Treatment of Plantar Heel Pain - A Literature Review: Difference between revisions
No edit summary |
No edit summary |
||
| Line 39: | Line 39: | ||
</ref><ref>Shanks P, Curran M, Fletcher P, Thompson R. [http://nectar.northampton.ac.uk/2923/7/Shanks20102923.pdf The effectiveness of therapeutic ultrasound for musculoskeletal conditions of the lower limb: A literature review]. The Foot. 2010 Dec 1;20(4):133-9. </ref>. | </ref><ref>Shanks P, Curran M, Fletcher P, Thompson R. [http://nectar.northampton.ac.uk/2923/7/Shanks20102923.pdf The effectiveness of therapeutic ultrasound for musculoskeletal conditions of the lower limb: A literature review]. The Foot. 2010 Dec 1;20(4):133-9. </ref>. | ||
[[File:PHP Treatment by ultrasound.jpg|frameless| | [[File:PHP Treatment by ultrasound.jpg|frameless|500x500px|alt=]] | ||
'''Figure 4'''. Studies investigating the treatment of PHP by ultrasound | '''Figure 4'''. Studies investigating the treatment of PHP by ultrasound | ||
| Line 48: | Line 48: | ||
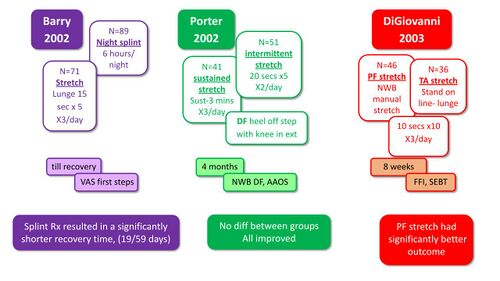
[[Stretching]] of the triceps surae muscles has been proposed in many studies as an essential part of the management of plantar fasciitis <ref name=":8" />. The aim of stretching is to release tension in the [[Achilles Tendon|Achilles tendon]] and [[Plantar Aponeurosis|plantar fascia]], both of which attach to the [[calcaneus]] <ref name=":8" />. Many studies have investigated the use of stretching for the treatment of PHPS, often with conflicting results. Several studies compared the use of various stretches for PHPS and generally found that all groups improved with Barry et al <ref name=":11">Barry LD, Barry AN, Chen Y. [https://pubmed.ncbi.nlm.nih.gov/12194511/ A retrospective study of standing gastrocnemius-soleus stretching versus night splinting in the treatment of plantar fasciitis]. The Journal of foot and ankle surgery. 2002 Jul 1;41(4):221-7. </ref> also reporting a shorter recovery time with the use of night splinting (Figure 5) <ref name=":11" /><ref name=":12">DiGiovanni BF, Nawoczenski DA, Malay DP, Graci PA, Williams TT, Wilding GE, Baumhauer JF. [http://www.ucsm.ca/documents/Plantar%20Fasciitis%20reading.pdf Plantar fascia-specific stretching exercise improves outcomes in patients with chronic plantar fasciitis: a prospective clinical trial with two-year follow-up]. JBJS. 2006 Aug 1;88(8):1775-81. </ref><ref name=":13">Porter D, Barrill E, Oneacre K, May BD. [https://pubmed.ncbi.nlm.nih.gov/12146772/ The effects of duration and frequency of Achilles tendon stretching on dorsiflexion and outcome in painful heel syndrome: a randomized, blinded, control study]. Foot & ankle international. 2002 Jul;23(7):619-24. </ref>. | [[Stretching]] of the triceps surae muscles has been proposed in many studies as an essential part of the management of plantar fasciitis <ref name=":8" />. The aim of stretching is to release tension in the [[Achilles Tendon|Achilles tendon]] and [[Plantar Aponeurosis|plantar fascia]], both of which attach to the [[calcaneus]] <ref name=":8" />. Many studies have investigated the use of stretching for the treatment of PHPS, often with conflicting results. Several studies compared the use of various stretches for PHPS and generally found that all groups improved with Barry et al <ref name=":11">Barry LD, Barry AN, Chen Y. [https://pubmed.ncbi.nlm.nih.gov/12194511/ A retrospective study of standing gastrocnemius-soleus stretching versus night splinting in the treatment of plantar fasciitis]. The Journal of foot and ankle surgery. 2002 Jul 1;41(4):221-7. </ref> also reporting a shorter recovery time with the use of night splinting (Figure 5) <ref name=":11" /><ref name=":12">DiGiovanni BF, Nawoczenski DA, Malay DP, Graci PA, Williams TT, Wilding GE, Baumhauer JF. [http://www.ucsm.ca/documents/Plantar%20Fasciitis%20reading.pdf Plantar fascia-specific stretching exercise improves outcomes in patients with chronic plantar fasciitis: a prospective clinical trial with two-year follow-up]. JBJS. 2006 Aug 1;88(8):1775-81. </ref><ref name=":13">Porter D, Barrill E, Oneacre K, May BD. [https://pubmed.ncbi.nlm.nih.gov/12146772/ The effects of duration and frequency of Achilles tendon stretching on dorsiflexion and outcome in painful heel syndrome: a randomized, blinded, control study]. Foot & ankle international. 2002 Jul;23(7):619-24. </ref>. | ||
[[File:Stretches and PHPS.jpg|frameless| | [[File:Stretches and PHPS.jpg|frameless|500x500px|alt=]] | ||
'''Figure 5'''. Research studies comparing various stretching regimes <ref name=":7" /><ref name=":11" /><ref name=":12" /><ref name=":13" /> | '''Figure 5'''. Research studies comparing various stretching regimes <ref name=":7" /><ref name=":11" /><ref name=":12" /><ref name=":13" /> | ||
| Line 56: | Line 56: | ||
</ref><ref name=":16">Kamonseki DH, Gonçalves GA, Liu CY, Júnior IL. [https://www.sciencedirect.com/science/article/abs/pii/S1356689X15001964?via%3Dihub Effect of stretching with and without muscle strengthening exercises for the foot and hip in patients with plantar fasciitis: a randomized controlled single-blind clinical trial]. Manual therapy. 2016 Jun 1;23:76-82. </ref>. | </ref><ref name=":16">Kamonseki DH, Gonçalves GA, Liu CY, Júnior IL. [https://www.sciencedirect.com/science/article/abs/pii/S1356689X15001964?via%3Dihub Effect of stretching with and without muscle strengthening exercises for the foot and hip in patients with plantar fasciitis: a randomized controlled single-blind clinical trial]. Manual therapy. 2016 Jun 1;23:76-82. </ref>. | ||
[[File:Studies Stretches and PHPS.jpg|frameless| | [[File:Studies Stretches and PHPS.jpg|frameless|500x500px|alt=]] | ||
'''Figure 6'''. Stretching compared to other forms of treatment <ref name=":7" /><ref name=":14" /><ref name=":15" /><ref name=":16" /> | '''Figure 6'''. Stretching compared to other forms of treatment <ref name=":7" /><ref name=":14" /><ref name=":15" /><ref name=":16" /> | ||
| Line 72: | Line 72: | ||
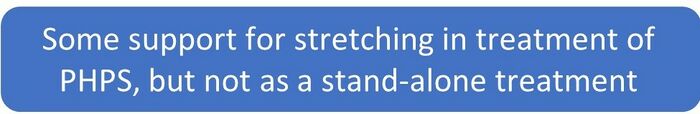
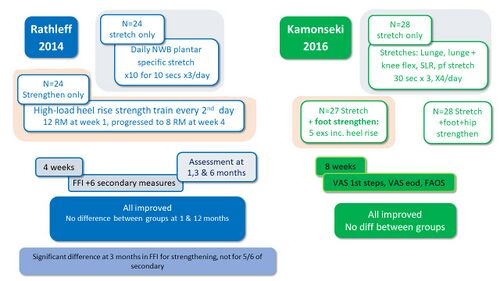
Weakness of the intrinsic [[Foot Anatomy|foot muscles]] as well as the ankle plantar flexors have been proposed as risk factors for the development of PHPS and prompted the use of strengthening as a treatment for PHPS <ref name=":5" />. Several studies investigated the effect of strengthening on PHPS and reported improvement in all groups with no advantage to strengthening in the management of PHPS, except after 3 months of plantar-specific stretching (Figure 6) <ref name=":16" /><ref name=":17">Rathleff MS, Mølgaard CM, Fredberg U, Kaalund S, Andersen KB, Jensen TT, Aaskov S, Olesen JL. [https://onlinelibrary.wiley.com/doi/10.1111/sms.12313 High‐load strength training improves outcome in patients with plantar fasciitis: A randomized controlled trial with 12‐month follow‐up]. Scandinavian journal of medicine & science in sports. 2015 Jun;25(3):e292-300. </ref>. | Weakness of the intrinsic [[Foot Anatomy|foot muscles]] as well as the ankle plantar flexors have been proposed as risk factors for the development of PHPS and prompted the use of strengthening as a treatment for PHPS <ref name=":5" />. Several studies investigated the effect of strengthening on PHPS and reported improvement in all groups with no advantage to strengthening in the management of PHPS, except after 3 months of plantar-specific stretching (Figure 6) <ref name=":16" /><ref name=":17">Rathleff MS, Mølgaard CM, Fredberg U, Kaalund S, Andersen KB, Jensen TT, Aaskov S, Olesen JL. [https://onlinelibrary.wiley.com/doi/10.1111/sms.12313 High‐load strength training improves outcome in patients with plantar fasciitis: A randomized controlled trial with 12‐month follow‐up]. Scandinavian journal of medicine & science in sports. 2015 Jun;25(3):e292-300. </ref>. | ||
