Stroke: Difference between revisions
No edit summary |
Scott Buxton (talk | contribs) No edit summary |
||
| Line 6: | Line 6: | ||
== Clinically Relevant Anatomy<br> == | == Clinically Relevant Anatomy<br> == | ||
[[Image:CircleofWillis.gif|frame|center|300px|Circle of Willis]]At the base of the brain, the carotid and vertebrobasilar arteries form a circle of communicating arteries known as the Circle of Willis. From this circle, other arteries—the anterior cerebral artery (ACA), the middle cerbral artery (MCA) and posterior cerebral artery (PCA)—arise and travel to all parts of the brain. <br><br> | [[Image:CircleofWillis.gif|frame|center|300px|Circle of Willis]]At the base of the brain, the carotid and vertebrobasilar arteries form a circle of communicating arteries known as the Circle of Willis. From this circle, other arteries—the anterior cerebral artery (ACA), the middle cerbral artery (MCA) and posterior cerebral artery (PCA)—arise and travel to all parts of the brain. <br><br> | ||
== Mechanism of Injury / Pathological Process<br> == | == Mechanism of Injury / Pathological Process<br> == | ||
| Line 72: | Line 72: | ||
| <br> | | <br> | ||
| align="right" | | | align="right" | | ||
{{#ev:youtube|NSWnNnfDt70|350}} <ref> USMLEFastTrack. Effects of Strokes - Anterior Cerebral & Lateral Striate Artery. Available from: http://www.youtube.com/watch?v=NSWnNnfDt70 [last accessed 10/10/14]</ref> | {{#ev:youtube|NSWnNnfDt70|350}} <ref> USMLEFastTrack. Effects of Strokes - Anterior Cerebral &amp; Lateral Striate Artery. Available from: http://www.youtube.com/watch?v=NSWnNnfDt70 [last accessed 10/10/14]</ref> | ||
|} | |} | ||
| Line 111: | Line 111: | ||
<references /> | <references /> | ||
[[Category:Neurology]][[Category:Older_People/Geriatrics|Geriatrics]][[Category:Condition]][[Category:Videos]] | [[Category:Neurology]][[Category:Older_People/Geriatrics|Geriatrics]][[Category:Condition]][[Category:Videos]][[Category:Stroke]] | ||
Revision as of 14:43, 25 October 2014
Original Editor - Wendy Walker
Top Contributors - Admin, Wendy Walker, Kim Jackson, Rachael Lowe, Laura Ritchie, Vidya Acharya, Naomi O'Reilly, Lucinda hampton, Tony Lowe, Katherine McBeth, Scott Buxton, Sweta Christian, Evan Thomas, Magdalena Hytros, Priyanka Chugh, Simisola Ajeyalemi, 127.0.0.1, Rucha Gadgil, Amrita Patro and Karen Wilson
Clinically Relevant Anatomy
[edit | edit source]
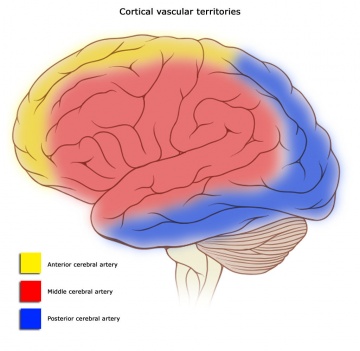
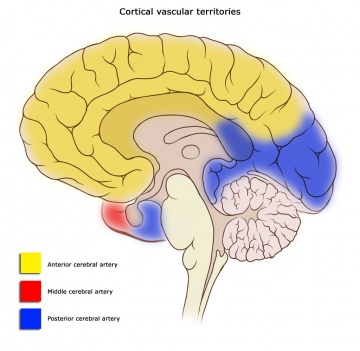
At the base of the brain, the carotid and vertebrobasilar arteries form a circle of communicating arteries known as the Circle of Willis. From this circle, other arteries—the anterior cerebral artery (ACA), the middle cerbral artery (MCA) and posterior cerebral artery (PCA)—arise and travel to all parts of the brain.
