Transient Ischaemic Attack (TIA): Difference between revisions
No edit summary |
(text, physio section & other sections) |
||
| Line 9: | Line 9: | ||
== <span style="line-height: 1.5em; background-color: initial;">Introduction</span> == | == <span style="line-height: 1.5em; background-color: initial;">Introduction</span> == | ||
The clinical definitions of TIA and ischemic stroke are based on focal neurologic signs or symptoms referable to known cerebral arterial distributions without direct measurement of blood flow or cerebral infarction. It is important to note that TIA and stroke represent different ends of an ischemic continuum from the physiologic perspective, but clinical management is similar<ref>Coutts SB. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5898963/ Diagnosis and management of transient ischemic attack]. Continuum: Lifelong Learning in Neurology. 2017 Feb 3;23(1):82. AVAILABLE FROM: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5898963/ (last accessed 27.12.2019)</ref>. | |||
*lasts less than an hour | The definition of a TIA has moved from time-based to tissue-based. A TIA | ||
* | * typically lasts less than an hour, more often minutes | ||
* | * can be considered as a serious warning for an impending ischemic stroke - the risk is highest in the first 48 hours following a transient ischemic attack. differentiating transient ischemic attack from other mimicking conditions is important | ||
* usually associated with a focal neurologic deficit and/or speech disturbance in a vascular territory due to underlying cerebrovascular disease | |||
* always sudden in onset. | |||
Evaluation of TIA should be done urgently with imaging and laboratory studies to decrease the risk of subsequent strokes. The subsequent risk of TIA or ischemic stroke can be stratified with a simple clinical measure. Immediate multimodality therapeutic interventions should be initiated.<ref name=":0">Panuganti KK, Tadi P, Lui F. [https://www.ncbi.nlm.nih.gov/books/NBK459143/ Transient ischemic attack.] InStatPearls [Internet] 2019 Mar 21. StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459143/ (last accessed 27.12.2019)</ref> | |||
The concept of TIA emerged in the 1950s, with the observation by C Miller Fisher, and others, that ischaemic stroke often followed transient neurological symptoms in the same arterial territory<ref>Estol CJ (March 1996). "Dr C. Miller Fisher and the history of carotid artery disease". Stroke 27 (3): 559–66.</ref>. | The concept of TIA emerged in the 1950s, with the observation by C Miller Fisher, and others, that ischaemic stroke often followed transient neurological symptoms in the same arterial territory<ref>Estol CJ (March 1996). "Dr C. Miller Fisher and the history of carotid artery disease". Stroke 27 (3): 559–66.</ref>. | ||
== Mechanism of Injury / Pathological Process == | |||
== Mechanism of Injury / Pathological Process | |||
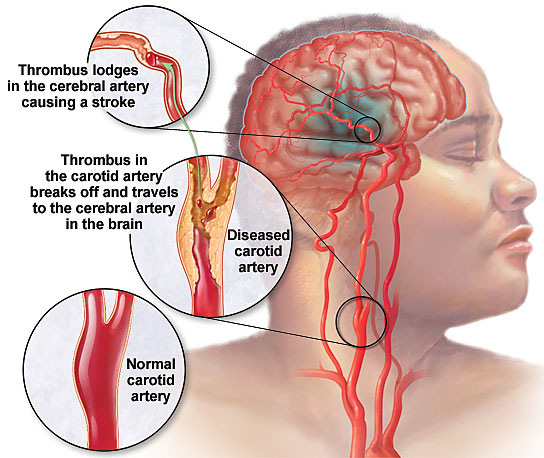
Like ischaemic strokes, TIAs are due to locally decreased blood flow to the brain, causing focal neurological symptoms. Decreased blood flow results from either embolism into a cerebral supply artery (from the heart, or the great proximal vessels, extracranial or intracranial arteries, usually affected by atherosclerosis), or in situ occlusion of small perforating arteries. | Like ischaemic strokes, TIAs are due to locally decreased blood flow to the brain, causing focal neurological symptoms. Decreased blood flow results from either embolism into a cerebral supply artery (from the heart, or the great proximal vessels, extracranial or intracranial arteries, usually affected by atherosclerosis), or in situ occlusion of small perforating arteries. | ||
| Line 24: | Line 26: | ||
