Spirometry: Difference between revisions
Kim Jackson (talk | contribs) m (Categorisation) |
No edit summary |
||
| (10 intermediate revisions by 3 users not shown) | |||
| Line 6: | Line 6: | ||
== Description == | == Description == | ||
[[Image:Spirometry1.jpg|thumb|right|300px]]Spirometry is one of the [[Pulmonary | [[Image:Spirometry1.jpg|thumb|right|300px]]Spirometry is one of the [[Pulmonary Function Test]]; they are useful investigations in the management of patients with respiratory disease or respiratory weakness secondary to neurological impairment. They aid diagnosis, help monitor response to treatment and can guide decisions regarding further treatment and intervention<ref name=":0">Ranu, H., Wilde, M., Madden, B. [https://scholar.google.com/scholar_url?url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3229853/&hl=en&sa=T&oi=gsb-ggp&ct=res&cd=0&d=11612805060986613558&ei=yraqZKauC5KcygSVpr24BA&scisig=ABFrs3yvOMa53IhPcaa0qAWvxfRz Pulmonary Function Tests]. The Ulster Medical Journal, 2011; 80(2), 84–90.</ref>. Spirometry can measure all the [[lung Volumes|lung volumes]] except residual volume. | ||
== | == Indications == | ||
*Investigation of patients with symptoms/signs/investigations that suggest pulmonary disease (e.g. cough, wheeze, breathlessness, crackles or abnormal [https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0062990/ chest x-ray]) | *Investigation of patients with symptoms/signs/investigations that suggest pulmonary disease (e.g. cough, wheeze, breathlessness, crackles or abnormal [https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0062990/ chest x-ray]) | ||
*Monitoring patients with known pulmonary disease for progression and response to treatment (e.g. [[Pulmonary Fibrosis|interstitial fibrosis]], [[COPD (Chronic Obstructive Pulmonary Disease)|COPD]], [[asthma]] or [https://www.webmd.com/lung/pulmonary-vascular-disease#1 pulmonary vascular disease]) | *Monitoring patients with known pulmonary disease for progression and response to treatment (e.g. [[Pulmonary Fibrosis|interstitial fibrosis]], [[COPD (Chronic Obstructive Pulmonary Disease)|COPD]], [[asthma]] or [https://www.webmd.com/lung/pulmonary-vascular-disease#1 pulmonary vascular disease]) | ||
*Investigation of patients with diseases that may have a respiratory complications (e.g. connective tissue disorders or neuromuscular diseases) | *Investigation of patients with diseases that may have a respiratory complications (e.g. connective tissue disorders or neuromuscular diseases) | ||
*Preoperative evaluation prior to lung resection, abdominal surgery or cardiothoracic surgery. | *Preoperative evaluation prior to [[Lung Anatomy|lung]] resection, abdominal surgery or cardiothoracic surgery. | ||
*Evaluating patients at risk of lung diseases (e.g. exposure to pulmonary toxins such a radiation, medication, or environmental or occupational exposure) | *Evaluating patients at risk of lung diseases (e.g. exposure to pulmonary toxins such a radiation, medication, or environmental or occupational exposure) | ||
*Surveillance following lung transplantation to assess for acute rejection, infection or obliterative bronchiolitis<ref name=":0" /> | *Surveillance following lung transplantation to assess for acute rejection, infection or obliterative [[bronchiolitis]]<ref name=":0" />. | ||
== Contraindications == | == Contraindications == | ||
* Aneurysm | * [[Aortic Aneurysm|Aneurysm]] | ||
* Haemoptysis of unknown origin | * Haemoptysis of unknown origin | ||
* [[Pneumothorax]] | * [[Pneumothorax]] | ||
| Line 24: | Line 24: | ||
*Recent thoracic or abdominal surgical procedures | *Recent thoracic or abdominal surgical procedures | ||
*Eye surgery | *Eye surgery | ||
*Pleural | *[[Pleural Effusion]] | ||
