Valgus stress to ulnar collateral ligament: Difference between revisions
(Clinical presentation paragraph added) |
m (Wendy Snyders moved page Valgus Stress to UCL to Valgus stress to ulna collateral ligament: Abbreviation used in title) |
(No difference)
| |
Revision as of 16:55, 12 February 2023
Top Contributors - Wendy Snyders, Rachael Lowe, Admin, Kim Jackson and George Prudden
Top Contributors - Wendy Snyders, Rachael Lowe, Admin, Kim Jackson and George Prudden
Clinically Relevant Anatomy[edit | edit source]
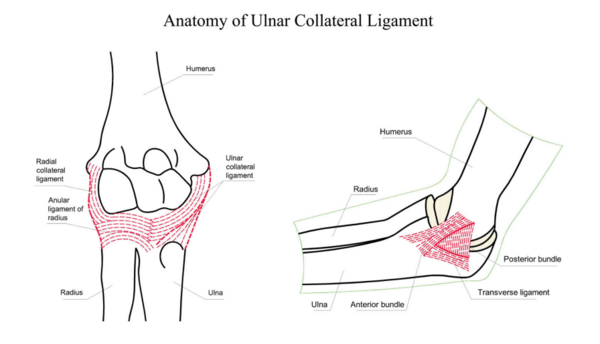
The ulna collateral ligament (UCL) consists of three bundles - the anterior oblique ligament/bundle (AOL), the posterior oblique ligament/bundle (POL) and the transverse ligament (which unites AOL and POL)[1][2]. Of the three bundles, the AOL is the strongest and provides significant restraint to valgus force when the elbow is between 30 and 120 degrees flexion. The UCL originates at the anterior-inferior aspect of the medial epicondyle of the humerus and it inserts at the sublime tubercle (the proximal aspect of the ulna)[1][2] . Its main functions are to stabilise the elbow joint and to resist valgus loads[1].
The UCL stabilises the elbow joint by slowing down elbow extension during throwing's deceleration phase and by generating a varus torque, counterbalancing the valgus force[1].
The proximal UCL is well vascularised and gets its blood supply from the recurrent flexor or pronator artery[3]. The distal aspect of the UCL is relatively hypovascularised[3].
Mechanism of Injury / Pathological Process[edit | edit source]
UCL injuries are usually due to chronic repetitive load rather than an acute injury[2][3] with tears typically occuring proximally[3]. Poor stabilisation together with repetitive near-failure tensile loads can lead to microtrauma, weaking the AOL and potentially leading to rupture or instability[1]. Acute ruptures typically occur during traumatic dislocations of the elbow, often associated with articular fractures[4].
Complete rupture of the AOL prevents countering of valgus stress during the acceleration phase of throwing, making forceful overhead throwing nearly impossible[1].
Clinical Presentation[edit | edit source]
Acute or sub-acute phase:
- Medial elbow pain[3]
- Medial swelling [2]
- Point tenderness along the ligament[2]
- No range-of-motion limitation (ROM)[2]
- Throwers may often recall feeling or hearing a "pop"[3].
- Ulna-nerve compression signs and symptoms - usually sensory[3].
Chronic:
- Medial elbow pain[3]
- Decreased velocity of accuracy with throwing
Athletes may also present for ulnar nerve compression symptoms, which are usually sensory[3].
Diagnostic Procedures[edit | edit source]
add text here relating to diagnostic tests for the condition
Outcome Measures[edit | edit source]
add links to outcome measures here (see Outcome Measures Database)
Management / Interventions
[edit | edit source]
add text here relating to management approaches to the condition
Differential Diagnosis
[edit | edit source]
add text here relating to the differential diagnosis of this condition
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Zaremski JL, Vincent KR, Vincent HK. Elbow ulnar collateral ligament: injury, treatment options, and recovery in overhead throwing athletes. Current Sports Medicine Reports. 2019 Sep 1;18(9):338-45.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Biz C, Crimi A, Belluzzi E, Maschio N, Baracco R, Volpin A, Ruggieri P. Conservative versus surgical management of elbow medial ulnar collateral ligament injury: a systematic review. Orthopaedic Surgery. 2019 Dec;11(6):974-84.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 Gehrman MD, Grandizio LC. Elbow ulnar collateral ligament injuries in throwing athletes: diagnosis and management. The Journal of Hand Surgery. 2022 Mar 1;47(3):266-73.
- ↑ 4.0 4.1 Biz C, Crimi A, Belluzzi E, Maschio N, Baracco R, Volpin A, Ruggieri P. Conservative versus surgical management of elbow medial ulnar collateral ligament injury: a systematic review. Orthopaedic Surgery. 2019 Dec;11(6):974-84.
References






