarpal test
- Distal radioulnar joint test
- Triangular fibrocartilage complex stress test
- Triangular fibrocartilage complex stress test with compression
- Gripping rotatory impaction test
These tests will give you more information about which ligaments are (partially) ruptured and instability of the wrist.[4]
Prosser et al[10]compared provocative wrist testing and MRI diagnostics to arthroscopic findings to assess their diagnostic value in 105 patients. The scaphoid shift test, midcarpal test, and DRUJ test had mild diagnostic usefulness. MRI was considered moderately useful for TFCC injury diagnostics and mildly useful for scapholunate ligament injury diagnostics[10].
Physical Therapy Management[edit | edit source]
Mild wrist sprains should follow the RICE method (discussed below) and may feel better in 24-48 hours[5].
Moderate to severe wrist sprains may need bracing to promote protection and healing of the area before, or while, progressing through the phases discussed below[5].
Phase 1[edit | edit source]
At first, you should follow the RICE method:[edit | edit source]
- Rest: Stop the activity and use of the injured wrist for 48 hours or until the pain and the swelling has subsided.[1]
- Ice: Apply a cold pack (wrapped in a towel) or a bag of crushed ice to the sprained wrist, for about 15 minutes, several a day for several days. Don’t ice it for more than 20 minutes at a time! [1]
- Cryotherapy will create a superficial vasoconstriction, so that the local blood flow and haemorrhage decrease.[4]There is some discussion about the effectiveness of cryotherapy, most studies approve the fact that cryotherapy has a pain-decreasing effect. There are also indications that cryotherapy would influence the inflammation, but more and bigger studies are required to prove evidence.[4][11]
- Compression: Wrap the wrist with an elastic compression bandage and limit swelling. The bandage should push the edema fluid away from the injured tissue. Start wrapping at the base of the fingers and stop just below the elbow, so that you wrap in the direction of the heart. The wrap should be snug, but be careful not cutting off circulation.[1][12]
- Elevate: Try to keep the wrist above heart level as often as possible, during two days. This will help drain fluid and reduce swelling around the wrist. Nonsteroidal anti-inflammatory drugs (NSAID) are also recommended.[1][12]
In case of a severe wrist sprain it can be recommended to immobilize the wrist. In some rare cases a surgery may be needed to repair a ligament that was torn completely.[4]
Phase 2[edit | edit source]
In a second phase the patient should do gradual retraining exercises, including[edit | edit source]
- Active mobilizations, to increase flexibility and range of motion,
- Exercises for the strengthening of the injured wrist.
- We have to start these exercises early in the rehabilitation, to prevent stiffness and weakness from developing and to ensure the wrist is functioning correctly. You can start exercising as soon as pain allows. It is very important that the patient is guided by the treating physiotherapist during the exercises.[13]
We prefer active mobilizations above the passive ones, but in some cases we can do passive mobilizations to treat hypomobility, by adding traction.[4][edit | edit source]
- First you can perform radiocarpal and midcarpal traction, to see whether this movement provokes pain. This handling can be used to treat hypomobility in different directions.[4][14]
- To stimulate flexion you should do the dorsal sliding technique. During this technique the convex carpal bones will move in dorsal direction over the concave surface of the distal radius. [4][14]
- To stimulate extension you have to do the volar sliding technique. This will cause a sliding of the convex carpal bones in the volar direction over the concave surface of the radius. [4][14]
- The ulnar sliding technique will stimulate radial deviation.[4][14]
- The radial sliding technique will stimulate ulnar deviation.[4][14]
After these passive mobilizations you can go to the active mobilizations.[4][edit | edit source]
- There are many exercises you can give to your patients, here are some examples.[4][14]
- Turning the wrists: hook your fingers into each other and turn the wrist in different directions.
- Place your forearms on a table and perform extension (arm in pronation on table) and flexion (arm in supination on table).