[[Image:Transient-Ischemic-Attacks.jpg|center]] | [[Image:Transient-Ischemic-Attacks.jpg|center]] | ||
== Etiology == | |||
TIA subtypes, classified according to the pathophysiological mechanisms are similar to ischemic stroke subtypes. They include <ref name=":0" /> | |||
* large artery atherothrombosis | |||
* cardiac embolism | |||
* small vessel (lacunar) | |||
* cryptogenic | |||
* uncommon subtypes such as vascular dissection, vasculitis etc. | |||
The common risk factors for all TIA include diabetes, hypertension, age, smoking, obesity, alcoholism, unhealthy diet, psychosocial stress, and lack of regular physical activity. A previous history of stroke or TIA will increase substantially the subsequent risk of recurrent stroke or TIA.[4][5] Among all risk factors, hypertension is the most important one for an individual as well as in a population. | |||
== Epidemiology == | == Epidemiology == | ||
TIA incidence in a population is difficult to estimate due to other mimicking disorders. Internationally, the probability of a first TIA is around 0.42 per 1000 population in developed countries<ref>Truelsen T, Begg S, Mathers C. World Health Organization. The global burden of cerebrovascular disease. Global Burden of Disease 2000</ref>. TIA incidence in the United States could be around half a million per year, and estimates are about 1.1 per 1000 in the United States population. The estimated overall prevalence of TIA among adults in the United States is approximately 2%<ref name=":0" />. TIAs occur in about 150,000 patients per year in the United Kingdom<ref>Giles MF, Rothwell PM. Risk of stroke early after transient ischaemic attack: a systematic review and meta-analysis. Lancet Neurol. Dec 2007;6(12):1063-72</ref>. It has been shown that previous stroke history increases the prevalence of TIA. Few studies have shown that the majority of people who presented with initial stroke had prior TIA symptoms. | |||
Internationally, the probability of a first TIA is around 0.42 per 1000 population in developed countries<ref>Truelsen T, Begg S, Mathers C. World Health Organization. The global burden of cerebrovascular disease. Global Burden of Disease 2000</ref>. TIAs occur in about 150,000 patients per year in the United Kingdom<ref>Giles MF, Rothwell PM. Risk of stroke early after transient ischaemic attack: a systematic review and meta-analysis. Lancet Neurol. Dec 2007;6(12):1063-72</ref>. | |||
'''Age''' | '''Age''' | ||
| Line 51: | Line 60: | ||
The main diagnostic challenge of TIA is that the symptoms and signs have usually resolved by the time of assessment<ref>Sheehan OC, Merwick A, Kelly LA, et al. Diagnostic usefulness of the ABCD2 score to distinguish transient ischemic attack and minor ischemic stroke from noncerebrovascular events: the North Dublin TIA Study. Stroke 2009;40:3449–54</ref>. | The main diagnostic challenge of TIA is that the symptoms and signs have usually resolved by the time of assessment<ref>Sheehan OC, Merwick A, Kelly LA, et al. Diagnostic usefulness of the ABCD2 score to distinguish transient ischemic attack and minor ischemic stroke from noncerebrovascular events: the North Dublin TIA Study. Stroke 2009;40:3449–54</ref>. | ||
National Stroke Association has established guidelines for TIA evaluation as follows in 2006:<ref name=":0" /> | |||
== | CBC = complete blood countCEA = carotid endarterectomyTCD = transcranial Doppler TEE = transesophageal echocardiogramTTE = transthoracic echocardiogram | ||
ABCD2 score is very important for predicting subsequent risks of TIA or stroke. It provides a more robust prediction standard. The ABCD2 score includes factors including age, blood pressure, clinical symptoms, duration, and diabetes. | |||
* Age: older than 60 years (1 point) | |||