[[File:Studies Strengthening and PHPS.jpg|frameless| | [[File:Studies Strengthening and PHPS.jpg|frameless|500x500px|alt=]] | ||
'''Figure 6'''. Effect of strengthening on PHPS <ref name=":7" /><ref name=":16" /><ref name=":17" /> | '''Figure 6'''. Effect of strengthening on PHPS <ref name=":7" /><ref name=":16" /><ref name=":17" /> | ||
| Line 81: | Line 81: | ||
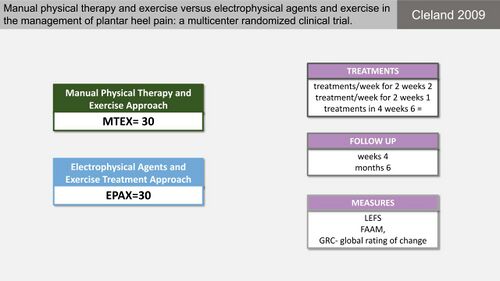
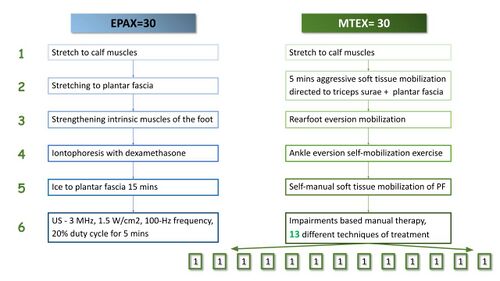
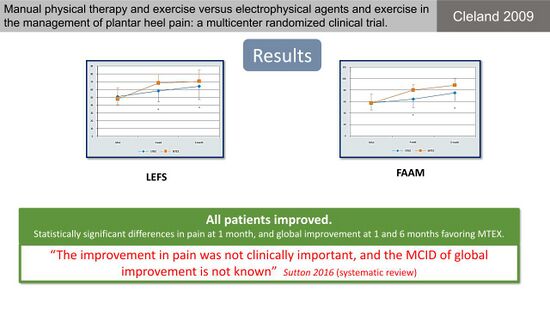
Physiotherapists often use manual therapy to improve joint mobility, mobilise soft tissue and reduce pain <ref name=":18">Mischke JJ, Jayaseelan DJ, Sault JD, Emerson Kavchak AJ. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5539575/pdf/yjmt-25-3.pdf The symptomatic and functional effects of manual physical therapy on plantar heel pain: a systematic review]. Journal of Manual & Manipulative Therapy. 2017 Jan 1;25(1):3-10. </ref><ref name=":19">Hasegawa M, Urits I, Orhurhu V, Orhurhu MS, Brinkman J, Giacomazzi S, Foster L, Manchikanti L, Kaye AD, Kaye RJ, Viswanath O. [https://sci-hub.se/10.1007/s11916-020-00883-7 Current concepts of minimally invasive treatment options for plantar fasciitis: A comprehensive review]. Current Pain and Headache Reports. 2020 Sep;24(9):1-1.</ref>. Current literature on the use of manual therapy for patients with PHP is however sparse and often of lesser quality <ref name=":18" />. Cleland et al <ref name=":20">Cleland JA, Abbott JH, Kidd MO, Stockwell S, Cheney S, Gerrard DF, Flynn TW. [https://www.jospt.org/doi/pdfplus/10.2519/jospt.2009.3036 Manual physical therapy and exercise versus electrophysical agents and exercise in the management of plantar heel pain: a multicenter randomized clinical trial]. journal of orthopaedic & sports physical therapy. 2009 Aug;39(8):573-85. </ref> conducted a study on the efficacy of manual therapy and exercise (MTEX) compared to electro-physical agents and exercise (EPAX) in the management of PHPS (Figure 7). Both treatment groups however, received multiple different interventions which is problematic for interpreting which intervention made the difference (Figure 8). They concluded that all patients improved with statistically significant differences between groups regarding pain and global improvement favouring MTEX (Figure 9) <ref name=":20" />. There is however not enough information about the clinical effects of the treatment. | Physiotherapists often use manual therapy to improve joint mobility, mobilise soft tissue and reduce pain <ref name=":18">Mischke JJ, Jayaseelan DJ, Sault JD, Emerson Kavchak AJ. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5539575/pdf/yjmt-25-3.pdf The symptomatic and functional effects of manual physical therapy on plantar heel pain: a systematic review]. Journal of Manual & Manipulative Therapy. 2017 Jan 1;25(1):3-10. </ref><ref name=":19">Hasegawa M, Urits I, Orhurhu V, Orhurhu MS, Brinkman J, Giacomazzi S, Foster L, Manchikanti L, Kaye AD, Kaye RJ, Viswanath O. [https://sci-hub.se/10.1007/s11916-020-00883-7 Current concepts of minimally invasive treatment options for plantar fasciitis: A comprehensive review]. Current Pain and Headache Reports. 2020 Sep;24(9):1-1.</ref>. Current literature on the use of manual therapy for patients with PHP is however sparse and often of lesser quality <ref name=":18" />. Cleland et al <ref name=":20">Cleland JA, Abbott JH, Kidd MO, Stockwell S, Cheney S, Gerrard DF, Flynn TW. [https://www.jospt.org/doi/pdfplus/10.2519/jospt.2009.3036 Manual physical therapy and exercise versus electrophysical agents and exercise in the management of plantar heel pain: a multicenter randomized clinical trial]. journal of orthopaedic & sports physical therapy. 2009 Aug;39(8):573-85. </ref> conducted a study on the efficacy of manual therapy and exercise (MTEX) compared to electro-physical agents and exercise (EPAX) in the management of PHPS (Figure 7). Both treatment groups however, received multiple different interventions which is problematic for interpreting which intervention made the difference (Figure 8). They concluded that all patients improved with statistically significant differences between groups regarding pain and global improvement favouring MTEX (Figure 9) <ref name=":20" />. There is however not enough information about the clinical effects of the treatment. | ||
[[File:Cleland 2009 MT and PHPS study.jpg|frameless| | [[File:Cleland 2009 MT and PHPS study.jpg|frameless|500x500px|alt=]] | ||
'''Figure 7'''. Manual therapy and exercise compared to Electro-physical agents and exercise for PHPS <ref name=":7" /><ref name=":20" /> | '''Figure 7'''. Manual therapy and exercise compared to Electro-physical agents and exercise for PHPS <ref name=":7" /><ref name=":20" /> | ||
[[File:MT vs EFT group treatment details Cleland 2009.jpg|frameless| | [[File:MT vs EFT group treatment details Cleland 2009.jpg|frameless|500x500px|alt=]] | ||
'''Figure 8'''. Treatment details of the groups in the study by Cleland et al <ref name=":20" /><ref name=":7" /> | '''Figure 8'''. Treatment details of the groups in the study by Cleland et al <ref name=":20" /><ref name=":7" /> | ||
[[File:Results MT vs EFT Cleland 2009.jpg|frameless| | [[File:Results MT vs EFT Cleland 2009.jpg|frameless|550x550px|alt=]] | ||
'''Figure 9'''. Results of the comparison between Manual therapy and electro-physical agents for PHPS <ref name=":7" /><ref name=":20" /> | '''Figure 9'''. Results of the comparison between Manual therapy and electro-physical agents for PHPS <ref name=":7" /><ref name=":20" /> | ||
| Line 95: | Line 95: | ||
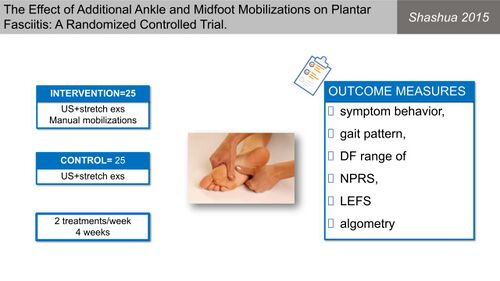
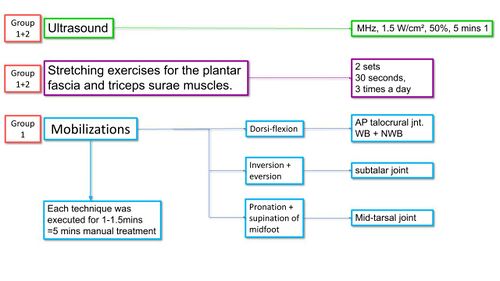
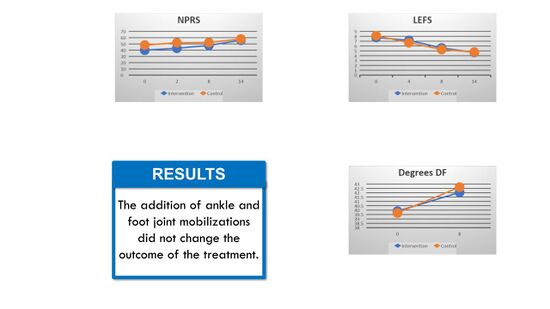
Shashua et al <ref name=":21">Shashua A, Flechter S, Avidan L, Ofir D, Melayev A, Kalichman L. [https://www.jospt.org/doi/pdfplus/10.2519/jospt.2015.5155 The effect of additional ankle and midfoot mobilizations on plantar fasciitis: a randomized controlled trial]. Journal of Orthopaedic & Sports Physical Therapy. 2015 Apr;45(4):265-72. </ref> also investigated the effect of manual therapy on [[Plantar Fasciitis|plantar fasciitis]] (Figure 10) with the treatment group receiving manual therapy, ultrasound and stretch exercises and the control group only ultrasound and stretch exercises (Figure 11). They reported an improvement in both groups with no difference between groups, indicating no additional advantage to manual therapy for PHPS (Figure 12)<ref name=":21" />. | Shashua et al <ref name=":21">Shashua A, Flechter S, Avidan L, Ofir D, Melayev A, Kalichman L. [https://www.jospt.org/doi/pdfplus/10.2519/jospt.2015.5155 The effect of additional ankle and midfoot mobilizations on plantar fasciitis: a randomized controlled trial]. Journal of Orthopaedic & Sports Physical Therapy. 2015 Apr;45(4):265-72. </ref> also investigated the effect of manual therapy on [[Plantar Fasciitis|plantar fasciitis]] (Figure 10) with the treatment group receiving manual therapy, ultrasound and stretch exercises and the control group only ultrasound and stretch exercises (Figure 11). They reported an improvement in both groups with no difference between groups, indicating no additional advantage to manual therapy for PHPS (Figure 12)<ref name=":21" />. | ||
[[File:Shashua 2015 Manual therapy and PF.jpg|frameless| | [[File:Shashua 2015 Manual therapy and PF.jpg|frameless|500x500px|alt=]] | ||
'''Figure 10'''. Manual therapy for Plantar fasciitis <ref name=":7" /><ref name=":21" /> | '''Figure 10'''. Manual therapy for Plantar fasciitis <ref name=":7" /><ref name=":21" /> | ||