- Do the same for ulnar and radial deviation, you can do this one in pro- and in supination.
You can combine mobilizations with some stretching exercises for the extensors and flexors.[4][14][15][edit | edit source]
- Before you start to stretch, you should perform an isometric contraction and hold this for 5 seconds.[4][14][15]
After mobilizations you can start exercises to improve muscle strength.[edit | edit source]
- These exercises will be very similar to the mobilizations, except from the fact that you should use some tools. By tools we mean weights, Theraband, pull machine and many others. The goal of these tools is to put a resistance on the movement. You should start with a low resistance/weight and many repetitions to train the muscle endurance first, then gradually increase resistance/weight but decrease repetitions to train muscle strength, do this depending on the possibilities of the patient.[4][14]
- It can also be useful to do some proprioceptive exercises, especially for practicing sports, like gymnastics, where the athletes frequently us the hands as weight carriers. These exercises are often performed in push-up position. You will gradually change the surface under the hands starting with flat ground, followed by, normal pillow, Airex pad, Sissel pillow and wobble board.[4][14]
It is difficult to give information about the repetitions and the duration of the exercises, because this is strongly related to the patient and his advancement. It is also important to know what the final goal of the patient will be, does he just have to return to ADL-activities or is he an athlete who has to return to his sport and on which level? You will have to consider all these things when you set up a personal training program for a specific patient.[4][14]
When returning to sports activities, the therapist can prepare the patient by taping the wrist or adjust a brace.[1][4]
Surgical Intervention[edit | edit source]
Surgery may be indicated if patient struggles to improve with conservative management or if there is a full ligament tear. Surgical interventions may include surgical fixation, arthroscopic debridement, or open debridement[5].
References[edit | edit source]
- Morgan WJ, Slowman LS. Acute hand and wrist injuries in athletes: Evaluation and management. Journal of the American Academy of Orthopaedic surgeons, nov.-dec. 2001, vol. 9, n°: 6, 389-400. Evidence level: 2A
- Prof. Dr. R. Meeusen. Praktijkgids pols- en handletsels. Vrije Universiteit Brussel. Dienst uitgaven, 2006.
- Tricia J. Hubbard; Craig R. Denegar. Does Cryotherapy Improve Outcomes With Soft Tissue Injury? Pennsylvania State University, University Park, PA. Journal of Athletic Training. Volume 39. Number 3. September 2004. Evidence level: 1A. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC522152/?tool=pubmed
- Roald Bahr, Sverre Maehlum. Clinical Guide To Sports Injuries. 2004.
- Christian Dumontier. Physical Examination of wrist instabilities. [INTERNET] Evidence level: 5 http://www.maitrise-orthop.com/corpusmaitri/orthopaedic/dumontier_synth/dumontier_us.shtml
- Bentohami, et al. Amsterdam wrist rules: A clinical decision aid. BMC Musculoskeletal Disorders. 17 october 2011. Evidence level: 1B Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3229467/?tool=pubmed
- Wolfe MW, Uhl TL, Mattacola CG, McCluskey LC. Management of ankle sprains. Erratum in Am Fam Physician 2001 Aug1;64(3):386. Evidence level: 2C
- Peter Vaes, Eric Kerckhofs, David Beckwée. Het Gezondheidsprofiel. Standaard uitgeverij.