* Bood pressure greater than or equal to 140/90 mmHg on first evaluation (1 point) | |||
* Clinical symptoms: focal weakness with the spell (2 points) or speech impairment without weakness (1 point) | |||
* Duration greater than 60 min (2 points), or 10 min to 59 min (1 point) | |||
* Diabetes mellitus (1 point). | |||
The 2-day risk of stroke was 0% for scores of 0 or 1, 1.3% for 2 or 3, 4.1% for 4 or 5, and 8.1% for 6 or 7. | |||
Most stroke centers will admit patients with TIA to the hospital for expedited management and observation if the score is 4 or 5 or higher. | |||
For those patients who have a lower score, expedited evaluation and management is still warranted. This expedited approach has been proven to improve the outcome | |||
Syncope | == Differential Diagnosis == | ||
Differential diagnosis of TIA includes but is not limited to<ref name=":0" /> | |||
* vertigo or dizziness | |||
* seizures | |||
* headaches, [[Migraine Headache|migraine]] Aura | |||
* bells palsy | |||
* drug withdrawal | |||
* dementia | |||
* electrolyte disorders | |||
* acute infections | |||
* alcoholism.<br>[[Stroke|Stroke]]<br>[[Meningitis|Meningitis]] | |||
* [[MS Multiple Sclerosis|Multiple Sclerosis]]<br>Syncope | |||
=== Physiotherapy === | |||
There is still a lack of studies addressing the physiotherapists’ role in lifestyle behavior changes in the TIA population. Longitudinal studies are required to enable a more detailed and specific understanding of how to help persons with stroke/TIA makes lifestyle behavior changes. A need exists to further explore what interventions are needed. | |||
Physiotherapists have a role in this population and when treating patients with chronic conditions of bringing awareness/discussing life style behavior changes<ref>The 4th European Congress of the ER-WCPT / Physiotherapy 102S (2016) eS67–eS282 [https://www.physiotherapyjournal.com/article/S0031-9406(16)30153-5/pdf Physio role in TIA] Available from: https://www.physiotherapyjournal.com/article/S0031-9406(16)30153-5/pdf (last accessed 27.12.2019)</ref>. | |||
=== learn more about TIA === | |||
{| width="100%" cellspacing="1" cellpadding="1" | {| width="100%" cellspacing="1" cellpadding="1" | ||
|- | |- | ||
| Line 83: | Line 107: | ||
<br> | <br> | ||
== Resources | == Resources == | ||
add appropriate resources here | add appropriate resources here | ||
| Line 90: | Line 114: | ||
add links to case studies here (case studies should be added on new pages using the [[Template:Case Study|case study template]])<br> | add links to case studies here (case studies should be added on new pages using the [[Template:Case Study|case study template]])<br> | ||
== References == | == References == | ||
<references /><br> | <references /><br> | ||
[[Category:Neurology]] [[Category:Neurological - Conditions]] | [[Category:Neurology]] | ||
[[Category:Stroke]] [[Category:Stroke - Conditions]] | [[Category:Neurological - Conditions]] | ||
[[Category:Head]] [[Category:Head - Conditions]] [[Category:Conditions]] | [[Category:Stroke]] | ||
[[Category:Stroke - Conditions]] | |||
[[Category:Head]] | |||
[[Category:Head - Conditions]] | |||
[[Category:Conditions]] | |||
Revision as of 07:28, 27 December 2019
This article is currently under review and may not be up to date. Please come back soon to see the finished work! (27/12/2019)
Original Editor - Wendy Walker
Lead Editors
Introduction[edit | edit source]
The clinical definitions of TIA and ischemic stroke are based on focal neurologic signs or symptoms referable to known cerebral arterial distributions without direct measurement of blood flow or cerebral infarction. It is important to note that TIA and stroke represent different ends of an ischemic continuum from the physiologic perspective, but clinical management is similar[1].