[[File:Treatment between groups MT study Shashua 2015.jpg|frameless| | [[File:Treatment between groups MT study Shashua 2015.jpg|frameless|500x500px|alt=]] | ||
'''Figure 11'''. Treatment details for both groups in the study by Shashua et al <ref name=":21" /><ref name=":7" /> | '''Figure 11'''. Treatment details for both groups in the study by Shashua et al <ref name=":21" /><ref name=":7" /> | ||
[[File:Results MT study Shashua 2015.jpg|frameless| | [[File:Results MT study Shashua 2015.jpg|frameless|550x550px|alt=]] | ||
'''Figure 12'''. Results on the effect of manual therapy for plantar fasciitis <ref name=":7" /><ref name=":21" /> | '''Figure 12'''. Results on the effect of manual therapy for plantar fasciitis <ref name=":7" /><ref name=":21" /> | ||
| Line 112: | Line 112: | ||
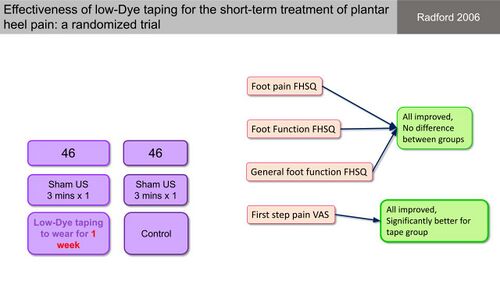
[[Taping]] is proposed to be associated with pain reduction, increased circulation and improved proprioception, all of which would be beneficial for the management of PHPS <ref name=":22">Tsai CT, Chang WD, Lee JP. [http://www.rocktape.pt/downloads/plantarfascitisstudy.pdf Effects of short-term treatment with kinesiotaping for plantar fasciitis]. Journal of Musculoskeletal Pain. 2010 Jan 1;18(1):71-80. </ref>. Radford et al <ref name=":23">Radford JA, Landorf KB, Buchbinder R, Cook C. [https://bmcmusculoskeletdisord.biomedcentral.com/track/pdf/10.1186/1471-2474-7-64.pdf Effectiveness of low-Dye taping for the short-term treatment of plantar heel pain: a randomised trial]. BMC musculoskeletal disorders. 2006 Dec;7(1):1-7. </ref> applied standardised leukotape to the plantar skin of patients and kept it in situ for 7 days, which they compared to a control group. Both groups improved and there was no significant reduction in heel pain intensity in the taping group compared to the controls <ref name=":2" /><ref name=":23" />. First step pain, however, was significantly better in the taping group compared to the controls (Figure 13) <ref name=":23" />. | [[Taping]] is proposed to be associated with pain reduction, increased circulation and improved proprioception, all of which would be beneficial for the management of PHPS <ref name=":22">Tsai CT, Chang WD, Lee JP. [http://www.rocktape.pt/downloads/plantarfascitisstudy.pdf Effects of short-term treatment with kinesiotaping for plantar fasciitis]. Journal of Musculoskeletal Pain. 2010 Jan 1;18(1):71-80. </ref>. Radford et al <ref name=":23">Radford JA, Landorf KB, Buchbinder R, Cook C. [https://bmcmusculoskeletdisord.biomedcentral.com/track/pdf/10.1186/1471-2474-7-64.pdf Effectiveness of low-Dye taping for the short-term treatment of plantar heel pain: a randomised trial]. BMC musculoskeletal disorders. 2006 Dec;7(1):1-7. </ref> applied standardised leukotape to the plantar skin of patients and kept it in situ for 7 days, which they compared to a control group. Both groups improved and there was no significant reduction in heel pain intensity in the taping group compared to the controls <ref name=":2" /><ref name=":23" />. First step pain, however, was significantly better in the taping group compared to the controls (Figure 13) <ref name=":23" />. | ||
[[File:Radford 2006 Taping vs controls.jpg|frameless| | [[File:Radford 2006 Taping vs controls.jpg|frameless|500x500px|alt=]] | ||
'''Figure 13'''. Effectiveness of low-Dye taping for the treatment of PHPS <ref name=":7" /><ref name=":23" /> | '''Figure 13'''. Effectiveness of low-Dye taping for the treatment of PHPS <ref name=":7" /><ref name=":23" /> | ||
| Line 118: | Line 118: | ||
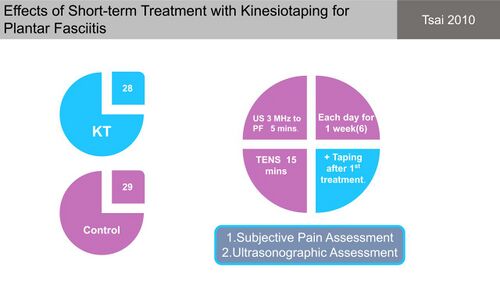
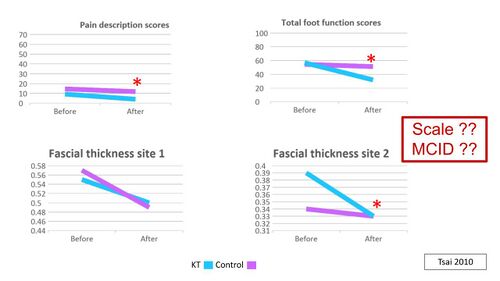
Tsai et al <ref name=":22" /> compared the use of kinesiotape for plantar fasciitis, applied over the gastrocnemius and plantar fascia and kept in situ for one week, to a control group (Figure 14). Both groups reported a significant reduction in pain and there was a significant difference in pain reduction between the groups, but this was also reported before intervention. No differences in plantar fascia thickness were found between groups <ref name=":22" />. This study, however, had insufficient information to accurately interpret its measurements and come to a final conclusion about the treatment effects (Figure 15) <ref name=":7" />. | Tsai et al <ref name=":22" /> compared the use of kinesiotape for plantar fasciitis, applied over the gastrocnemius and plantar fascia and kept in situ for one week, to a control group (Figure 14). Both groups reported a significant reduction in pain and there was a significant difference in pain reduction between the groups, but this was also reported before intervention. No differences in plantar fascia thickness were found between groups <ref name=":22" />. This study, however, had insufficient information to accurately interpret its measurements and come to a final conclusion about the treatment effects (Figure 15) <ref name=":7" />. | ||
[[File:Tsai 2010 kinesiotape vs control PHPS.jpg|frameless| | [[File:Tsai 2010 kinesiotape vs control PHPS.jpg|frameless|500x500px|alt=]] | ||
'''Figure 14'''. Kinesiotaping versus control group <ref name=":7" /><ref name=":22" /> | '''Figure 14'''. Kinesiotaping versus control group <ref name=":7" /><ref name=":22" /> | ||
[[File:Results KT and control Tsai 2010.jpg|frameless| | [[File:Results KT and control Tsai 2010.jpg|frameless|500x500px|alt=]] | ||
'''Figure 15'''. Results of the study by Tsai et al <ref name=":22" /><ref name=":7" /> | '''Figure 15'''. Results of the study by Tsai et al <ref name=":22" /><ref name=":7" /> | ||
| Line 134: | Line 134: | ||
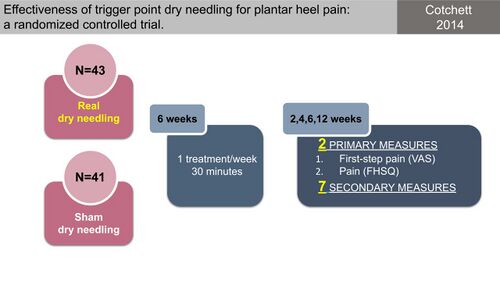
</ref><ref name=":25">Cotchett MP, Landorf KB, Munteanu SE. [https://link.springer.com/content/pdf/10.1186/1757-1146-3-18.pdf Effectiveness of dry needling and injections of myofascial trigger points associated with plantar heel pain: a systematic review]. Journal of foot and ankle research. 2010 Dec;3(1):1-9. </ref>. Limited evidence for the effectiveness of dry needling was however reported in a systematic review on dry needling for PHPS and the poor quality of the studies precluded making definite conclusions <ref name=":25" />. Following this, Cotchett et al <ref name=":24" /> conducted a study to determine the efficacy of trigger point dry needling for PHPS (Figure 16) and compared “real dry needling” into the myofascial trigger points of a variety of muscles (Figure 17) to sham dry needling. They found that even though real dry needling provided statistically significant reductions in PHP compared to sham dry needling, the size of the effect was not clinically meaningful (Figure 18) <ref name=":24" />. | </ref><ref name=":25">Cotchett MP, Landorf KB, Munteanu SE. [https://link.springer.com/content/pdf/10.1186/1757-1146-3-18.pdf Effectiveness of dry needling and injections of myofascial trigger points associated with plantar heel pain: a systematic review]. Journal of foot and ankle research. 2010 Dec;3(1):1-9. </ref>. Limited evidence for the effectiveness of dry needling was however reported in a systematic review on dry needling for PHPS and the poor quality of the studies precluded making definite conclusions <ref name=":25" />. Following this, Cotchett et al <ref name=":24" /> conducted a study to determine the efficacy of trigger point dry needling for PHPS (Figure 16) and compared “real dry needling” into the myofascial trigger points of a variety of muscles (Figure 17) to sham dry needling. They found that even though real dry needling provided statistically significant reductions in PHP compared to sham dry needling, the size of the effect was not clinically meaningful (Figure 18) <ref name=":24" />. | ||
