Trapezius Myalgia
Original Editor - Lauren Trehout
Top Contributors - Nick Van Doorsselaer, Lauren Trehout, Abbey Wright, Elien Clerix, Camille Dewaele, Gayatri Jadav Upadhyay, Kim Jackson, Vanessa Rhule, Admin, Joao Costa, Rachael Lowe, Aminat Abolade, Rishika Babburu, Ajay Upadhyay, Kai A. Sigel and Kirenga Bamurange Liliane
Definition/Description[edit | edit source]
Myalgia is generally known as muscle ache or muscle pain.
Trapezius myalgia (TM) is the complaint of pain, stiffness and tightness of the upper trapezius muscle. It is characterised by acute or persistent neck-shoulder pain.[1]
TM is not a medical disorder or disease but rather a symptom of an existing underlying condition. The pain in the muscle can last a few days or longer.
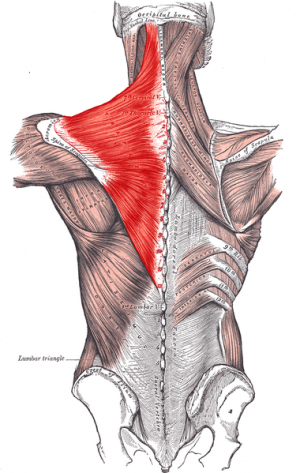
Clinically Relevant Anatomy[edit | edit source]
Trapezius is a large fan shaped muscle that extends from the cervical to thoracic region on the posterior aspect of the neck and trunk and attaches onto the clavicle and scapula.[2]
It consists of three parts with different actions:
- Superior fibres of Trapezius - elevates the shoulder girdle.
- Middle fibres of Trapezius - retracts the scapula
- Inferior fibres of Trapezius - depresses the scapula
Typically the area of pain involved with TM is the superior fibres of trapezius.
Aetiology/Epidemiology [edit | edit source]
Monotonous jobs with highly repetitive work, forceful exertions, high level of static contractions, prolonged static loads, constrained work postures or a combination of these factors are possible causes of neck and shoulder disorders (which include TM) in the working population. [3]
More research is required to conclude that computer work alone increases the risk of developing musculoskeletal disorders. [4]
As recent research suggests with most muscloskeletal coniditions there is a strong relationship between psycho-social factors and the occurrence of TM. There is some evidence that there is a link between TM and other social issues such as: lack of support from colleagues, mental stress at work and low influence.[5]
Epidemiology[edit | edit source]
Persistent TM concerns 10-20% of the 20% of the adult population with severe chronic pain in the neck and shoulder region. [6] The persistent form of TM also shows a higher prevalence in women, but also in low income groups. [7]
Gender seems to play an important role in the development of neck disorders, since the prevalence is much higher among women. Women more often experience neck pain and develop persistent pain than men do. This difference might be explained by the content of their jobs. Women’s work tasks involve more static load on the neck muscles, high repetitiveness, low control and high mental demands, which are all risk factors for developing neck disorders.[7]
Characteristics/Clinical Presentation[edit | edit source]
Typical symptoms of “myalgia” are:
- Sudden onset of pain[1]
- Muscle stiffness and spasms[1]
- Tightness of the neck-shoulder complex[1]
- Heaviness of the head and occipital headache
- Tenderness of the upper trapezius area[1]
Other symptoms:
- Low mood
- Anxiety
- Paresthesia
Persistent TM can cause pain and stiffness after periods of inactivity. The pain usually eases after reasonable exercise.[8]
Differential Diagnosis[edit | edit source]
TM can be diagnosed when neck pain, muscle tightness and trigger points are present, but tension neck syndrome or cervical syndrome is not present.[3]
Other pathologies that can cause similar symptoms are:
- Cervical spondylosis[9]
- Cervical osteoarthritis
- Cervical radiculopathy
- Thoracic Outlet Syndrome
- Shoulder pathology - including rotator cuff pathology and shoulder osteoarthritis[10]
- Polymyaglia rheumatica[10]
Diagnostic Procedures[edit | edit source]
The basis for diagnostic criteria of neck and shoulder myalgia is not very clear and the diagnostic terminology and methods for assessment are variable.[3]
- Thorough subjective assessment
- Objective assessment - including neurological exam, and shoulder assessment
- Imaging studies - can be useful if no improvement in symptoms, neurological symptoms or if red flags present[9]
- Use of diagnostic injections (if qualified to do so)[9]
- Referral to orthopaedic consultant if no improvement in symptoms with conservative management[10]
In general, no objective diagnostic methods are available specifically for TM. The diagnosis is mostly based on symptom presentation and history of illness.
