Spinal cord anatomy
Original Editor - Naomi O'Reilly
Top Contributors - Naomi O'Reilly, Lucinda hampton, Kim Jackson, Nikhil Benhur Abburi, Vidya Acharya, Admin, Tarina van der Stockt, Aminat Abolade, Rucha Gadgil, Jess Bell and Ewa Jaraczewska
Introduction[edit | edit source]
The spinal cord is part of the central nervous system and consists of a tightly packed column of nerve tissue that extends downwards from the brainstem through the central column of the spine. It is a relatively small bundle of tissue (weighing 35g and just about 1cm in diameter) but is crucial in facilitating our daily activities.
The spinal cord carries nerve signals from the brain to other parts of the body (importantly the muscles we use to move) and receives sensory input from the body, partially processes it, and then transmits that information to the brain.
Along with its role in relaying motor and sensory signals between the brain and periphery, the spinal cord also provides separate neural circuits for many of our reflexes. Some reflexes eg the knee-jerk are built into the nervous system and bypass the brain, while others can be learned over time.
Spinal Cord: External[edit | edit source]
Externally, the spinal cord is protected by 33 vertebrae, which sit between a semi-rigid intervertebral disk, which provide a level of flexibility to the vertebral column. Its flexibility is greatest in the cervical region and lowest in the thoracic region. The spinal cord (similar to the brain) is protected by three layers of meninges (membranes).
The vertebrae (in adults) are arranged in five regions, which provide support and protection for the spinal cord. It consists of seven Cervical Vertebrae, twelve Thoracic Vertebrae, five Lumbar Vertebrae, five Sacral (fused in adults to form the sacrum) and four Coccygeal Vertebrae (fused to form the coccyx).[1]
Spinal Cord: Internal[edit | edit source]
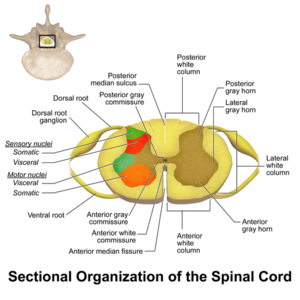
Inside, the spinal cord consists of grey matter and white matter.
The grey matter takes on the shape of a butterfly, with four 'wings' called horns: The horns in the front contain motor neurons; the horns in the back contain sensory neurons which carry sensory information.
The spinal cord grey matter is surrounded by a column of white matter, containing axons that allow different parts of the spinal cord to communicate smoothly, with signals passing upwards and downwards conveying eg sensation and motor signals.
Spinal Canal[edit | edit source]
Formed by the vertebral foramina of the vertebral bodies the spinal canal [bound anteriorly by the vertebral bodies and posteriorly by the laminae (vertebral arches)] with reinforcement at the walls through the intervertebral disks and the anterior and posterior longitudinal ligaments. The diameter varies from 12 to 22 mm in the cervical region and from 22 to 25 mm in the lumbar region.
Contains:
- Spinal cord
- Meninges
- Blood vessels
- Spinal nerve roots and surrounding fatty and connective tissues. [3][1]
Spinal Cord[edit | edit source]
The spinal cord is the major conduit and reflex centre between the peripheral nerves and the brain and transmits motor information from the brain to the muscles, tissues and organs, and sensory information from these areas back to the brain. [4] It is, in an adult, approximately 45 cm long, cylindrical and slightly flattened anteriorly and posteriorly. The spinal cord consists of grey matter and white matter. [3]
- The grey matter takes on the shape of a butterfly, with four 'wings' called horns: The horns in the front contain motor neurons; the horns in the back contain sensory neurons which carry sensory information.
- The white matter surrounds the grey column, containing axons that allow different parts of the spinal cord to communicate smoothly, with signals passing upwards and downwards conveying eg sensation and motor signals.
- The spinal cord lies within the vertebral canal, extending from the foramen magnum to the lowest border of the first lumbar vertebra. It is enlarged at two sites, the cervical and lumbar region.
- Its upper end is continuous with the medulla, the transition is defined to occur just above the level of exit of the first pair of cervical nerves.
- Its tapering lower end, the conus medullaris, terminates at the level of the L3 vertebra in neonates, and at the level of the L1-2 intervertebral disk in adults.
- The conus medullaris is continuous at its lower end with the threadlike filum terminale, composed mainly of glial and connective tissue, which, in turn, runs through the lumbar sac amidst the posterior and anterior roots of the spinal nerves, collectively called the Cauda Equina (“horse’s tail”), and then attaches to the dorsal surface of the coccyx. [1]
Sensory Nerve Fibres enter the Spinal Cord via the Posterior (Dorsal) Root. The cell bodies for these neurons are situated in the Dorsal Root Ganglia. Motor and Preganglionic Autonomic Fibres exit via the Anterior (Ventral) Root.