[[File:Dry needling for PHPS Cotchett 2014.jpg|frameless| | [[File:Dry needling for PHPS Cotchett 2014.jpg|frameless|500x500px|alt=]] | ||
'''Figure 16'''. Effectiveness of trigger point dry needling for PHPS <ref name=":7" /><ref name=":24" /> | '''Figure 16'''. Effectiveness of trigger point dry needling for PHPS <ref name=":7" /><ref name=":24" /> | ||
[[File:Myofascial trigger points dry needled Cotchett 2014.jpg|frameless| | [[File:Myofascial trigger points dry needled Cotchett 2014.jpg|frameless|500x500px|alt=]] | ||
'''Figure 17'''. Different muscles in which trigger points were dry needled <ref name=":7" /><ref name=":24" /> | '''Figure 17'''. Different muscles in which trigger points were dry needled <ref name=":7" /><ref name=":24" /> | ||
[[File:Dry needling and PHPS results Cotchett 2014.jpg|frameless| | [[File:Dry needling and PHPS results Cotchett 2014.jpg|frameless|500x500px|alt=]] | ||
'''Figure 18'''. Outcome of real vs sham dry needling <ref name=":7" /><ref name=":24" /> | '''Figure 18'''. Outcome of real vs sham dry needling <ref name=":7" /><ref name=":24" /> | ||
| Line 151: | Line 151: | ||
[[Cryotherapy|Ice/cryotherapy]] is generally considered as a basic component in the management of any injury due to its proposed effectiveness in reducing swelling and relieving short-term pain <ref name=":10" />. It has thereby also been proposed as a treatment option for PHP as for many other musculoskeletal conditions <ref name=":10" /><ref name=":19" />. Costantino et al <ref name=":10" /> conducted a study comparing cryoultrasound to only cryotherapy and found that all patients improved but the ultrasound group showed a larger improvement (Figure 19). | [[Cryotherapy|Ice/cryotherapy]] is generally considered as a basic component in the management of any injury due to its proposed effectiveness in reducing swelling and relieving short-term pain <ref name=":10" />. It has thereby also been proposed as a treatment option for PHP as for many other musculoskeletal conditions <ref name=":10" /><ref name=":19" />. Costantino et al <ref name=":10" /> conducted a study comparing cryoultrasound to only cryotherapy and found that all patients improved but the ultrasound group showed a larger improvement (Figure 19). | ||
[[File:Cryoultrasound vs cryotherapy Costantino 2014.jpg|frameless| | [[File:Cryoultrasound vs cryotherapy Costantino 2014.jpg|frameless|500x500px|alt=]] | ||
'''Figure 19'''. Cryoultrasound vs cryotherapy for chronic plantar fasciitis <ref name=":7" /><ref name=":10" /> | '''Figure 19'''. Cryoultrasound vs cryotherapy for chronic plantar fasciitis <ref name=":7" /><ref name=":10" /> | ||
| Line 175: | Line 175: | ||
</ref>. | </ref>. | ||
[[File:Studies on orthoses in PHPS.jpg|frameless| | [[File:Studies on orthoses in PHPS.jpg|frameless|500x500px|alt=]] | ||
'''Figure 21'''. Good quality studies on the use of orthoses/insoles for PHPS <ref name=":7" /> | '''Figure 21'''. Good quality studies on the use of orthoses/insoles for PHPS <ref name=":7" /> | ||
[[File:Study details studies on foot orthoses and PHPS.jpg|frameless| | [[File:Study details studies on foot orthoses and PHPS.jpg|frameless|500x500px|alt=]] | ||
'''Figure 22'''. Study details of the four studies on orthoses for PHPS <ref name=":7" /><ref name=":26" /><ref name=":27" /><ref name=":28" /><ref name=":29" /> | '''Figure 22'''. Study details of the four studies on orthoses for PHPS <ref name=":7" /><ref name=":26" /><ref name=":27" /><ref name=":28" /><ref name=":29" /> | ||
[[File:Results on the most effective insole for PHPS.jpg|frameless| | [[File:Results on the most effective insole for PHPS.jpg|frameless|500x500px|alt=]] | ||
'''Figure 23'''. Results on the most effective insole for PHPS <ref name=":7" /> | '''Figure 23'''. Results on the most effective insole for PHPS <ref name=":7" /> | ||
| Line 191: | Line 191: | ||
</ref> compared the effect of magnetic versus sham-magnetic insoles on PHP and found no benefit to magnetic insoles compared to sham-magnetic inserts (Figure 24). | </ref> compared the effect of magnetic versus sham-magnetic insoles on PHP and found no benefit to magnetic insoles compared to sham-magnetic inserts (Figure 24). | ||
[[File:Magnetic vs sham-magnetic insoles for PHPS Winemillar 2003.jpg|frameless| | [[File:Magnetic vs sham-magnetic insoles for PHPS Winemillar 2003.jpg|frameless|500x500px|alt=]] | ||
'''Figure 24'''. Magnetic insoles vs sham-magnetic insoles for PHP <ref name=":7" /><ref name=":30" /> | '''Figure 24'''. Magnetic insoles vs sham-magnetic insoles for PHP <ref name=":7" /><ref name=":30" /> | ||
| Line 206: | Line 206: | ||
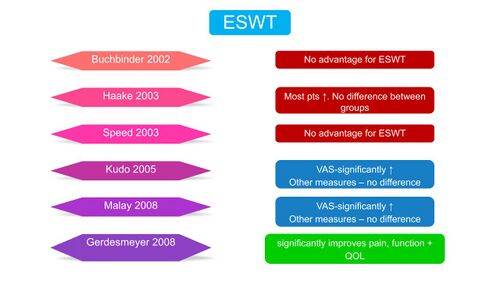
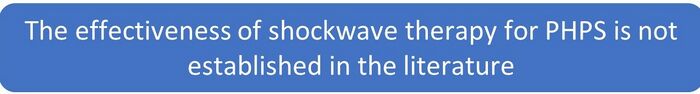
Several studies, many of poor methodological quality, explored the effect of ESWT on PHPS with conflicting results (Figure 25). | Several studies, many of poor methodological quality, explored the effect of ESWT on PHPS with conflicting results (Figure 25). | ||
[[File:Studies on ESWT for PHPS.jpg|frameless| | [[File:Studies on ESWT for PHPS.jpg|frameless|500x500px|alt=]] | ||
'''Figure 25'''. Evidence for the use of ESWT in PHPS <ref name=":7" /><ref name=":31" /><ref name=":32">Gerdesmeyer L, Frey C, Vester J, Maier M, Lowell Jr W, Weil Sr L, Russlies M, Stienstra J, Scurran B, Fedder K, Diehl P. [https://journals.sagepub.com/doi/10.1177/0363546508324176 Radial extracorporeal shock wave therapy is safe and effective in the treatment of chronic recalcitrant plantar fasciitis: results of a confirmatory randomized placebo-controlled multicenter study]. The American journal of sports medicine. 2008 Nov;36(11):2100-9. | '''Figure 25'''. Evidence for the use of ESWT in PHPS <ref name=":7" /><ref name=":31" /><ref name=":32">Gerdesmeyer L, Frey C, Vester J, Maier M, Lowell Jr W, Weil Sr L, Russlies M, Stienstra J, Scurran B, Fedder K, Diehl P. [https://journals.sagepub.com/doi/10.1177/0363546508324176 Radial extracorporeal shock wave therapy is safe and effective in the treatment of chronic recalcitrant plantar fasciitis: results of a confirmatory randomized placebo-controlled multicenter study]. The American journal of sports medicine. 2008 Nov;36(11):2100-9. | ||
| Line 233: | Line 233: | ||
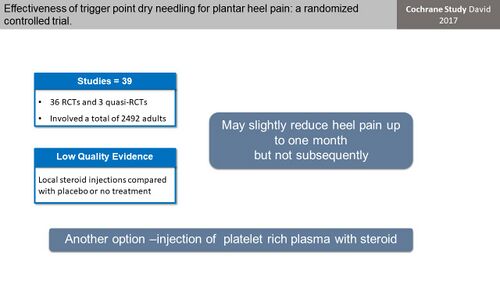
Corticosteroid injections are used in multiple musculoskeletal conditions, including PHP, as a way of relieving pain <ref name=":19" /><ref name=":33">David JA, Sankarapandian V, Christopher PR, Chatterjee A, Macaden AS. [https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD009348.pub2/full Injected corticosteroids for treating plantar heel pain in adults]. Cochrane Database of Systematic Reviews. 2017(6). CD009348. </ref>. In a Cochrane review, David et al <ref name=":33" /> reported low quality evidence that local steroid injections may slightly reduce PHP for up to one month, compared to placebo or no treatment (Figure 27). | Corticosteroid injections are used in multiple musculoskeletal conditions, including PHP, as a way of relieving pain <ref name=":19" /><ref name=":33">David JA, Sankarapandian V, Christopher PR, Chatterjee A, Macaden AS. [https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD009348.pub2/full Injected corticosteroids for treating plantar heel pain in adults]. Cochrane Database of Systematic Reviews. 2017(6). CD009348. </ref>. In a Cochrane review, David et al <ref name=":33" /> reported low quality evidence that local steroid injections may slightly reduce PHP for up to one month, compared to placebo or no treatment (Figure 27). | ||
[[File:Steroids for PHP David 2017.jpg|frameless| | [[File:Steroids for PHP David 2017.jpg|frameless|500x500px|alt=]] | ||