Outcome measures[edit | edit source]
Visual analogue scale[8]
This scale measures visualises to what extend the patient experiences pain or another sensation. It is a 100mm line on which the patient need to draw a perpendicular line to indicate how he experiences pain. On the left is the minimum score of 0 meaning ‘no pain’ and on the right, stands the maximus score of 10, which means ‘unbearable pain’.
McGill pain questionnaire (MPQ)[11] [12] [13]
The MPQ is a subjective questionnaire used to asses the quality and intensity of pain in patients with a number of diagnoses.
Neck disability index (NDI) [14][15] [13]
The NDI is a questionnaire that inquires the functional status of a patient concern the following 10 items: pain, personal care, lifting, reading, headaches, concentration, work, driving, sleeping and recreation.
Neck Bournemouth Questionnaire (NBQ)[16] [15] [13]
The NBQ is administered to patients with non-specific neck pain. It assesses pain, disability, effective and cognitive aspects of the neck pain. The questionnaire contains seven items: pain intensity, function in activities of daily living, function in social activities, anxiety, depression levels and fear avoidance behaviour. The NBQ has been shown to be reliable, valid, and responsive to clinically significant change in patients with non-specific neck pain.[16]
Examination[edit | edit source]
Subjective assessment is vital in assessing the condition history, potential cause and severity. It is also necessary in order to assess the patient's outlook and mental well being, which is a good indicator for prognosis and recovery in all types of injury or illness.[17]
Outcome measures can be used at the initial assessment to indicate severity and impact on the patient's well being and quality of life (as noted in the Outcome measures section).
Objective examination of the neck and upper extremities can be useful for diagnosing TM or exclude other pathologies. This should include:
- Cervical and shoulder range of movement (active and passive)
- Muscle strength
- Palpation
- Neurological exam [18]
Patients suffering from TM can present with neck pain, headaches, tightness of the trapezius muscle and palpable trigger points.[18] [19]
A surface electromyography can be done to evaluate muscle function. Parameters that can be studied are amplitude, timing, conduction velocity, fatigability and characteristic frequencies/patterns.[20]
Medical Management[edit | edit source]
Centrally a reorganisation of the neuromotor control strategies takes place. The superficial cervical extensor muscles show a higher muscle activation and deplete faster. So, the superficial upper trapezius shows a higher activation than the erector spinae. A greater recruitment of type II fibres in symptomatic patients could possibly explain the muscle fatigue.[21]
There is no specific medical management for TM. This is because either TM is caused by environmental reasons like stress, overuse, bad working position… or either it’s a side effect of different kinds of medication.
With medication, you can only treat the pain, but not the cause.
According to the review of Jensen et al most of the pharmacological treatments lack effects or haven’t enough evidence. An intra-muscular injection with lidocaine only has short term effect on pain in chronic neck pain. Intravenous methylprednisolone and lidocaine works in short term on pain. There is not enough evidence on the long term effects of surgical interventions. 24
Physical Therapy Management[edit | edit source]
Prevention
Electromyographical biofeedback training of the upper trapezius muscle might be useful in the prevention of TM in computer workers. Studies have found a positive relation between the amount of inactivity and neck disorders. Sedentary workers with low levels of leisure-time activity had a higher prevalence of neck disorders.From this we can conclude that it is important to be active after working hours.The biggest risk factors are:[22](LoE:1B)
- repetitive movements, gender (woman),
- high force demands,
- work posture,
- vibration,
- computer work and stress.