*Post-MI.<ref name=":0" /><ref> | *Post-[[Myocardial Infarction|MI]].<ref name=":0" /><ref>Cooper BG. [https://scholar.google.com/scholar_url?url=https://academic.oup.com/pmj/article-abstract/87/1032/724/7031948&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=9454804651345072600&ei=97aqZPLbPPGB6rQPlNyeqA4&scisig=ABFrs3yOi8hulJTP1UYJe7lP7n6N An update on contraindications for lung function testing]. Thorax. 2011 Aug;66(8):714-23.</ref><ref name=":1">Moore VC. [https://scholar.google.com/scholar_url?url=https://breathe.ersjournals.com/content/8/3/232%3Ffbclid%3DIwAR2v3kybw5gvOyBNb38xZgRGYp83JQawfmkx0I5lofWiowyNkr6pnpI_cBY%26utm_source%3DTrendMD%26utm_medium%3Dcpc%26utm_campaign%3D_Breathe_TrendMD_1&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=6175044291822125407&ei=G7eqZI6XCcWO6rQP_Yao8AU&scisig=ABFrs3yttgUNxK60fDfkmqJ8E5Ay Spirometry: step by step]. Breathe. 2012; 8(3):232-40.</ref> | ||
== Protocol == | == Protocol == | ||
=== Calibration === | === Calibration: === | ||
Before performing spirometry, the equipment used must be calibrated, or at least the calibration checked at the beginning of the session. Calibration procedures differ between | * Before performing spirometry, the equipment used must be calibrated, or at least the calibration checked at the beginning of the session. Calibration procedures differ between devices. Read the instructions associated with your spirometer for more information. Some meters need to be returned to the manufacturer for a repair if the calibration is out. It is considered optimal for spirometric values to be checked on a weekly basis using a biological control (a healthy person working in your team)<ref name=":1" />. | ||
=== Patient positioning === | === Patient positioning: === | ||
Correct measurement posture is as follows: | Correct measurement posture is as follows: | ||
*Upright sitting: there | *Upright sitting: there is a difference in the amount of air the patient can exhale from a sitting position compared to a standing position as long as they are sitting up straight and there are no restrictions<ref>Patel AK, Thakar HM. [https://scholar.google.com/scholar_url?url=https://www.researchgate.net/profile/Helee-Thakar/publication/276558853_Spirometric_Values_in_Sitting_Standing_and_Supine_Position/links/5c04c43045851523d159b4e9/Spirometric-Values-in-Sitting-Standing-and-Supine-Position.pdf&hl=en&sa=T&oi=gsb-ggp&ct=res&cd=0&d=8297341256533811317&ei=TreqZOHiNraJ6rQPusK_-AE&scisig=ABFrs3z6UyFptvbd8_cnuoZ3hOoO Spirometric Values in Sitting, Standing and Supine Position.] J Lung Pulm Respir Res. 2015; 2(1): 00026. </ref> and standing position is more better than supine lying<ref>Melam G, Buragadda S, Alhusaini A, Alghamdi M, Alghamdi M, Kaushal P. [https://scholar.google.com/scholar_url?url=https://www.jstage.jst.go.jp/article/jpts/26/4/26_jpts-2013-451/_article/-char/ja/&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=2234089388733835012&ei=dbeqZIODEqSK6rQPhqKGiAE&scisig=ABFrs3y-cSuajvJKRNvdJPiOUFh0 Effect of Different Positions on FVC and FEV1 Measurements of Asthmatic Patients.] Journal of physical therapy science.2014; 26(4) 591-593. 10.1589/jpts.26.591.</ref> | ||
*Feet flat on floor with legs uncrossed: no use of abdominal muscles for leg position. | *Feet flat on the floor with legs uncrossed: no use of abdominal muscles for leg position. | ||
*Loosen tight-fitting clothing | *Loosen tight-fitting clothing | ||
*Dentures normally left in: it is best to have some structure to the mouth area unless dentures are very loose. | *Dentures normally left in: it is best to have some structure to the mouth area unless dentures are very loose. | ||
*Use a chair with arms: when exhaling maximally, patients can become light-headed and possibly sway or faint. | *Use a chair with arms: when exhaling maximally, patients can become light-headed and possibly sway or faint. | ||
In the hospital setting, it may be impossible for your patient to sit in a chair, therefore, the position of the patient (usually supine) should be the same and documented for future testing | In the hospital setting, it may be impossible for your patient to sit in a chair, therefore, the position of the patient (usually supine) should be the same and documented for future testing<ref name=":1" />. | ||
