Subacromial Pain Syndrome: Difference between revisions
No edit summary |
mNo edit summary |
||
| Line 64: | Line 64: | ||
<br> | <br> | ||
Non-operative treatment is typically attempted first, assuming there is no significant biceps or rotator cuff tear that will require surgery. [[Manual Techniques for the Shoulder|Shoulder manual therapy techniques]] have been shown in multiple studies to be effective for treatment of subacromial impingement. In particular, manual therapy techniques have been shown to have a significant effect on improving pain levels in patients with SAI. Although exercise therapy alone has been shown to bring decreased pain, the addition of manual therapy further augments those gains and also aids in greater strength gains than exercise alone<ref>Bang MD, Deyle GD. Comparison of Supervised Exercise With and Without Manual Physical Therapy for Patients with Shoulder Impingement Syndrome. Journal of Orthopaedic and Sports Physical Therapy. 2000;30(3):126-137.</ref>. Acromioplasty and/or manual therapy may be used alongside therapeutic exercise to improve functional and impairment-level gains, depending on severity of anatomic dysfunction involved. Although exercise treatment is a vital part of treatment for this condition, results showed no significant difference between home-based exercises and clinical exercise. Once manual therapy is no longer necessary and the patient has an adequate home exercise program, forma therapy is often no longer necessary<ref>Kuhn JE. Exercise in the treatment of rotator cuff impingement: A systematic review and synthesized evidence-based rehabilitation protocol. Journal fo Shoulder and Elbow Surgery. 2009;18:138-160.</ref>. Soft tissue mobilization to normalize muscle spasm and other soft tissue dysfunction has been shown to be effective alongside joint mobilizations to restore motion in treatment of SAI<ref>Senbursa G, Baltaci G, Atay A. Comparison of conservative treatment with and without manual physical therapy for patients with shoulder impingement syndrome: a prospective, randomized clinical trial. Knee Surg Sports Traumatol Arthoscop. 2007;15:915-921.</ref> | Non-operative treatment is typically attempted first, assuming there is no significant biceps or rotator cuff tear that will require surgery. [[Manual Techniques for the Shoulder|Shoulder manual therapy techniques]] have been shown in multiple studies to be effective for treatment of subacromial impingement. In particular, manual therapy techniques have been shown to have a significant effect on improving pain levels in patients with SAI. Although exercise therapy alone has been shown to bring decreased pain, the addition of manual therapy further augments those gains and also aids in greater strength gains than exercise alone<ref>Bang MD, Deyle GD. Comparison of Supervised Exercise With and Without Manual Physical Therapy for Patients with Shoulder Impingement Syndrome. Journal of Orthopaedic and Sports Physical Therapy. 2000;30(3):126-137.</ref>. Acromioplasty and/or manual therapy may be used alongside therapeutic exercise to improve functional and impairment-level gains, depending on severity of anatomic dysfunction involved. Although exercise treatment is a vital part of treatment for this condition, results showed no significant difference between home-based exercises and clinical exercise. Once manual therapy is no longer necessary and the patient has an adequate home exercise program, forma therapy is often no longer necessary. Therapeutic exercise should include rotator cuff strengthening, lower and middle trapezius strengthening.<ref>Kuhn JE. Exercise in the treatment of rotator cuff impingement: A systematic review and synthesized evidence-based rehabilitation protocol. Journal fo Shoulder and Elbow Surgery. 2009;18:138-160.</ref>. Soft tissue mobilization to normalize muscle spasm and other soft tissue dysfunction has been shown to be effective alongside joint mobilizations to restore motion in treatment of SAI<ref>Senbursa G, Baltaci G, Atay A. Comparison of conservative treatment with and without manual physical therapy for patients with shoulder impingement syndrome: a prospective, randomized clinical trial. Knee Surg Sports Traumatol Arthoscop. 2007;15:915-921.</ref> | ||
== Differential Diagnosis<br> == | == Differential Diagnosis<br> == | ||
Revision as of 02:14, 13 April 2010
Be the first to edit this page and have your name permanently included as the original editor, see the editing pages tutorial for help.
|
Original Editor - David Drinkard Lead Editors - Your name will be added here if you are a lead editor on this page. Read more. |
Clinically Relevant Anatomy
[edit | edit source]
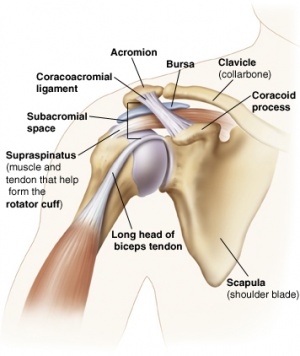
Subacromial Impingement is defined as the compression of the subacromial structures (rotator cuff tendons, long head of the biceps, glenohumeral joint capsule, and subacromial bursa) during elevation of the arm. These structures are compressed against the coracoacromial arch[1], creating sensations of pain. The margin between the superior portion of the humeral head and the inferior
surface of the acromion is known as the subacromial space. In healthy individuals, this space is approximately 10mm, but as this space narrows the likelihood of tissue irritation increases. This margin holds the supraspinatus muscle belly and tendon, long head of the biceps brachii, and subacromial bursa. Subacromial structures can be pinched either due to pathologic factors (muscle imbalance, overuse) or anatomic factors. The shape of the acromion can play a role. There are three types of acromial shapes:
- Type I Acromion: Flat shape (Least likely to contribute to impingement)
- Type II Acromion: Curved shape
- Type III Acromion: Hooked shape (Most likely to contribute to impingement)
Bony spurs on the underside of the acromion process can also cause irritation of the subacromial structures.