Information and advice
To prevent TM it’s important to inform people who are at risk about what they should or shouldn’t do. We need to advise them on which working position is the best and how to work at the computer.Stress is a big risk factor for developing trapezius myalgia. Therefor it should be a main focus in prevention and treating TM. With stress often comes muscle tension in the upper part of the trapezius. This should be avoided and decreased. Physical applications:There is moderate evidence available for short-term relief of mysfascial trigger points by Transcutaneous Electro Nerve Stimulation (TENS), acapuncture and magnet therapy. Laser therapy and acupuncture also show symptom relief of myofascial trigger points.The review of Chow et al. shows evidence of pain reduction in patients with acute or chronic neck pain after low-level laser therapy (wavelength: 780, 830 or 904 nm.[23][24](LoE:1A)
however there are other studies that say The quality of evidence ranged from very poor to poor in short term with acupuncture/dry needling having the largest effect size. There is no evidence of effective treatment to reduce pain in the intermediate and long term periods.[25](LoE:1A)
The RCT of Aguilera et al shows an immediate decrease in electrical activity in the trapezius muscle and a reduced sensitivity of myofascial trigger points after ultrasound treatment. The review of Vernon & Schneider show however that there’s conflicting evidence (level C) as to whether ultrasound therapy is no more effective than placebo or somewhat more effective than other therapies in the treatment of myofascial trigger points. Ultrasound can therefore be used as a therapeutic modulation, but is not recommended.
Biofeedback, earlier described as a prevention modality, can also be useful in the treatment of work related neck-and shoulder pain. The RCT of Ma et al. shows that six weeks of biofeedback training results in less pain and neck disability than active and passive treatment, which is remained at 6 months post intervention. They also found consistent trends of reduced muscle activity in the upper trapezius.[26][23](LoE:1B) (LoE:1A)
however there are other studies that say The quality of evidence ranged from very poor to poor in short term with acupuncture/dry needling. There is no evidence of effective treatment to reduce pain in the intermediate and long term periods for TM.[25](LoE:1A)
Manual therapies
Ischaemic compression, stretch of the upper trapezius muscle, transverse friction massage are manual techniques to help patients with TM. These techniques appear to have instant improvement on pain. Long-term effects have not yet been well investigated.The RCT of Aguilera et al. shows an immediate decrease in electrical activity in the trapezius muscle and an improvement of active ROM after ischaemic compression.According to Vernon & Schneider moderately strong evidence is available for immediate pain relief at trigger points due to spinal manipulation and ischemic compression.[23](LoE:1A)
Physical exercise
Different forms of exercise can be recommended for acute or persistent neck pain [27]
Physical activity and exercise have been proven to give the most immediate and long-term pain relief in patients with TM[28]. Both general fitness training and specific strength training generate significant effects on decreasing pain[29]. However strength training has proven to be even more effective compared to general fitness training. Following a specific neck strengthening exercise program a study showed that three years later the neck strength gains were consistent despite a similar NDI score to one year after completing the program. Therefore; pain and strength were maintained even after adherence to the exercise program faltered after the initial year.[30]
High-intensity strength training relying on principles of progressive overload for 20min can be successfully in reductions of neck and shoulder pain
[31] [32][33]
A study showed that general exercise is beneficial for TM pain. Especially specific strengthening exercises however it was also shown that general fitness exercise can reduce pain.[29]LoE:2B)
1. Shoulder shrugs:
The subject is standing erect and holding the dumbbells to the side, then elevates the shoulders while focusing on contracting the upper trapezius muscle.
2. One-arm row:
The subject is bending her torso forward to approximately 30° from horizontal with one knee on the bench and the other foot on the floor. The subject now pulls the dumbbell towards the ipsilateral lower rib, while the contralateral arm is maintained extended and supports the body on the bench.
3. Upright row:
The subject is standing erect and holding the dumbbells while the arms are hanging relaxed in front of the body. The dumbbells are lifted towards the chest in a vertical line close to the body while flexing the elbows and abducting the shoulder. The elbows are pointing out- and upwards.
4. Reverse flies:
The subject is lying on the chest at a 45° angle from horizontal and the arms pointing towards the floor. The dumbbells are raised until the upper arm is horizontally, while the elbows are in a static slightly flexed position (~5°) during the entire range of motion.
5. Lateral raise:
The subject is standing erect and holding the dumbbells side, and then abducts the shoulder joint until the upper arm is horizontally. The elbows are in a static slightly flexed position (5°) during the entire range of motion.
Exercise has been shown to increase blood flow and therefore oxygenation to areas of the body with increase anaerobic muscle metabolism. [35](LoE:2B)
Psychosocial involvement
The possible presence of psychosocial causative factors in patients with TM should be considered. If they are present, the patient should certainly be approached biopsychosocially.