=== Technique === | === Technique: === | ||
There are a number of different techniques for performing spirometry. However, most commonly the patient takes a deep breath in, as large as possible, and blows out as hard and as fast as possible and keeps going until there is no air left. PEF is obtained from the FEV1 and FVC | There are a number of different techniques for performing spirometry. However, most commonly the patient takes a deep breath in, as large as possible, and blows out as hard and as fast as possible and keeps going until there is no air left. PEF is obtained from the FEV1 and FVC maneuver. | ||
Encouragement makes a big difference, so don't be afraid to raise your voice to encourage the patient, particularly near the end of the | Encouragement makes a big difference, so don't be afraid to raise your voice to encourage the patient, particularly near the end of the maneuver. The patient needs to keep blowing until no more air comes out . Some patients, particularly those with obstructive disease, may find it difficult to exhale completely on a forced maneuver.<ref name=":1" /> | ||
=== Quality === | === Quality: === | ||
An acceptable | An acceptable maneuver is defined as follows: | ||
*An explosive start (no hesitation or sigmoid curve) with a back-extrapolation volume <150 mL (fig. 1)<ref name=":0" /> | *An explosive start (no hesitation or sigmoid curve) with a back-extrapolation volume <150 mL (fig. 1)<ref name=":0" /> | ||
*The | *The maneuver was performed with a maximal inspiration and expiration. | ||
*No glottis closure or cessation of airflow occurred during the | *No glottis closure or cessation of airflow occurred during the maneuver (e.g. by hesitation or blocking the mouthpiece). | ||
*No coughs (particularly during the first second), inspirations during the trace or evidence of leaks. | *No coughs (particularly during the first second), inspirations during the trace or evidence of leaks. | ||
The best FEV<sub>1</sub> and FVC can be taken from different | The best FEV<sub>1</sub> and FVC can be taken from different maneuvers. | ||
There can be problems with reproducibility: forced expiration can cause bronchoconstriction, so there must be ≥30 seconds between | There can be problems with reproducibility: forced expiration can cause bronchoconstriction, so there must be ≥30 seconds between maneuvers. For some patients, particularly [[Asthma|asthmatics]], several minutes may need to be left<ref name=":1" />. | ||
== Measurement definitions<ref name=":1" /> | == Measurement definitions == | ||
The definitions for the measurements are as follows<ref name=":1" />: | |||
{| class="wikitable" | {| class="wikitable" | ||
|Forced expiratory volume in one second (FEV<sub>1</sub>) | |Forced expiratory volume in one second (FEV<sub>1</sub>) | ||
| Line 80: | Line 81: | ||
{| width="100%" cellspacing="1" cellpadding="1" | {| width="100%" cellspacing="1" cellpadding="1" | ||
|- | |- | ||
| {{#ev:youtube|9VdHhD1vcDU|412}} | | {{#ev:youtube|9VdHhD1vcDU|412}} <ref>Armando Hasudungan Lung Function - Lung Volumes and Capacities Available from: https://www.youtube.com/watch?v=9VdHhD1vcDU. Accessed on 4/11/19</ref> | ||
| {{#ev:youtube|YwcNbVnHNAo|412}} | | {{#ev:youtube|YwcNbVnHNAo|412}}<ref>Armando Hasudungan Understanding Spirometry - Normal, Obstructive vs Restrictive Available from:https://www.youtube.com/watch?v=YwcNbVnHNAo. Accessed on 4/11/19.</ref> | ||
|} | |} | ||
{| width="100%" cellspacing="1" cellpadding="1" | {| width="100%" cellspacing="1" cellpadding="1" | ||
|- | |- | ||
| {{#ev:youtube|6kbgZWS5wH0|412}} | | {{#ev:youtube|6kbgZWS5wH0|412}}<ref>The European Lung Foundation Spirometry: how to take a lung function test Available from: https://www.youtube.com/watch?time_continue=4&v=6kbgZWS5wH0 Accessed on 4/11/19</ref> | ||