'''Figure 27'''. Cochrane review of injected corticosteroids for the treatment of PHP <ref name=":7" /><ref name=":33" /> | '''Figure 27'''. Cochrane review of injected corticosteroids for the treatment of PHP <ref name=":7" /><ref name=":33" /> | ||
| Line 250: | Line 250: | ||
The outcomes following plantar fasciotomy vary but generally shows good early pain relief and return to function in the short term <ref name=":34" />. Many individuals however experience ongoing pain and functional limitations and a retrospective study by Gibbons et al <ref name=":34" /> demonstrated that even though 72% of patients reported long-term satisfaction with the surgery, 44% continued to experience ongoing pain, swelling and tenderness (Figure 28). | The outcomes following plantar fasciotomy vary but generally shows good early pain relief and return to function in the short term <ref name=":34" />. Many individuals however experience ongoing pain and functional limitations and a retrospective study by Gibbons et al <ref name=":34" /> demonstrated that even though 72% of patients reported long-term satisfaction with the surgery, 44% continued to experience ongoing pain, swelling and tenderness (Figure 28). | ||
[[File:Plantar fasciotomy evidence Gibbons 2018.jpg|frameless| | [[File:Plantar fasciotomy evidence Gibbons 2018.jpg|frameless|500x500px|alt=]] | ||
'''Figure 28'''. Long-term outcomes following plantar fasciotomy <ref name=":7" /><ref name=":34" /> | '''Figure 28'''. Long-term outcomes following plantar fasciotomy <ref name=":7" /><ref name=":34" /> | ||
Revision as of 17:33, 5 August 2021
Original Editor - Merinda Rodseth based on the course by
Bernice Saban
Top Contributors - Merinda Rodseth, Kim Jackson, Jess Bell and Tarina van der Stockt
Introduction[edit | edit source]
Plantar heel pain (PHP) is regarded as a multifactorial condition with many factors proposed to be associated with it [1][2]. PHP is generally viewed as a self-limiting condition and for the majority of individuals with PHP, the symptoms resolve within one year without any therapeutic intervention [1][3][4]. Twenty percent of individuals, however, continue to experience PHP beyond a year [1][3]. The aetiology of PHP is generally not well understood which causes uncertainty regarding the most effective management thereof, making the condition difficult to effectively treat [1][2]. Combined with this, there is also a lack of high quality evidence regarding optimal treatment which leaves clinicians with a variety of treatment options but no clear evidence on what works best and no firm, evidence-based clinical advice on the optimal management of PHP [3][4][5][6][7][8].
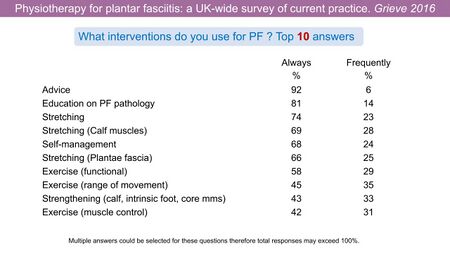
With no clear guidance, Grieve et al [9] conducted a survey on which interventions Physiotherapists in the United Kingdom (UK) then use for PHP (Figure 1).
Figure 1. Interventions used by Physiotherapists in the UK for PHP [9][10]
This again highlights the need to search the available research to establish which treatment options are available and effective in the management of plantar heel pain syndrome (PHPS). When considering the research, it is important to keep in mind that the term “significant difference” is a statistical value and not always reflective of a difference/change that would be meaningful for the patient. It is therefore also important to consider the “Minimal important difference” (Minimal clinically important difference/change) or the “smallest change in treatment outcome that an individual patient would identify as important, and which would mandate a change in the patient’s management” [10][11].
Which treatments should then be used for patients with PHPS? The following physiotherapy and medical treatments will be discussed in this review, with the aim of identifying treatment options supported by high-quality research studies (Figure 2).
Figure 2. Treatment options proposed for PHPS [10]
Physiotherapy Treatments[edit | edit source]
A large variety of physiotherapy treatment options for PHPS have been discussed in the literature and will be reviewed in the following section (Figure 3).
Figure 3. Physiotherapy treatment options proposed for PHPS [10]
Ultrasound[edit | edit source]
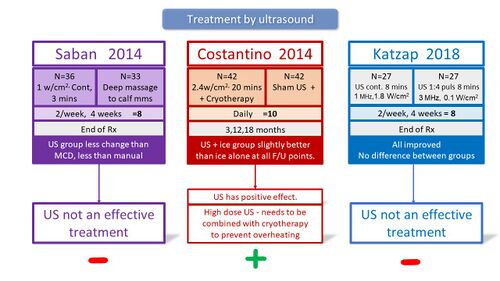
Therapeutic ultrasound is one of the most widely used electrical devices among physiotherapists worldwide even without the support of sufficient high-quality evidence for its use in musculoskeletal conditions [12]. Many studies investigated the use of ultrasound and found therapeutic ultrasound to be ineffective for the treatment of PHP and its use is therefore not recommended for individuals with PHPS (Figure 4) [12][13][14][15][16].
Figure 4. Studies investigating the treatment of PHP by ultrasound
Stretching[edit | edit source]
Stretching of the triceps surae muscles has been proposed in many studies as an essential part of the management of plantar fasciitis [12]. The aim of stretching is to release tension in the Achilles tendon and plantar fascia, both of which attach to the calcaneus [12]. Many studies have investigated the use of stretching for the treatment of PHPS, often with conflicting results. Several studies compared the use of various stretches for PHPS and generally found that all groups improved with Barry et al [17] also reporting a shorter recovery time with the use of night splinting (Figure 5) [17][18][19].
Figure 5. Research studies comparing various stretching regimes [10][17][18][19]
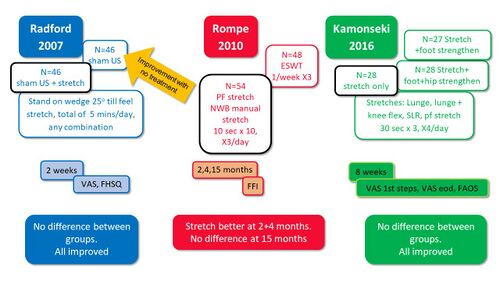
Some studies compared stretching to various other treatment interventions (sham US, ESWT, strengthening) and generally found no differences between groups, that all groups improved. Stretching was thereby not superior to other forms of treatment (Figure 6) [20][21][22].
Figure 6. Stretching compared to other forms of treatment [10][20][21][22]
In a systematic review analysing the effectiveness of manual stretching for PHPS, Sweeting et al [23] reported:
- Conflicting results
- One study showed placebo to be equally effective to stretching
- Another study showed stretch to be more effective than EWST
- Intermittent or sustained methods of stretching were equally effective
- Plantar fascia NWB stretch could be more effective than dorsiflexion WB stretch
Strengthening[edit | edit source]
Weakness of the intrinsic foot muscles as well as the ankle plantar flexors have been proposed as risk factors for the development of PHPS and prompted the use of strengthening as a treatment for PHPS [8]. Several studies investigated the effect of strengthening on PHPS and reported improvement in all groups with no advantage to strengthening in the management of PHPS, except after 3 months of plantar-specific stretching (Figure 6) [22][24].
Figure 6. Effect of strengthening on PHPS [10][22][24]
Manual Therapy[edit | edit source]
Physiotherapists often use manual therapy to improve joint mobility, mobilise soft tissue and reduce pain [25][26]. Current literature on the use of manual therapy for patients with PHP is however sparse and often of lesser quality [25]. Cleland et al [27] conducted a study on the efficacy of manual therapy and exercise (MTEX) compared to electro-physical agents and exercise (EPAX) in the management of PHPS (Figure 7). Both treatment groups however, received multiple different interventions which is problematic for interpreting which intervention made the difference (Figure 8). They concluded that all patients improved with statistically significant differences between groups regarding pain and global improvement favouring MTEX (Figure 9) [27]. There is however not enough information about the clinical effects of the treatment.