Spinal Nerves[edit | edit source]
Emerging from the spinal cord are 31 pairs of anterior and posterior nerve roots. The cervical, thoracic, lumbar, and sacral portions of the spinal cord are defined according to the segmental division of the vertebral column and spinal nerves. There are eight cervical*, twelve thoracic, five lumbar, five sacral and one coccygeal. At each level an anterior pair of nerve roots carries motor nerves, while a posterior pair of nerve roots carries only sensory nerves. The anterior and posterior roots join to form two spinal nerves, one on either side of the spine, which then exit the vertebral canal through the intervertebral foramina. Once outside the intervertebral foramina they form peripheral nerves. [1]
*While there are eight pairs of cervical spinal nerves there are only seven cervical vertebrae. This disparity occurs because the first pair of cervical spinal nerves exits above the first cervical vertebra just below the skull. However, the eighth pair of cervical spinal nerves exits below the last cervical vertebra.* [3]
Muscle Innervation[edit | edit source]
Upper Limb [7][edit | edit source]
Lower Limb [7][edit | edit source]
| Joint | Movement | Muscles | Innervation | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| L1 | L2 | L3 | L4 | L5 | S1 | S2 | S3 | |||
| Hip | Flexion | Psoas Major | X | X | O | |||||
| Iliacus | X | O | ||||||||
| Pectineus | X | O | ||||||||
| Rectus Femoris | O | X | X | |||||||
| Adductor Longus | X | X | O | |||||||
| Sartorius | O | O | ||||||||
| Extension | Gluteus Maximus | X | X | O | ||||||
| Adductor Magnus | X | X | O | |||||||
| Semimembranosus | O | X | O | |||||||
| Semitendinosus | O | X | O | |||||||
| Biceps Femoris | O | X | O | |||||||
| Internal Rotation | Iliacus | X | O | |||||||
| Gluteus Medius | X | X | O | |||||||
| Gluteus Minimus | X | X | O | |||||||
| Tensor Fascia Latae | X | X | O | |||||||
| External Rotation | Superior Gemelli | O | O | |||||||
| Inferior Gemelli | O | O | ||||||||
| Quadratus Femoris | O | O | ||||||||
| Piriformis | O | X | O | |||||||
| Obturator Internus | O | X | ||||||||
| Obturator Externus | O | X | ||||||||
| Sartorius | O | O | ||||||||
| Adduction | Gracilis | X | O | |||||||
| Adductor Longus | X | X | O | |||||||
| Adductor Magnus | X | X | O | |||||||
| Pectineus | X | O | ||||||||
| Abduction | Tensor Fascia Latae | X | X | O | ||||||
| Gluteus Medius | X | X | O | |||||||
| Gluteus Minimus | X | X | O | |||||||
| Piriformis | O | X | O | |||||||
| Knee | Flexion | Semimembranosus | O | X | O | |||||
| Semitendinosus | O | X | O | |||||||
| Biceps Femoris | O | X | O | |||||||
| Gastrocnemius | O | O | ||||||||
| Extension | Rectus Femoris | O | X | X | ||||||
| Vastus Lateralis | O | X | X | |||||||
| Vastus Intermedius | O | X | X | |||||||
| Vastus Medialis | O | X | X | |||||||
| Ankle | Dorsiflexion | Tibialis Anterior | X | O | ||||||
| Extensor Digitorum Longus | X | O | ||||||||
| Extensor Hallucis Longus | X | O | ||||||||
| Peroneus Tertius | O | O | ||||||||
| Plantarflexion | Gastrocnemius | O | O | |||||||
| Soleus | O | O | ||||||||
| Flexor Digitorum Longus | O | X | X | |||||||
| Flexor Hallucis Longus | O | X | X | |||||||
| Peroneus Longus | O | O | ||||||||
| Tibialis Posterior | O | O | ||||||||
| Inversion | Tibialis Anterior | X | O | |||||||
| Tibialis Posterior | O | O | ||||||||
| Eversion | Peroneus Longus | O | O | |||||||
| Peroneus Brevis | O | O | ||||||||
| Peroneus Tertius | O | O | ||||||||
| Toes | Flexion | Flexor Digitorum Longus | O | X | X | |||||
| Flexor Hallucis Longus | O | X | X | |||||||
| Flexor Hallucis Brevis | O | O | ||||||||
| Flexor Digitorum Brevis | O | O | ||||||||
| Flexor Digitorum Accessorius | O | O | ||||||||
| Flexor Digiti Minimi Brevis | O | O | ||||||||
| Abductor Hallucis | O | O | ||||||||
| Abductor Digiti Minimi | O | O | ||||||||
| Lumbricals | O | O | O | |||||||
| Extension | Extensor Digitorum Longus | X | O | |||||||
| Extensor Digitorum Brevis | O | O | ||||||||
| Extensor Hallucis Longus | X | O | ||||||||
| Abduction | Abductor Hallucis | O | O | |||||||
| Abductor Digiti Minimi | O | O | ||||||||
| Dorsal Interossei | O | O | ||||||||
| Adduction | Plantar Interossei | O | O | |||||||
| Adductor Hallucis | O | O | ||||||||
X - Main Nerves Innervating Muscle
O - Accessory Nerves Innervating Muscle
Spinal Motorneurons[edit | edit source]
Alpha and Gamma motor neurons are both found in the anterior (ventral) horn.