Resources [edit | edit source]
Bournemouth Neck Questionnaire
Short form McGill pain questionnaire
Clinical Bottom Line[edit | edit source]
In a study of patients with and without pain but exposed to repetitive load such as desk work showed increased muscle fibre cross sectional areas - however it is unclear how this relates to pain.[36]
A EMG and doppler flowmetry study concluded that patient's with TM have impaired microcirculation in the upper traps which it is hypothesised can lead to nociceptive pain patterns.[37] A further EMG study in the non-painful population showed higher trapezius activity in the dominant hand and more trapezius activity in men than women.[7] Again after exercise in patients with pain EMG studies have shown nociceptive patterns (increased anaerobic metabolism) in comparison with a control group.[38] Trapezius biopsy also shows increase in inflammatory proteins compared with control group.[19]
Trapezius Myalgia is rather a symptom of an underlying existing problem than the problem itself and is often categorised in the neck and shoulder disorders. The typical symptoms of a patient with TM complaints are pain in the upper trapezius muscle that can linger for a few days to weeks. This pain is often associated with spasms, stiffness and tenderness in the neck region with radiation to the head and behind the eyes. Trigger points can also be present and can cause headaches. Both biomechanical and psychosocial factors can contribute to the development and maintenance of TM. It should be kept in mind that women suffer more frequently of TM than men do.
TM shouldn’t be confused with the tension neck syndrome, cervical syndrome, cervicalgia or thoracic outlet syndrome. To differentiate between these pathologies, the anamnesis and addition standard clinical examination on neck and upper extremities are very important. The use of a VAS for pain, a pressure algometer, a pain drawing and several questionnaires focused on pain and disabilities could help to evaluate the success of the treatment. Radiography, MRI, electromyography, nerve conductance testing or blood tests could be done to rule out other disorders, but aren’t standard procedures. The medical treatment consists of painkillers, which is the only medication which helps at short-term. The physiotherapist can apply TENS, dry needling, magnet therapy, laser therapy and ultrasound for short-term relief of the myofascial trigger points. Laser therapy, dry needling and biofeedback training can also result in a long-term effect. Biofeedback training is also a precautionary measure. Ischaemic compression and dry needling are manual techniques which could be used to relieve the pain of the trigger points immediately. Also stretch of the upper trapezius muscle and transverse friction massage are pain mitigation techniques. General fitness training appears to relieve pain immediately while 3 times a week 20 minutes’ specific strength training of the neck and shoulder musculature at an intensity of 70-85% relieves pain at long term. To avoid or cure TM it’s important to be active during the day and prevent overuse of the trapezius or stress.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 De Meulemeester K, Calders P, De Pauw R, Grymonpon I, Govaerts A, Cagnie B. Morphological and physiological differences in the upper trapezius muscle in patients with work-related trapezius myalgia compared to healthy controls: A systematic review. Musculoskeletal Science and Practice. 2017 Jun 1;29:43-51.
- ↑ Simons SM, Dixon JB. Physical examination of the shoulder. Up-To-Date Online. 2013 Nov.
- ↑ 3.0 3.1 3.2 Larsson B, Søgaard K, Rosendal L. Work related neck–shoulder pain: a review on magnitude, risk factors, biochemical characteristics, clinical picture and preventive interventions. Best Practice & Research Clinical Rheumatology. 2007 Jun 1;21(3):447-63.
- ↑ Wærsted M, Hanvold TN, Veiersted KB. Computer work and musculoskeletal disorders of the neck and upper extremity: a systematic review. BMC musculoskeletal disorders. 2010 Dec;11(1):79.
- ↑ Burton AK. Back injury and work loss: biomechanical and psychosocial influences. Spine. 1997 Nov 1;22(21):2575-80.
- ↑ Gerdle B, Ghafouri B, Ernberg M, Larsson B. Chronic musculoskeletal pain: review of mechanisms and biochemical biomarkers as assessed by the microdialysis technique. Journal of pain research. 2014;7:313.
- ↑ 7.0 7.1 7.2 Marker RJ, Balter JE, Nofsinger ML, Anton D, Fethke NB, Maluf KS. Upper trapezius muscle activity in healthy office workers: reliability and sensitivity of occupational exposure measures to differences in sex and hand dominance. Ergonomics. 2016 Sep 1;59(9):1205-14.
- ↑ 8.0 8.1 Waling K, Sundelin G, Ahlgren C, Järvholm B. Perceived pain before and after three exercise programs–a controlled clinical trial of women with work-related trapezius myalgia. Pain. 2000 Mar 1;85(1-2):201-7.