Figure 7. Manual therapy and exercise compared to Electro-physical agents and exercise for PHPS [10][27]
Figure 8. Treatment details of the groups in the study by Cleland et al [27][10]
Figure 9. Results of the comparison between Manual therapy and electro-physical agents for PHPS [10][27]
Shashua et al [28] also investigated the effect of manual therapy on plantar fasciitis (Figure 10) with the treatment group receiving manual therapy, ultrasound and stretch exercises and the control group only ultrasound and stretch exercises (Figure 11). They reported an improvement in both groups with no difference between groups, indicating no additional advantage to manual therapy for PHPS (Figure 12)[28].
Figure 10. Manual therapy for Plantar fasciitis [10][28]
Figure 11. Treatment details for both groups in the study by Shashua et al [28][10]
Figure 12. Results on the effect of manual therapy for plantar fasciitis [10][28]
Taping[edit | edit source]
Taping is proposed to be associated with pain reduction, increased circulation and improved proprioception, all of which would be beneficial for the management of PHPS [29]. Radford et al [30] applied standardised leukotape to the plantar skin of patients and kept it in situ for 7 days, which they compared to a control group. Both groups improved and there was no significant reduction in heel pain intensity in the taping group compared to the controls [3][30]. First step pain, however, was significantly better in the taping group compared to the controls (Figure 13) [30].
Figure 13. Effectiveness of low-Dye taping for the treatment of PHPS [10][30]
Tsai et al [29] compared the use of kinesiotape for plantar fasciitis, applied over the gastrocnemius and plantar fascia and kept in situ for one week, to a control group (Figure 14). Both groups reported a significant reduction in pain and there was a significant difference in pain reduction between the groups, but this was also reported before intervention. No differences in plantar fascia thickness were found between groups [29]. This study, however, had insufficient information to accurately interpret its measurements and come to a final conclusion about the treatment effects (Figure 15) [10].
Figure 14. Kinesiotaping versus control group [10][29]
Figure 15. Results of the study by Tsai et al [29][10]
Dry Needling[edit | edit source]
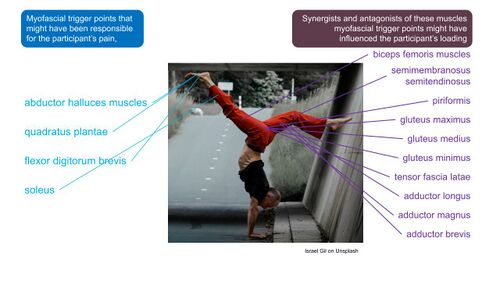
The presence of myofascial trigger points within the musculature of the plantar foot as well as the muscles proximal to the foot, has been proposed to play a role in PHPS [31]. Dry needling of these myofascial trigger points has therefore been proposed for the management of plantar fasciitis [31][32][33]. Limited evidence for the effectiveness of dry needling was however reported in a systematic review on dry needling for PHPS and the poor quality of the studies precluded making definite conclusions [33]. Following this, Cotchett et al [31] conducted a study to determine the efficacy of trigger point dry needling for PHPS (Figure 16) and compared “real dry needling” into the myofascial trigger points of a variety of muscles (Figure 17) to sham dry needling. They found that even though real dry needling provided statistically significant reductions in PHP compared to sham dry needling, the size of the effect was not clinically meaningful (Figure 18) [31].
Figure 16. Effectiveness of trigger point dry needling for PHPS [10][31]
Figure 17. Different muscles in which trigger points were dry needled [10][31]
Figure 18. Outcome of real vs sham dry needling [10][31]
Cryotherapy[edit | edit source]
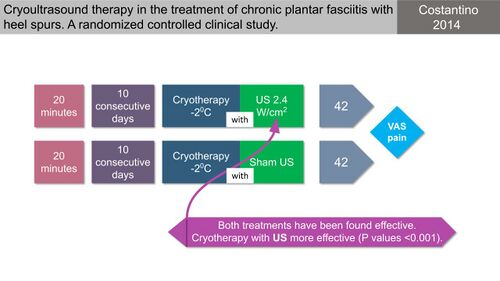
Ice/cryotherapy is generally considered as a basic component in the management of any injury due to its proposed effectiveness in reducing swelling and relieving short-term pain [15]. It has thereby also been proposed as a treatment option for PHP as for many other musculoskeletal conditions [15][26]. Costantino et al [15] conducted a study comparing cryoultrasound to only cryotherapy and found that all patients improved but the ultrasound group showed a larger improvement (Figure 19).
Figure 19. Cryoultrasound vs cryotherapy for chronic plantar fasciitis [10][15]
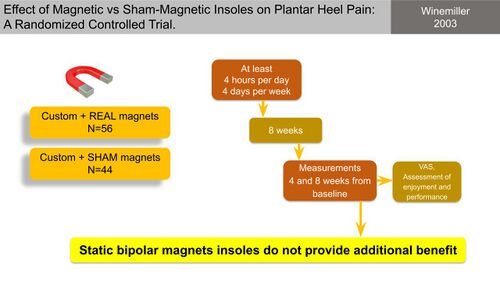
Medical Treatments[edit | edit source]
Varying between countries and depending on the scope of practice, many of the following treatments are often not performed by physiotherapists but rather medical doctors, and mostly used after failure of conservative management (Figure 20).
Figure 20. Proposed medical treatments for the management of PHPS [10]
Orthotics[edit | edit source]
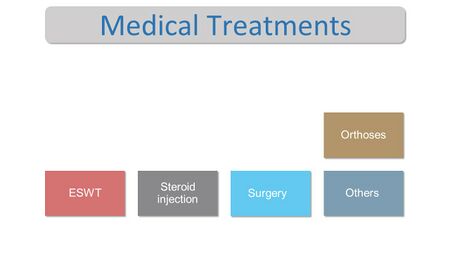
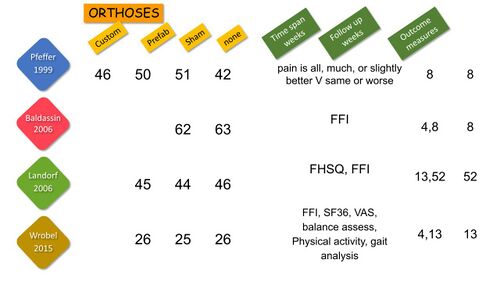
Four high quality studies investigating the effect of a variety of foot orthoses/insoles in PHPS were identified (Figure 21 and Figure 22) [10]. They provided varied and somewhat conflicting results on the efficacy of various insoles for PHPS and generally reported improvement in all groups with no consistent benefit to any one orthosis (Figure 23) [6][34][35][36][37].
Figure 21. Good quality studies on the use of orthoses/insoles for PHPS [10]
Figure 22. Study details of the four studies on orthoses for PHPS [10][34][35][36][37]
Figure 23. Results on the most effective insole for PHPS [10]
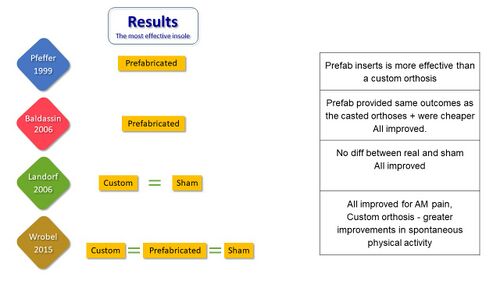
Winemiller et al [38] compared the effect of magnetic versus sham-magnetic insoles on PHP and found no benefit to magnetic insoles compared to sham-magnetic inserts (Figure 24).
Figure 24. Magnetic insoles vs sham-magnetic insoles for PHP [10][38]
Extracorporeal Shock Wave Therapy[edit | edit source]
Extracorporeal shock wave therapy (ESWT) has been used since 1976 to disintegrate kidney and gallstones (lithotripsy) and for several decades as a non-invasive pain-relief treatment option for failed conservative management of plantar fasciitis before surgical intervention [26][39]. ESWT involves an electromagnetic system where a magnetic field in a surrounding fluid medium is used to produce shock waves [26]. Abrupt, high-amplitude pulses of mechanical energy (similar to sound waves) are generated by an electromagnetic coil or a spark in water [10]. The shock waves are proposed to stimulate angiogenesis (new blood vessels) and neurogenesis (new nerve cells) [10]. Its mechanism of action is still not well understood but proposed to be through the destruction of unmyelinated nerve fibres with simultaneous stimulation of neovascularisation and collagen synthesis [26]. The cells therefore appear to undergo micro trauma which promotes the inflammatory and catabolic processes associated with the removal of damaged matrix waste and stimulation of wound healing mechanisms [10]. In short, ESWT should:[10]
- Increase blood supply
- Improve collagen remodelling
- Enhance waste elimination
Several studies, many of poor methodological quality, explored the effect of ESWT on PHPS with conflicting results (Figure 25).