| {{#ev:youtube|78vfDmufbVU|412}} | | {{#ev:youtube|78vfDmufbVU|412}}<ref>CANVent Ottawa Pulmonary Function Assessment in Neuromuscular Diseases and Spinal Cord Injury Available from:https://www.youtube.com/watch?v=78vfDmufbVU Accessed on 4/11/19</ref> | ||
|} | |} | ||
| Line 96: | Line 97: | ||
[[Category:Cardiopulmonary]] | [[Category:Cardiopulmonary]] | ||
[[Category:Respiratory]] | [[Category:Respiratory]] | ||
[[Category:Assessment and Examination | [[Category:Respiratory System - Assessment and Examination]] | ||
Latest revision as of 15:38, 9 July 2023
Original Editor - George Prudden
Top Contributors - George Prudden, Uchechukwu Chukwuemeka, Kim Jackson, Rucha Gadgil, Vidya Acharya, Admin and Chelsea Mclene
Description[edit | edit source]
Spirometry is one of the Pulmonary Function Test; they are useful investigations in the management of patients with respiratory disease or respiratory weakness secondary to neurological impairment. They aid diagnosis, help monitor response to treatment and can guide decisions regarding further treatment and intervention[1]. Spirometry can measure all the lung volumes except residual volume.
Indications[edit | edit source]
- Investigation of patients with symptoms/signs/investigations that suggest pulmonary disease (e.g. cough, wheeze, breathlessness, crackles or abnormal chest x-ray)
- Monitoring patients with known pulmonary disease for progression and response to treatment (e.g. interstitial fibrosis, COPD, asthma or pulmonary vascular disease)
- Investigation of patients with diseases that may have a respiratory complications (e.g. connective tissue disorders or neuromuscular diseases)
- Preoperative evaluation prior to lung resection, abdominal surgery or cardiothoracic surgery.
- Evaluating patients at risk of lung diseases (e.g. exposure to pulmonary toxins such a radiation, medication, or environmental or occupational exposure)
- Surveillance following lung transplantation to assess for acute rejection, infection or obliterative bronchiolitis[1].
Contraindications[edit | edit source]
- Aneurysm
- Haemoptysis of unknown origin
- Pneumothorax
- Unstable cardiovascular status, recent myocardial infarction or pulmonary embolism
- Acute disorders affecting test performance, such as nausea or vomiting
- Recent thoracic or abdominal surgical procedures
- Eye surgery
- Pleural Effusion
- Post-MI.[1][2][3]
Protocol[edit | edit source]
Calibration:[edit | edit source]
- Before performing spirometry, the equipment used must be calibrated, or at least the calibration checked at the beginning of the session. Calibration procedures differ between devices. Read the instructions associated with your spirometer for more information. Some meters need to be returned to the manufacturer for a repair if the calibration is out. It is considered optimal for spirometric values to be checked on a weekly basis using a biological control (a healthy person working in your team)[3].
Patient positioning:[edit | edit source]
Correct measurement posture is as follows:
- Upright sitting: there is a difference in the amount of air the patient can exhale from a sitting position compared to a standing position as long as they are sitting up straight and there are no restrictions[4] and standing position is more better than supine lying[5]
- Feet flat on the floor with legs uncrossed: no use of abdominal muscles for leg position.
- Loosen tight-fitting clothing
- Dentures normally left in: it is best to have some structure to the mouth area unless dentures are very loose.
- Use a chair with arms: when exhaling maximally, patients can become light-headed and possibly sway or faint.
In the hospital setting, it may be impossible for your patient to sit in a chair, therefore, the position of the patient (usually supine) should be the same and documented for future testing[3].