- ↑ 9.0 9.1 9.2 Pateder DB, Berg JH, Thal R. Neck and shoulder pain: differentiating cervical spine pathology from shoulder pathology. Journal of surgical orthopaedic advances. 2009;18(4):170-4.
- ↑ 10.0 10.1 10.2 Mitchell C, Adebajo A, Hay E, Carr A. Shoulder pain: diagnosis and management in primary care. BMJ: British Medical Journal. 2005 Nov 12;331(7525):1124.
- ↑ Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual analog scale for pain (vas pain), numeric rating scale for pain (nrs pain), mcgill pain questionnaire (mpq), short‐form mcgill pain questionnaire (sf‐mpq), chronic pain grade scale (cpgs), short form‐36 bodily pain scale (sf‐36 bps), and measure of intermittent and constant osteoarthritis pain (icoap). Arthritis care & research. 2011 Nov 1;63(S11):S240-52.
- ↑ Melzack R. The McGill Pain Questionnaire: major properties and scoring methods. Pain. 1975 Sep 1;1(3):277-99.
- ↑ 13.0 13.1 13.2 OHLSSON K, ATTEWELL RG, JOHNSSON B, AHLM A, Skerfving S. An assessment of neck and upper extremity disorders by questionnaire and clinical examination. Ergonomics. 1994 May 1;37(5):891-7.
- ↑ Macdermid JC, Walton DM, Avery S, Blanchard A, Etruw E, Mcalpine C, Goldsmith CH. Measurement properties of the neck disability index: a systematic review. Journal of orthopaedic & sports physical therapy. 2009 May;39(5):400-C12.
- ↑ 15.0 15.1 Gay RE, Madson TJ, Cieslak KR. Comparison of the Neck Disability Index and the Neck Bournemouth Questionnaire in a sample of patients with chronic uncomplicated neck pain. Journal of Manipulative and Physiological Therapeutics. 2007 May 1;30(4):259-62.
- ↑ 16.0 16.1 Bolton JE, Humphreys BK. The Bournemouth Questionnaire: a short-form comprehensive outcome measure. II. Psychometric properties in neck pain patients. Journal of manipulative and physiological therapeutics. 2002 Mar 1;25(3):141-8.
- ↑ Chida Y, Steptoe A. Positive psychological well-being and mortality: a quantitative review of prospective observational studies. Psychosomatic medicine. 2008 Sep 1;70(7):741-56.
- ↑ 18.0 18.1 Sjøgaard G, Søgaard K, Hermens HJ, Sandsjö L, Läubli T, Thorn S, Vollenbroek-Hutten MM, Sell L, Christensen H, Klipstein A, Kadefors R. Neuromuscular assessment in elderly workers with and without work related shoulder/neck trouble: the NEW-study design and physiological findings. European Journal of Applied Physiology. 2006 Jan 1;96(2):110-21.
- ↑ 19.0 19.1 Hadrevi J, Ghafouri B, Larsson B, Gerdle B, Hellström F. Multivariate modeling of proteins related to trapezius myalgia, a comparative study of female cleaners with or without pain. PLOS one. 2013 Sep 4;8(9):e73285.
- ↑ Castelein B, Cools A, Bostyn E, Delemarre J, Lemahieu T, Cagnie B. Analysis of scapular muscle EMG activity in patients with idiopathic neck pain: a systematic review. Journal of Electromyography and Kinesiology. 2015 Apr 1;25(2):371-86.
- ↑ Szeto GP, Straker LM, O’Sullivan PB. A comparison of symptomatic and asymptomatic office workers performing monotonous keyboard work—2: neck and shoulder kinematics. Manual therapy. 2005 Nov 1;10(4):281-91.