- Honing, E. Wrist injuries – pinpointing pathology in a complex joint. Phys sportsmed, 26(9): 41-49, 1998a. Evidence level: 5
- Prosser R, Harvey L, Lastayo P, Hargreaves I, Scougall P, Herbert RD. Provocative wrist tests and MRI are of limited diagnostic value for suspected wrist ligament injuries: a cross-sectional study. Australian Physiotherapy Association. Evidence level: 1B
- Rettig, A. Elbow, forearm and wrist injuries in athlete. Sports Med, 25(2):115-130, 1998. Evidence level: 2C
- Levine W. Rehabilitation techniques for ligament injuries of the wrist. Hand Clin 8(4):669-681, 1992. Evidence level: 5
- Wadsworth C. The wrist and hand. In: Malone T., McPoil T., Nitz A.. Orthopedic and sports physical therapy. Mosby, St. Louis, USA.pp. 327-378,1997
- Humphrey D. Flexibility for the wrist, fingers and thumbs. Phys Sportsmed, 18(12):147-148, 1990. Evidence level: 5
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Morgan WJ, Slowman LS. Acute hand and wrist injuries in athletes: Evaluation and management. Journal of the American Academy of Orthopaedic surgeons, nov.-dec. 2001, vol. 9, n°: 6, 389-400. Evidence level: 2A
- ↑ 2.0 2.1 Roald Bahr, Sverre Maehlum. Clinical Guide To Sports Injuries. 2004.
- ↑ Rettig, A. Elbow, forearm and wrist injuries in athlete. Sports Med, 25(2):115-130, 1998. Evidence level: 2C
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 4.15 4.16 4.17 4.18 4.19 4.20 4.21 4.22 Prof. Dr. R. Meeusen. Praktijkgids pols- en handletsels. Vrije Universiteit Brussel. Dienst uitgaven, 2006.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 5.8 May Jr DD, Varacallo M. Wrist Sprain. 2021 Jul 18. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan–.
- ↑ Bentohami, et al. Amsterdam wrist rules: A clinical decision aid. BMC Musculoskeletal Disorders. 17 october 2011. Evidence level: 1B Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3229467/?tool=pubmed
- ↑ 7.0 7.1 7.2 7.3 7.4 Christian Dumontier. Physical Examination of wrist instabilities. [INTERNET] Evidence level: 5 http://www.maitrise-orthop.com/corpusmaitri/orthopaedic/dumontier_synth/dumontier_us.shtml
- ↑ 8.0 8.1 Peter Vaes, Eric Kerckhofs, David Beckwée. Het Gezondheidsprofiel. Standaard uitgeverij.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 9.6 Honing, E. Wrist injuries – pinpointing pathology in a complex joint. Phys sportsmed, 26(9): 41-49, 1998a. Evidence level: 5
- ↑ 10.0 10.1 10.2 10.3 Prosser R, Harvey L, Lastayo P, Hargreaves I, Scougall P, Herbert RD. Provocative wrist tests and MRI are of limited diagnostic value for suspected wrist ligament injuries: a cross-sectional study. Australian Physiotherapy Association. Evidence level: 1B
- ↑ Tricia J. Hubbard; Craig R. Denegar. Does Cryotherapy Improve Outcomes With Soft Tissue Injury? Pennsylvania State University, University Park, PA. Journal of Athletic Training. Volume 39. Number 3. September 2004. Evidence level: 1A. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC522152/?tool=pubmed
- ↑ 12.0 12.1 Wolfe MW, Uhl TL, Mattacola CG, McCluskey LC. Management of ankle sprains. Erratum in Am Fam Physician 2001 Aug1;64(3):386. Evidence level: 2C
- ↑ Levine W. Rehabilitation techniques for ligament injuries of the wrist. Hand Clin 8(4):669-681, 1992. Evidence level: 5
- ↑ 14.00 14.01 14.02 14.03 14.04 14.05 14.06 14.07 14.08 14.09 14.10 Wadsworth C. The wrist and hand. In: Malone T., McPoil T., Nitz A.. Orthopedic and sports physical therapy. Mosby, St. Louis, USA.pp. 327-378,1997
- ↑ 15.0 15.1 Humphrey D. Flexibility for the wrist, fingers and thumbs. Phys Sportsmed, 18(12):147-148, 1990. Evidence level: 5
- ↑ Mathew Hawkes. Hawkes Physiotherapy Wrist sprain video. Available from: https://youtu.be/0AMIVnkcR0U [Accessed 2 Apr 2015]