Technique:[edit | edit source]
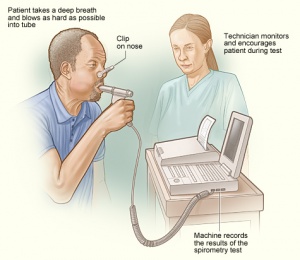
There are a number of different techniques for performing spirometry. However, most commonly the patient takes a deep breath in, as large as possible, and blows out as hard and as fast as possible and keeps going until there is no air left. PEF is obtained from the FEV1 and FVC maneuver.
Encouragement makes a big difference, so don't be afraid to raise your voice to encourage the patient, particularly near the end of the maneuver. The patient needs to keep blowing until no more air comes out . Some patients, particularly those with obstructive disease, may find it difficult to exhale completely on a forced maneuver.[3]
Quality:[edit | edit source]
An acceptable maneuver is defined as follows:
- An explosive start (no hesitation or sigmoid curve) with a back-extrapolation volume <150 mL (fig. 1)[1]
- The maneuver was performed with a maximal inspiration and expiration.
- No glottis closure or cessation of airflow occurred during the maneuver (e.g. by hesitation or blocking the mouthpiece).
- No coughs (particularly during the first second), inspirations during the trace or evidence of leaks.
The best FEV1 and FVC can be taken from different maneuvers.
There can be problems with reproducibility: forced expiration can cause bronchoconstriction, so there must be ≥30 seconds between maneuvers. For some patients, particularly asthmatics, several minutes may need to be left[3].
Measurement definitions[edit | edit source]
The definitions for the measurements are as follows[3]:
| Forced expiratory volume in one second (FEV1) | The volume of air that is forcibly exhaled after full inspiration in the first second. |
| Forced vital capacity (FVC) | The volume of air that is forcibly exhaled after full inspiration. |
| The ratio of the two volumes (FEV1/FVC) | This calculation allows the identification of obstructive or restrictive ventilatory defects. FEV1/FVC <70% where FEV1 is reduced more than FVC suggests an obstructive pathology. FEV1/FVC >70% where FVC is reduced more so than FEV1 is seen in restrictive pathology. |
| Vital capacity (VC) | The maximum amount of air that can be exhaled when blowing out as fast as possible |
| Peak expiratory flow (PEF) | The maximal flow that can be exhaled when blowing out at a steady rate |
Resources[edit | edit source]
| [6] | [7] |
| [8] | [9] |
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Ranu, H., Wilde, M., Madden, B. Pulmonary Function Tests. The Ulster Medical Journal, 2011; 80(2), 84–90.
- ↑ Cooper BG. An update on contraindications for lung function testing. Thorax. 2011 Aug;66(8):714-23.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Moore VC. Spirometry: step by step. Breathe. 2012; 8(3):232-40.
- ↑ Patel AK, Thakar HM. Spirometric Values in Sitting, Standing and Supine Position. J Lung Pulm Respir Res. 2015; 2(1): 00026.
- ↑ Melam G, Buragadda S, Alhusaini A, Alghamdi M, Alghamdi M, Kaushal P. Effect of Different Positions on FVC and FEV1 Measurements of Asthmatic Patients. Journal of physical therapy science.2014; 26(4) 591-593. 10.1589/jpts.26.591.
- ↑ Armando Hasudungan Lung Function - Lung Volumes and Capacities Available from: https://www.youtube.com/watch?v=9VdHhD1vcDU. Accessed on 4/11/19
- ↑ Armando Hasudungan Understanding Spirometry - Normal, Obstructive vs Restrictive Available from:https://www.youtube.com/watch?v=YwcNbVnHNAo. Accessed on 4/11/19.
- ↑ The European Lung Foundation Spirometry: how to take a lung function test Available from: https://www.youtube.com/watch?time_continue=4&v=6kbgZWS5wH0 Accessed on 4/11/19
- ↑ CANVent Ottawa Pulmonary Function Assessment in Neuromuscular Diseases and Spinal Cord Injury Available from:https://www.youtube.com/watch?v=78vfDmufbVU Accessed on 4/11/19