Figure 25. Evidence for the use of ESWT in PHPS [10][39][40][41][42][43][44]
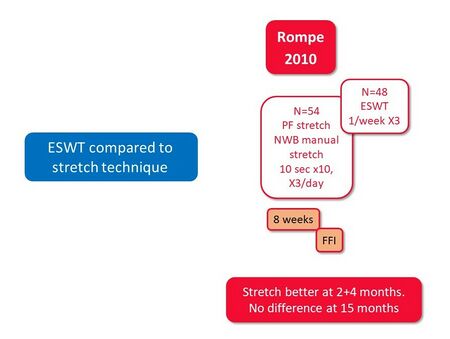
Of the studies reviewed, only Gerdesmeyer et al [40] reported a significant improvement in pain, function and quality of life with ESWT whereas others had conflicting results. Rompe et al [21] compared ESWT to stretching techniques and found stretching to be more advantageous than ESWT at 2 and 4 months (Figure 26).
Figure 26. ESWT compared to a stretching regime for PHPS [10][21]
Following the results of their systematic review, Yu et al [45] reported inconsistent evidence on the effectiveness of ESWT for PHPS and stated that the current evidence does not support the use of ESWT for PHPS.
Steroid Injections[edit | edit source]
Corticosteroid injections are used in multiple musculoskeletal conditions, including PHP, as a way of relieving pain [26][46]. In a Cochrane review, David et al [46] reported low quality evidence that local steroid injections may slightly reduce PHP for up to one month, compared to placebo or no treatment (Figure 27).
Figure 27. Cochrane review of injected corticosteroids for the treatment of PHP [10][46]
Surgery[edit | edit source]
Surgical interventions are generally not considered for plantar fasciitis until conservative treatment has been thoroughly pursued and symptoms have been present for more than 6 months [47]. Plantar fasciotomy will only be considered if conservative therapies have been ineffective and significant symptoms continue to persist [47]. Plantar fasciotomy involves: [47]
- an open procedure
- either a partial release of the medial one-third of the plantar fascia
- or a complete release of the fascia
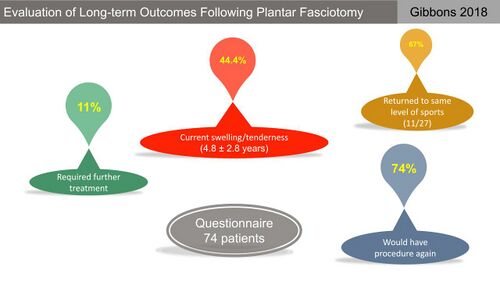
The outcomes following plantar fasciotomy vary but generally shows good early pain relief and return to function in the short term [47]. Many individuals however experience ongoing pain and functional limitations and a retrospective study by Gibbons et al [47] demonstrated that even though 72% of patients reported long-term satisfaction with the surgery, 44% continued to experience ongoing pain, swelling and tenderness (Figure 28).
Figure 28. Long-term outcomes following plantar fasciotomy [10][47]
Conclusion[edit | edit source]
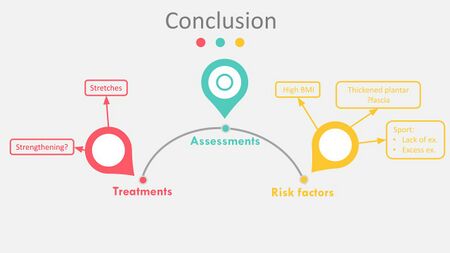
From the literature explored it seems that stretches could possibly help for PHPS and strengthening may be beneficial but the available evidence does not support any of the commonly used treatments for PHP as significantly better than any other [4][13]. At the moment there is limited evidence upon which to base clinical practice [48] which poses a professional spur for clinicians as it relates to the risk factors, assessment and management of PHPS.
From the literature reviews on these topics in PHPS, there is some information on the risk factors associated with PHPS, no evidence for the assessment of PHPS and very little information on the management thereof (Figure 29) which prompts us to the next lecture in the series, the pursuing of a new protocol for PHPS [10].
Figure 29. Known variables from the literature reviews on risk factors, assessment and treatment of PHPS [10]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Sullivan J, Pappas E, Burns J. Role of mechanical factors in the clinical presentation of plantar heel pain: implications for management. The Foot. 2020 Mar 1;42:101636. DOI:10.1016/j.foot.2019.08.007
- ↑ 2.0 2.1 Thomas MJ, Whittle R, Menz HB, Rathod-Mistry T, Marshall M, Roddy E. Plantar heel pain in middle-aged and older adults: population prevalence, associations with health status and lifestyle factors, and frequency of healthcare use. BMC musculoskeletal disorders. 2019 Dec;20(1):1-8.
- ↑ 3.0 3.1 3.2 3.3 Salvioli S, Guidi M, Marcotulli G. The effectiveness of conservative, non-pharmacological treatment, of plantar heel pain: a systematic review with meta-analysis. The Foot. 2017 Dec 1;33:57-67.
- ↑ 4.0 4.1 4.2 Babatunde OO, Legha A, Littlewood C, Chesterton LS, Thomas MJ, Menz HB, van der Windt D, Roddy E. Comparative effectiveness of treatment options for plantar heel pain: a systematic review with network meta-analysis. British journal of sports medicine. 2019 Feb 1;53(3):182-94.
- ↑ Morrissey D, Cotchett M, J'Bari AS, Prior T, Griffiths IB, Rathleff MS, Gulle H, Vicenzino B, Barton CJ. Management of plantar heel pain: a best practice guide informed by a systematic review, expert clinical reasoning and patient values. British Journal of Sports Medicine. 2021 Mar 30.
- ↑ 6.0 6.1 Rasenberg N, Bierma-Zeinstra SM, Bindels PJ, van der Lei J, van Middelkoop M. Incidence, prevalence, and management of plantar heel pain: a retrospective cohort study in Dutch primary care. British Journal of General Practice. 2019 Nov 1;69(688):e801-8.
- ↑ Whittaker GA, Landorf KB, Munteanu SE, Menz HB. Predictors of response to foot orthoses and corticosteroid injection for plantar heel pain. Journal of Foot and Ankle Research. 2020 Dec;13(1):1-9.
- ↑ 8.0 8.1 Franettovich Smith MM, Collins NJ, Mellor R, Grimaldi A, Elliott J, Hoggarth M, Weber Ii KA, Vicenzino B. Foot exercise plus education versus wait and see for the treatment of plantar heel pain (FEET trial): a protocol for a feasibility study. Journal of foot and ankle research. 2020 Dec;13:1-4. DOI: 10.1186/s13047-020-00384-1
- ↑ 9.0 9.1 Grieve R, Palmer S. Physiotherapy for plantar fasciitis: a UK-wide survey of current practice. Physiotherapy. 2017 Jun 1;103(2):193-200.
- ↑ 10.00 10.01 10.02 10.03 10.04 10.05 10.06 10.07 10.08 10.09 10.10 10.11 10.12 10.13 10.14 10.15 10.16 10.17 10.18 10.19 10.20 10.21 10.22 10.23 10.24 10.25 10.26 10.27 10.28 10.29 10.30 10.31 10.32 10.33 10.34 10.35 10.36 Bernice Saban 2021.Treatment of Plantar Heel Pain - A Literature Review. Physioplus Course. 2021
- ↑ Cotchett M, Rathleff MS, Dilnot M, Landorf KB, Morrissey D, Barton C. Lived experience and attitudes of people with plantar heel pain: a qualitative exploration. Journal of foot and ankle research. 2020 Dec;13(1):1-9.
- ↑ 12.0 12.1 12.2 12.3 Katzap Y, Haidukov M, Berland OM, Itzhak RB, Kalichman L. Additive effect of therapeutic ultrasound in the treatment of plantar fasciitis: a randomized controlled trial. Journal of Orthopaedic & Sports Physical Therapy. 2018 Nov;48(11):847-55.
- ↑ 13.0 13.1 Martin RL, Davenport TE, Reischl SF, McPoil TG, Matheson JW, Wukich DK, McDonough CM, Altman RD, Beattie P, Cornwall M, Davis I. Heel pain—plantar fasciitis: revision 2014. Journal of Orthopaedic & Sports Physical Therapy. 2014 Nov;44(11):A1-33.
- ↑ Saban B, Deutscher D, Ziv T. Deep massage to posterior calf muscles in combination with neural mobilization exercises as a treatment for heel pain: a pilot randomized clinical trial. Manual therapy. 2014 Apr 1;19(2):102-8.
- ↑ 15.0 15.1 15.2 15.3 15.4 Costantino C, Vulpiani MC, Romiti D, Vetrano M, Saraceni VM. Cryoultrasound therapy in the treatment of chronic plantar fasciitis with heel spurs. A randomized controlled clinical study. Eur J Phys Rehabil Med. 2014 Feb 1;50(1):39-47.
- ↑ Shanks P, Curran M, Fletcher P, Thompson R. The effectiveness of therapeutic ultrasound for musculoskeletal conditions of the lower limb: A literature review. The Foot. 2010 Dec 1;20(4):133-9.
- ↑ 17.0 17.1 17.2 Barry LD, Barry AN, Chen Y. A retrospective study of standing gastrocnemius-soleus stretching versus night splinting in the treatment of plantar fasciitis. The Journal of foot and ankle surgery. 2002 Jul 1;41(4):221-7.
- ↑ 18.0 18.1 DiGiovanni BF, Nawoczenski DA, Malay DP, Graci PA, Williams TT, Wilding GE, Baumhauer JF. Plantar fascia-specific stretching exercise improves outcomes in patients with chronic plantar fasciitis: a prospective clinical trial with two-year follow-up. JBJS. 2006 Aug 1;88(8):1775-81.