The definition of a TIA has moved from time-based to tissue-based. A TIA
- typically lasts less than an hour, more often minutes
- can be considered as a serious warning for an impending ischemic stroke - the risk is highest in the first 48 hours following a transient ischemic attack. differentiating transient ischemic attack from other mimicking conditions is important
- usually associated with a focal neurologic deficit and/or speech disturbance in a vascular territory due to underlying cerebrovascular disease
- always sudden in onset.
Evaluation of TIA should be done urgently with imaging and laboratory studies to decrease the risk of subsequent strokes. The subsequent risk of TIA or ischemic stroke can be stratified with a simple clinical measure. Immediate multimodality therapeutic interventions should be initiated.[2]
The concept of TIA emerged in the 1950s, with the observation by C Miller Fisher, and others, that ischaemic stroke often followed transient neurological symptoms in the same arterial territory[3].
Mechanism of Injury / Pathological Process[edit | edit source]
Like ischaemic strokes, TIAs are due to locally decreased blood flow to the brain, causing focal neurological symptoms. Decreased blood flow results from either embolism into a cerebral supply artery (from the heart, or the great proximal vessels, extracranial or intracranial arteries, usually affected by atherosclerosis), or in situ occlusion of small perforating arteries.
Resolution of symptoms probably occurs by spontaneous lysis or distal passage of the occluding thrombus or embolus, or by compensation through collateral circulation restoring perfusion into the ischaemic brain area.
Etiology[edit | edit source]
TIA subtypes, classified according to the pathophysiological mechanisms are similar to ischemic stroke subtypes. They include [2]
- large artery atherothrombosis
- cardiac embolism
- small vessel (lacunar)
- cryptogenic
- uncommon subtypes such as vascular dissection, vasculitis etc.
The common risk factors for all TIA include diabetes, hypertension, age, smoking, obesity, alcoholism, unhealthy diet, psychosocial stress, and lack of regular physical activity. A previous history of stroke or TIA will increase substantially the subsequent risk of recurrent stroke or TIA.[4][5] Among all risk factors, hypertension is the most important one for an individual as well as in a population.
Epidemiology[edit | edit source]
TIA incidence in a population is difficult to estimate due to other mimicking disorders. Internationally, the probability of a first TIA is around 0.42 per 1000 population in developed countries[4]. TIA incidence in the United States could be around half a million per year, and estimates are about 1.1 per 1000 in the United States population. The estimated overall prevalence of TIA among adults in the United States is approximately 2%[2]. TIAs occur in about 150,000 patients per year in the United Kingdom[5]. It has been shown that previous stroke history increases the prevalence of TIA. Few studies have shown that the majority of people who presented with initial stroke had prior TIA symptoms.
Age
The incidence of TIAs increases with age, from 1-3 cases per 100,000 in those younger than 35 years to as many as 1500 cases per 100,000 in those older than 85 years[6]. Fewer than 3% of all major cerebral infarcts occur in children. Paediatric strokes often can have quite different etiologies from those of adult strokes and tend to occur with less frequency.
Gender
The incidence of TIAs in men (101 cases per 100,000 population) is significantly higher than that in women (70 per 100,000)[7].
Clinical Presentation[edit | edit source]
Clinical manifestations will vary, depending on the vessel involved and the cerebral territory it supplies.
The key rule here is that symptoms of TIA should mimic known stroke syndromes, and so depend on the arterial territory involved; see the Stroke page for details
A TIA may last only minutes, therefore symptoms have often resolved before the patient presents to a clinician. Thus, historical questions should be addressed not just to the patient but also to family members or friends who were present at the time of TIA. Witnesses often perceive abnormalities that the patient cannot, such as changes in behaviour, speech, gait, memory, and movement.
Diagnostic Procedures[edit | edit source]
The main diagnostic challenge of TIA is that the symptoms and signs have usually resolved by the time of assessment[8].