Mechanism of Injury / Pathological Process
[edit | edit source]
| [1] |
A stroke occurs when there is interruption of the blood supply to a particular area of the brain, ultimately leading to cell injury and cell death.
Strokes can be classified as either:
- Ischaemic
- Haemorrhagic
Ischaemic strokes are the most common, accounting for up to 80% of strokes, and occur when there is an occlusion of a blood vessel impairing the flow of blood to the brain.
Ischaemic strokes are divided into:
1. thrombotic - where a blood clot forms in a main brain artery or within the small blood vessels deep inside the brain. The clot usually forms around atherosclerotic plaques.
2. embolic - a blood clot, air bubble or fat globule forms within a blood vessel elsewhere in the body and is carried to the brain.
3. systemic hypoprofusion - a general decrease in blood supply, eg. in shock.
4. venous thrombosis
Haemorrhagic strokes occur when a blood vessel in the brain ruptures and bleeds.
1. Intracerebral haemorrhagic stroke — there is bleeding from a blood vessel within the brain. High blood pressure is the main cause of intracerebral haemorrhagic stroke.
2. Subarachnoid haemorrhagic stroke — there is bleeding from a blood vessel between the surface of the brain and the arachnoid tissues that cover the brain.
Nb. Some experts do not classify subarachnoid haemorrhage as stroke because subarachnoid haemorrhages present differently from ischaemic strokes and intracerebral haemorrhagic strokes.
Epidemiology/Etiology[edit | edit source]
According to the World Health Organization (WHO), 15 million people suffer stroke worldwide each year. Of these, 5 million die and another 5 million are left permanently disabled.[2]
Stroke subtypes vary greatly in different parts of the world and between different races. For example, the proportion of ahemorrhagic strokes may be higher in certain populations, such as the Chinese population, in which it has been reported to be up to 39.4%, and the Japanese, in which it is reportedly up to 38.7%.[3]
Stroke kills more than 49,000 people each year in the UK, nearly 1 in 10.
In 2010 stroke was the fourth largest cause of death in the UK after cancer, heart disease and respiratory disease.[4]
Clinical Presentation[edit | edit source]
Cortical Areas and their vascular supply:
LOCATION OF INFARCT & DEFICITS PRODUCED:[edit | edit source]
Left MCA Superficial Division
Right face and arm upper-motor weakness due to damage to motor cortex, nonfluent (Broca’s) aphasia due to damage to Broca’s area. There may also be right face and arm cortical type sensory loss if the infarct involves the sensory cortex. Other deficits include a fluent (Wernicke’s) aphasia due to damage to Wernicke’s area.
Right MCA Superficial Division
Left face and arm upper-motor weakness due to damage to motor cortex. Left hemineglect (variable) due to damage to non-dominant association areas. There may also be left face and arm cortical type sensory loss if the infarct involves the sensory cortex.
Left MCA Lenticulostriate Branches
Right pure upper-motor hemiparesis due to damage to the basal ganglia (globus pallidus and striatum) and the genu of the internal capsule on the left side. Larger infarcts extending to the cortex may produce cortical deficits such as aphasia.
Right MCA Lenticulostriate Branches
Left pure upper-motor hemiparesis due to damage to the basal ganglia (globus pallidus and striatum) and the genu of the internal capsule on the right side. Larger infarcts extending to the cortex may produce cortical deficits such aphasia.
Left PCA
Right homonymous hemianopsia due to damage to left visual cortex in the occipital lobe. Extension to the the corpus collusom interferes with comunication between the two visual association areas so can cause alexia without agraphia. Larger infarcts involving the internal capsule and thalamus may cause right hemisensory loss and right hemiparesis due to disruption of the ascending and descending information passing through these structures.