- ↑ 19.0 19.1 Porter D, Barrill E, Oneacre K, May BD. The effects of duration and frequency of Achilles tendon stretching on dorsiflexion and outcome in painful heel syndrome: a randomized, blinded, control study. Foot & ankle international. 2002 Jul;23(7):619-24.
- ↑ 20.0 20.1 Radford JA, Landorf KB, Buchbinder R, Cook C. Effectiveness of calf muscle stretching for the short-term treatment of plantar heel pain: a randomised trial. BMC musculoskeletal disorders. 2007 Dec;8(1):1-8.
- ↑ 21.0 21.1 21.2 21.3 Rompe JD, Cacchio A, Weil Jr L, Furia JP, Haist J, Reiners V, Schmitz C, Maffulli N. Plantar fascia-specific stretching versus radial shock-wave therapy as initial treatment of plantar fasciopathy. JBJS. 2010 Nov 3;92(15):2514-22.
- ↑ 22.0 22.1 22.2 22.3 Kamonseki DH, Gonçalves GA, Liu CY, Júnior IL. Effect of stretching with and without muscle strengthening exercises for the foot and hip in patients with plantar fasciitis: a randomized controlled single-blind clinical trial. Manual therapy. 2016 Jun 1;23:76-82.
- ↑ Sweeting D, Parish B, Hooper L, Chester R. The effectiveness of manual stretching in the treatment of plantar heel pain: a systematic review. Journal of foot and ankle research. 2011 Dec;4(1):1-3.
- ↑ 24.0 24.1 Rathleff MS, Mølgaard CM, Fredberg U, Kaalund S, Andersen KB, Jensen TT, Aaskov S, Olesen JL. High‐load strength training improves outcome in patients with plantar fasciitis: A randomized controlled trial with 12‐month follow‐up. Scandinavian journal of medicine & science in sports. 2015 Jun;25(3):e292-300.
- ↑ 25.0 25.1 Mischke JJ, Jayaseelan DJ, Sault JD, Emerson Kavchak AJ. The symptomatic and functional effects of manual physical therapy on plantar heel pain: a systematic review. Journal of Manual & Manipulative Therapy. 2017 Jan 1;25(1):3-10.
- ↑ 26.0 26.1 26.2 26.3 26.4 26.5 Hasegawa M, Urits I, Orhurhu V, Orhurhu MS, Brinkman J, Giacomazzi S, Foster L, Manchikanti L, Kaye AD, Kaye RJ, Viswanath O. Current concepts of minimally invasive treatment options for plantar fasciitis: A comprehensive review. Current Pain and Headache Reports. 2020 Sep;24(9):1-1.
- ↑ 27.0 27.1 27.2 27.3 27.4 Cleland JA, Abbott JH, Kidd MO, Stockwell S, Cheney S, Gerrard DF, Flynn TW. Manual physical therapy and exercise versus electrophysical agents and exercise in the management of plantar heel pain: a multicenter randomized clinical trial. journal of orthopaedic & sports physical therapy. 2009 Aug;39(8):573-85.
- ↑ 28.0 28.1 28.2 28.3 28.4 Shashua A, Flechter S, Avidan L, Ofir D, Melayev A, Kalichman L. The effect of additional ankle and midfoot mobilizations on plantar fasciitis: a randomized controlled trial. Journal of Orthopaedic & Sports Physical Therapy. 2015 Apr;45(4):265-72.
- ↑ 29.0 29.1 29.2 29.3 29.4 Tsai CT, Chang WD, Lee JP. Effects of short-term treatment with kinesiotaping for plantar fasciitis. Journal of Musculoskeletal Pain. 2010 Jan 1;18(1):71-80.
- ↑ 30.0 30.1 30.2 30.3 Radford JA, Landorf KB, Buchbinder R, Cook C. Effectiveness of low-Dye taping for the short-term treatment of plantar heel pain: a randomised trial. BMC musculoskeletal disorders. 2006 Dec;7(1):1-7.
- ↑ 31.0 31.1 31.2 31.3 31.4 31.5 31.6 Cotchett MP, Munteanu SE, Landorf KB. Effectiveness of trigger point dry needling for plantar heel pain: a randomized controlled trial. Physical therapy. 2014 Aug 1;94(8):1083-94.
- ↑ Llurda-Almuzara L, Labata-Lezaun N, Meca-Rivera T, Navarro-Santana MJ, Cleland JA, Fernández-de-Las-Peñas C, Pérez-Bellmunt A. Is Dry Needling Effective for the Management of Plantar Heel Pain or Plantar Fasciitis? An Updated Systematic Review and Meta-analysis. Pain Medicine. 2021 Mar 24.
- ↑ 33.0 33.1 Cotchett MP, Landorf KB, Munteanu SE. Effectiveness of dry needling and injections of myofascial trigger points associated with plantar heel pain: a systematic review. Journal of foot and ankle research. 2010 Dec;3(1):1-9.
- ↑ 34.0 34.1 Pfeffer G, Bacchetti P, Deland J, Lewis AI, Anderson R, Davis W, Alvarez R, Brodsky J, Cooper P, Frey C, Herhck R. Comparison of custom and prefabricated orthoses in the initial treatment of proximal plantar fasciitis. Foot & Ankle International. 1999 Apr;20(4):214-21.
- ↑ 35.0 35.1 Landorf KB, Keenan AM, Herbert RD. Effectiveness of foot orthoses to treat plantar fasciitis: a randomized trial. Archives of internal medicine. 2006 Jun 26;166(12):1305-10.
- ↑ 36.0 36.1 Baldassin V, Gomes CR, Beraldo PS. Effectiveness of prefabricated and customized foot orthoses made from low-cost foam for noncomplicated plantar fasciitis: a randomized controlled trial. Archives of physical medicine and rehabilitation. 2009 Apr 1;90(4):701-6.
- ↑ 37.0 37.1 Wrobel JS, Fleischer AE, Crews RT, Jarrett B, Najafi B. A randomized controlled trial of custom foot orthoses for the treatment of plantar heel pain. Journal of the American Podiatric Medical Association. 2015 Jul;105(4):281-94.
- ↑ 38.0 38.1 Winemiller MH, Billow RG, Laskowski ER, Harmsen WS. Effect of magnetic vs sham-magnetic insoles on plantar heel pain: a randomized controlled trial. Jama. 2003 Sep 17;290(11):1474-8.
- ↑ 39.0 39.1 Buchbinder R, Ptasznik R, Gordon J, Buchanan J, Prabaharan V, Forbes A. Ultrasound-guided extracorporeal shock wave therapy for plantar fasciitis: a randomized controlled trial. Jama. 2002 Sep 18;288(11):1364-72.
- ↑ 40.0 40.1 Gerdesmeyer L, Frey C, Vester J, Maier M, Lowell Jr W, Weil Sr L, Russlies M, Stienstra J, Scurran B, Fedder K, Diehl P. Radial extracorporeal shock wave therapy is safe and effective in the treatment of chronic recalcitrant plantar fasciitis: results of a confirmatory randomized placebo-controlled multicenter study. The American journal of sports medicine. 2008 Nov;36(11):2100-9.
- ↑ Haake M, Buch M, Schoellner C, Goebel F, Vogel M, Mueller I, Hausdorf J, Zamzow K, Schade-Brittinger C, Mueller HH. Extracorporeal shock wave therapy for plantar fasciitis: randomised controlled multicentre trial. Bmj. 2003 Jul 10;327(7406):75.
- ↑ Kudo P, Dainty K, Clarfield M, Coughlin L, Lavoie P, Lebrun C. Randomized, placebo‐controlled, double‐blind clinical trial evaluating the treatment of plantar fasciitis with an extracoporeal shockwave therapy (ESWT) device: A North American confirmatory study. Journal of orthopaedic research. 2006 Feb;24(2):115-23.
- ↑ Malay DS, Pressman MM, Assili A, Kline JT, York S, Buren B, Heyman ER, Borowsky P, LeMay C. Extracorporeal shockwave therapy versus placebo for the treatment of chronic proximal plantar fasciitis: results of a randomized, placebo-controlled, double-blinded, multicenter intervention trial. The Journal of foot and ankle surgery. 2006 Jul 1;45(4):196-210.
- ↑ Speed CA, Nichols D, Wies J, Humphreys H, Richards C, Burnet S, Hazleman BL. Extracorporeal shock wave therapy for plantar fasciitis. A double blind randomised controlled trial. Journal of Orthopaedic Research. 2003 Sep;21(5):937-40.
- ↑ Yu H, Randhawa K, Côté P, Optima Collaboration. The effectiveness of physical agents for lower-limb soft tissue injuries: A systematic review. Journal of Orthopaedic & Sports Physical Therapy. 2016 Jul;46(7):523-54.
- ↑ 46.0 46.1 46.2 David JA, Sankarapandian V, Christopher PR, Chatterjee A, Macaden AS. Injected corticosteroids for treating plantar heel pain in adults. Cochrane Database of Systematic Reviews. 2017(6). CD009348.
- ↑ 47.0 47.1 47.2 47.3 47.4 47.5 Gibbons R, Mackie KE, Beveridge T, Hince D, Ammon P. Evaluation of long-term outcomes following plantar fasciotomy. Foot & ankle international. 2018 Nov;39(11):1312-9.
- ↑ Crawford F, Thomson CE. Interventions for treating plantar heel pain. Cochrane Database of Systematic Reviews. 2003(3).