National Stroke Association has established guidelines for TIA evaluation as follows in 2006:[2]
CBC = complete blood countCEA = carotid endarterectomyTCD = transcranial Doppler TEE = transesophageal echocardiogramTTE = transthoracic echocardiogram
ABCD2 score is very important for predicting subsequent risks of TIA or stroke. It provides a more robust prediction standard. The ABCD2 score includes factors including age, blood pressure, clinical symptoms, duration, and diabetes.
- Age: older than 60 years (1 point)
- Bood pressure greater than or equal to 140/90 mmHg on first evaluation (1 point)
- Clinical symptoms: focal weakness with the spell (2 points) or speech impairment without weakness (1 point)
- Duration greater than 60 min (2 points), or 10 min to 59 min (1 point)
- Diabetes mellitus (1 point).
The 2-day risk of stroke was 0% for scores of 0 or 1, 1.3% for 2 or 3, 4.1% for 4 or 5, and 8.1% for 6 or 7.
Most stroke centers will admit patients with TIA to the hospital for expedited management and observation if the score is 4 or 5 or higher.
For those patients who have a lower score, expedited evaluation and management is still warranted. This expedited approach has been proven to improve the outcome
Differential Diagnosis[edit | edit source]
Differential diagnosis of TIA includes but is not limited to[2]
- vertigo or dizziness
- seizures
- headaches, migraine Aura
- bells palsy
- drug withdrawal
- dementia
- electrolyte disorders
- acute infections
- alcoholism.
Stroke
Meningitis - Multiple Sclerosis
Syncope
Physiotherapy[edit | edit source]
There is still a lack of studies addressing the physiotherapists’ role in lifestyle behavior changes in the TIA population. Longitudinal studies are required to enable a more detailed and specific understanding of how to help persons with stroke/TIA makes lifestyle behavior changes. A need exists to further explore what interventions are needed.
Physiotherapists have a role in this population and when treating patients with chronic conditions of bringing awareness/discussing life style behavior changes[9].
learn more about TIA[edit | edit source]
Key Evidence[edit | edit source]
Resources[edit | edit source]
add appropriate resources here
Case Studies[edit | edit source]
add links to case studies here (case studies should be added on new pages using the case study template)
References[edit | edit source]
- ↑ Coutts SB. Diagnosis and management of transient ischemic attack. Continuum: Lifelong Learning in Neurology. 2017 Feb 3;23(1):82. AVAILABLE FROM: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5898963/ (last accessed 27.12.2019)
- ↑ 2.0 2.1 2.2 2.3 2.4 Panuganti KK, Tadi P, Lui F. Transient ischemic attack. InStatPearls [Internet] 2019 Mar 21. StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459143/ (last accessed 27.12.2019)
- ↑ Estol CJ (March 1996). "Dr C. Miller Fisher and the history of carotid artery disease". Stroke 27 (3): 559–66.
- ↑ Truelsen T, Begg S, Mathers C. World Health Organization. The global burden of cerebrovascular disease. Global Burden of Disease 2000
- ↑ Giles MF, Rothwell PM. Risk of stroke early after transient ischaemic attack: a systematic review and meta-analysis. Lancet Neurol. Dec 2007;6(12):1063-72
- ↑ Kleindorfer D, Panagos P, Pancioli A, et al. Incidence and short-term prognosis of transient ischemic attack in a population-based study. Stroke. Apr 2005;36(4):720-3
- ↑ Bots ML, van der Wilk EC, Koudstaal PJ, Hofman A, Grobbee DE. Transient neurological attacks in the general population. Prevalence, risk factors, and clinical relevance. Stroke. Apr 1997;28(4):768-73
- ↑ Sheehan OC, Merwick A, Kelly LA, et al. Diagnostic usefulness of the ABCD2 score to distinguish transient ischemic attack and minor ischemic stroke from noncerebrovascular events: the North Dublin TIA Study. Stroke 2009;40:3449–54
- ↑ The 4th European Congress of the ER-WCPT / Physiotherapy 102S (2016) eS67–eS282 Physio role in TIA Available from: https://www.physiotherapyjournal.com/article/S0031-9406(16)30153-5/pdf (last accessed 27.12.2019)