Right PCA
Left homonymous hemianopia due to damage to right visual cortex in the occipital lobe. Larger infarcts involving the internal capsule and thalamus may cause left hemisensory loss and left hemiparesis due to disruption of the ascending and descending information passing through these structures.
| [5] | [6] | [7] |
Outcome Measures[edit | edit source]
Dynamic Gait Index, the 4-item Dynamic Gait Index, and the Functional Gait Assessment show sufficient validity, responsiveness, and reliability for assessment of walking function in patients with stroke undergoing rehabilitation, but the Functional Gait Assessment is recommended for its psychometric properties[8].
Physiotherapy[edit | edit source]
Physiotherapists should be involved early, and should make their own assessment of how much they can work with a patient. Early mobilization is associated with better outcomes - even after taking account of the potential confounding influence of disease severity. If rehabilitation is to take place on a different ward from acute care, the care received should be made as seamless as possible. Type and intensity of therapy should be determined by the patient's needs not location.[9]
Management / Interventions
[edit | edit source]
Early management of acute stroke: The goal for the acute management of patients with stroke is to stabilize the patient and to complete initial evaluation and assessment, including imaging and laboratory studies, within a short time frame. Critical decisions focus on the need for intubation, blood pressure control, and determination of risk/benefit for thrombolytic intervention.[10]
Patients presenting with Glasgow Coma Scale scores of 8 or less or rapidly decreasing Glasgow Coma Scale scores, require emergent airway control via intubation.
Differential Diagnosis
[edit | edit source]
Hypoglycemia and hyperglycemia need to be identified and treated early in the evaluation. Not only can both produce symptoms that mimic ischemic stroke, but they can also aggravate ongoing neuronal ischaemia.
Resources
[edit | edit source]
- Stroke Scales & Clinical Assessment Tools
- The Evidence-Based Review of Stroke Rehabilitation (EBRSR) is a comprehensive and up-to-date review available examining therapy-based (and also pharmacological) interventions associated with stroke rehabilitation. The review is updated regularly:
http://www.ebrsr.com/uploads/Executive-summary-SREBR-15.pdf
Recent Related Research (from Pubmed)[edit | edit source]
References[edit | edit source]
- ↑ Cal Shipley, M.D. What Is A Stroke? - Narration and Animation by Cal Shipley, M.D. Available from: http://www.youtube.com/watch?v=uLJewzJcCZ0 [last accessed 10/10/14]
- ↑ Global Burden of Stroke. The Atlas of Heart Disease and Stroke. MacKay J, Mensah GA. World Health Organization.
- ↑ Feigin VL, Lawes CM, Bennett DA, Anderson CS. Stroke epidemiology: a review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. Lancet Neurol. Jan 2003;2(1):43-53.
- ↑ Townsend N, Wickramasinghe K, Bhatnagar P, fckLRSmolina K, Nichols M, Leal J, Luengo-Fernandez R, fckLRRayner M (2012). Coronary heart disease statistics fckLR2012 edition. British Heart Foundation: London. P21
- ↑ USMLEFastTrack. Effects of Strokes - Middle Cerebral Artery. Available from: http://www.youtube.com/watch?v=6sk7AXNw9Ns [last accessed 10/10/14]
- ↑ USMLEFastTrack. Effects of Strokes - Posterior Cerebral Artery. Available from: http://www.youtube.com/watch?v=OFlL9Dm8qCM [last accessed 10/10/14]
- ↑ USMLEFastTrack. Effects of Strokes - Anterior Cerebral & Lateral Striate Artery. Available from: http://www.youtube.com/watch?v=NSWnNnfDt70 [last accessed 10/10/14]
- ↑ Lin JH, Hsu MJ, Hsu HW, Wu HC, Hsieh CL. Psychometric Comparisons of 3 Functional Ambulation Measures for Patients With Stroke. Stroke. 2010 Jul 29; online article ahead of print
- ↑ Harwood R, Huwez F, Good D. Stroke Care: A practical manual. New York: Oxford, 2011.
- ↑ Adams H, Adams R, Del Zoppo G, Goldstein LB. Guidelines for the early management of patients with ischemic stroke: 2005 guidelines update a scientific statement from the Stroke Council of the American Heart Association/American Stroke Association. Stroke. Apr 2005;36(4):916-23.