- ↑ Holtermann A, Søgaard K, Christensen H, Dahl B, Blangsted AK. The influence of biofeedback training on trapezius activity and rest during occupational computer work: a randomized controlled trial. European journal of applied physiology. 2008 Dec 1;104(6):983-9.(LoE:1B)
- ↑ 23.0 23.1 23.2 Vernon H, Schneider M. Chiropractic management of myofascial trigger points and myofascial pain syndrome: a systematic review of the literature. Journal of manipulative and physiological therapeutics. 2009 Jan 1;32(1):14-24. (LoE:1A)
- ↑ Chow RT, Johnson MI, Lopes-Martins RA, Bjordal JM. Efficacy of low-level laser therapy in the management of neck pain: a systematic review and meta-analysis of randomised placebo or active-treatment controlled trials. The Lancet. 2009 Dec 5;374(9705):1897-908.(LoE:1A)
- ↑ 25.0 25.1 Nunes AM, Moita JP. Effectiveness of physical and rehabilitation techniques in reducing pain in chronic trapezius myalgia: A systematic review and meta-analysis. International Journal of Osteopathic Medicine. 2015 Sep 30;18(3):189-206.
- ↑ Aguilera FJ, Martín DP, Masanet RA, Botella AC, Soler LB, Morell FB. Immediate effect of ultrasound and ischemic compression techniques for the treatment of trapezius latent myofascial trigger points in healthy subjects: a randomized controlled study. Journal of manipulative and physiological therapeutics. 2009 Sep 1;32(7):515-20. (LoE:1B)
- ↑ Jensen, IreneHarms-Ringdahl, Karin et al. Strategies for prevention and management of musculoskeletal conditions. Neck pain. Best Practice & Research Clinical Rheumatology , 2007 Feb;21(1):93-108. (LoE:5)
- ↑ Nielsen PK, Andersen LL, Olsen HB, Rosendal L, Sjøgaard G, Søgaard K. Effect of physical training on pain sensitivity and trapezius muscle morphology. Muscle & Nerve: Official Journal of the American Association of Electrodiagnostic Medicine. 2010 Jun;41(6):836-44.
- ↑ 29.0 29.1 Andersen LL, Kjaer M, SØgaard K, Hansen L, Kryger AI, Sjögaard G. Effect of two contrasting types of physical exercise on chronic neck muscle pain. Arthritis Care & Research: Official Journal of the American College of Rheumatology. 2008 Jan;59(1):84-91.(LoE:2B)
- ↑ Ylinen J, Hakkinen A, Nykanen M, Kautiainen H, Takala E. Neck muscle training in the treatment of chronic neck pain: a three-year follow-up study. Europa medicophysica. 2007 Jun 1;43(2):161.(LoE:2B)
- ↑ Rodrigues EV, Gomes AR, Tanhoffer AI, Leite N. Effects of exercise on pain of musculoskeletal disorders: a systematic review. Acta ortopedica brasileira. 2014 Dec;22(6):334-8.(LoE:1A)
- ↑ Hagberg M, Harms-Ringdahl K, Nisell R, Hjelm EW. Rehabilitation of neck-shoulder pain in women industrial workers: a randomized trial comparing isometric shoulder endurance training with isometric shoulder strength training. Archives of physical medicine and rehabilitation. 2000 Aug 1;81(8):1051-8.
- ↑ Zebis MK, Andersen LL, Pedersen MT, Mortensen P, Andersen CH, Pedersen MM, Boysen M, Roessler KK, Hannerz H, Mortensen OS, Sjøgaard G. Implementation of neck/shoulder exercises for pain relief among industrial workers: a randomized controlled trial. BMC musculoskeletal disorders. 2011 Dec;12(1):205.
- ↑ Physiotutors. Tight Upper Traps? Try These Exercises!. Available from: https://www.youtube.com/watch?v=4D6_sK6hxLQ
- ↑ Andersen LL, Blangsted AK, Nielsen PK, Hansen L, Vedsted P, Sjøgaard G, Søgaard K. Effect of cycling on oxygenation of relaxed neck/shoulder muscles in women with and without chronic pain. European journal of applied physiology. 2010 Sep 1;110(2):389-94.(LoE:2B)
- ↑ Hägg GM. Human muscle fibre abnormalities related to occupational load. European journal of applied physiology. 2000 Oct 1;83(2-3):159-65.
- ↑ Larsson R, Öberg PÅ, Larsson SE. Changes of trapezius muscle blood flow and electromyography in chronic neck pain due to trapezius myalgia. Pain. 1999 Jan 1;79(1):45-50.
- ↑ Rosendal L, Larsson B, Kristiansen J, Peolsson M, Søgaard K, Kjær M, Sørensen J, Gerdle B. Increase in muscle nociceptive substances and anaerobic metabolism in patients with trapezius myalgia: microdialysis in rest and during exercise. Pain. 2004 Dec 1;112(3):324-34.