Mechanism of Injury / Pathological Process
[edit | edit source]
Impingement is often a condition than can have a variety of causes acting together to create symptoms. Subacromial impingement occurs when the arm is elevated, narrowing the subacromial space and compressing the structures that reside in that margin. With repeated elevation, these structures sustain microtrauma that can cause them to become inflammed. Subacromial impingement can be caused by a variety of factors:
- Rotator cuff weakness, causing the humeral head to drift superiorally
- Chronic rotator cuff irritation due to overuse
- Posterior GH capsule tightness
- Anatomical variations such as narrow SA space, Type II or III Acromion, or bony spurs
- Poor posture (forward shoulder posture can cause functional narrowing of subacromial space)
Clinical Presentation[edit | edit source]
Individuals with subacromial impingement will usually complain of pain with active elevation of the shoulder. Activities performed with the involved arm below shoulder level are often not painful because the subacromial structure are not impinged when the shoulder is in anatomic position. These individuals often do not remember a traumatic incident as the onset is more of a gradual, degenerative condition rather than due to a strong external force.
Diagnostic Procedures[edit | edit source]
Also see Impingement Cluster page
An accurate history is often one of the best indicators in diagnosing subacromial impingement. However, many diagnostic procedures can be used to validate this diagnosis. The following are a few special tests for the presence of subacromial impingement:
Outcome Measures[edit | edit source]
add links to outcome measures here (see Outcome Measures Database)
Management / Interventions
[edit | edit source]
Treatment of subacromial impingement can be managed either operatively or non-operatively.
Operative treatment usually includes repair of any tissues that have been damaged due to repetitive trauma. Such structures often involve the supraspinatus muscle and/or tendon, proximal biceps tendon, or joint capsule. Removal of the subacromial bursa is a procedure known as a bursectomy. A procedure known as a subacromial decompression (SAD) is often performed to increase the available space in the subacromail space by removing bony spurs, removing the coracoacromial ligament, and even occasionally removing the most inferior portion of the acromion (acromioplasty).
Non-operative treatment is typically attempted first, assuming there is no significant biceps or rotator cuff tear that will require surgery. Shoulder manual therapy techniques have been shown in multiple studies to be effective for treatment of subacromial impingement. In particular, manual therapy techniques have been shown to have a significant effect on improving pain levels in patients with SAI. Although exercise therapy alone has been shown to bring decreased pain, the addition of manual therapy further augments those gains and also aids in greater strength gains than exercise alone[2]. Acromioplasty and/or manual therapy may be used alongside therapeutic exercise to improve functional and impairment-level gains, depending on severity of anatomic dysfunction involved. Although exercise treatment is a vital part of treatment for this condition, results showed no significant difference between home-based exercises and clinical exercise. Once manual therapy is no longer necessary and the patient has an adequate home exercise program, forma therapy is often no longer necessary. Therapeutic exercise should include rotator cuff strengthening, lower and middle trapezius strengthening.[3]. Soft tissue mobilization to normalize muscle spasm and other soft tissue dysfunction has been shown to be effective alongside joint mobilizations to restore motion in treatment of SAI[4]
Differential Diagnosis
[edit | edit source]
There are a variety of shoulder conditions that can initially confused with subacromial impingement, although a thorough examination is usually sufficient for identifying this condition. Partial and full rotator cuff tears are often the result of subacromial impingement, but can occur without impingement and usually demonstrate some sort of lag sign upon evaluation. Adhesive capsulitis, or "frozen shoulder", can also present with limitation of active shoulder elevation and significant shoulder pain; however, adhesive capsulitis usually presents with glenohumeral motion loss in a capsular pattern, meaning that external rotation and abduction are the two directions with the greatest magnitude of motion lost.
Key Evidence[edit | edit source]
add text here relating to key evidence with regards to any of the above headings
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ Kachingwe AF, Phillips B, Sletten E, Plunkett SW. Comparison of Manual Therapy Techniques with Therapeutic Exercise in the Treatment of Shoulder Impingement: A Randomized Controlled Pilot Clinical Trial. The Journal of Manual &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Manipulative Therapy 2008;16(4):238-247.
- ↑ Bang MD, Deyle GD. Comparison of Supervised Exercise With and Without Manual Physical Therapy for Patients with Shoulder Impingement Syndrome. Journal of Orthopaedic and Sports Physical Therapy. 2000;30(3):126-137.
- ↑ Kuhn JE. Exercise in the treatment of rotator cuff impingement: A systematic review and synthesized evidence-based rehabilitation protocol. Journal fo Shoulder and Elbow Surgery. 2009;18:138-160.
- ↑ Senbursa G, Baltaci G, Atay A. Comparison of conservative treatment with and without manual physical therapy for patients with shoulder impingement syndrome: a prospective, randomized clinical trial. Knee Surg Sports Traumatol Arthoscop. 2007;15:915-921.