- Alpha motor neurons are the largest motor neurons in the nervous system and innervate skeletal muscle.
- Gamma Motorneurons innervate intrafusal muscle fibres of the muscle spindle.
Motor neurons are arranged somatotopically across the anterior horn. The more medially placed motor neurons innervate proximal muscles while laterally placed motor neurons innervate distal muscles. [3][1]
Blood Supply[edit | edit source]
The majority of the spinal cord blood supply is provided by the segmental spinal arteries, with further supply coming from the vertebral arteries via a single anterior spinal artery and paired posterior spinal arteries. The segmental and spinal arteries are linked by numerous anastomoses. [3][1]
Segmental Arteries[edit | edit source]
The segmental arteries give off radicular branches, cervical and thoracolumbar, which enter the intervertebral foramen and supply the anterior and posterior roots and spinal ganglion of the corresponding level. The spinal cord itself is supplied by unpaired medullary arteries that originate from segmental arteries. [3][1]
Spinal Arteries[edit | edit source]
The spinal arteries, arising from the vertebral artery, run longitudinally down the spinal cord. The unpaired anterior spinal artery lies in the anterior median fissure of the spinal cord and extends from the level of the lower brainstem to the tip of the conus medullaris, with the diameter steadily increasing below the T2 level. It supplies the ventral medial surface of the medulla and anterior 2/3 of the spinal cord. The paired posterior spinal arteries supply the dorsal columns and the all but the base of the dorsal horns bilaterally. There are reinforcing branches from other arteries along the length of the cord and numerous anastomoses of the spinal arteries produce a vasocorona around the spinal cord. If occlusion occurs, it is normally of the anterior spinal artery, producing loss of power and spinothalamic sensory deficit, but dorsal column sensory capabilities are maintained. [3][1]
Spinal Veins[edit | edit source]
Blood from within the spinal cord travels through the intramedullary veins, to the anterior and posterior spinal veins, which form a reticulated network in the pia mater around the circumference of the cord throughout its length. The anterior two-thirds of the gray matter drain via the anterior spinal vein, while the posterior and lateral spinal veins drain the rest of the spinal cord. These vessels empty by way of the radicular veins into the external and internal vertebral venous plexuses, groups of valveless veins that extend from the coccyx to the base of the skull. The vertebral and deep cervical veins drain venous blood from the cervical spine into the superior vena cava; the posterior intercostal and lumbar veins drain venous supply from the thoracic and lumbar spine into the azygos and hemiazygos veins; and the median and lateral sacral veins drain venous supply from the sacrum into the common iliac vein. [3][1]
Associated Pathways[edit | edit source]
Ascending Sensory Pathway[edit | edit source]
Information detected by sensory receptors in the periphery is transmitted along ascending neural tracts in the spinal cord. Located in the white matter of the spinal cord, the ascending sensory tracts arise from either the the cells of the spinal ganglia or the intrinsic neurons within the grey matter that receive primary sensory input. There are many sensory tracts and pathways carrying different types of sensory information from the periphery to the cerebral cortex. In humans the major sensory pathways include:
- Spinothalamic Tract - The spinothalamic tracts sit within the dorsal horn laminae I,III,IV,V of the spinal cord. Most of the fibres cross the midline at or near the level they enter the spinal cord. The lateral spinothalamic tract carries information about pain and temperature, and the anterior spinothalamic tract carries information about crude touch.
- Dorsal Column or Medial Lemniscal Pathway - The largest ascending tract, the fasciculi gracilis and cuneatus, arise from the spinal ganglion cells and ascend in the dorsal funiculus to the medulla oblongata. The gracile and cuneate tracts carry information about proprioception and light touch. The gracile tract is positioned medially and predominantly carries sensory fibres from the lower body below T6, while the cuneate tract is positioned laterally and predominantly carries fibres from the upper body above T6. The fibres within the gracile and cuneate tracts cross completely in the brainstem and form the medial lemniscus, which in turn projects to the anterior basal nuclear complex of the thalamus. Conveys proprioception, light touch and vibration.
- Spinocerebellar Tract - From spinal cord interneurons. It has two tracts a) Posterior Spinocerebellar Tract, which relays via inferior cerebellar peduncle and b) Anterior Spinocerebellar Tract relays via superior cerebellar peduncle to the cerebellum. It conveys proprioceptive information and on-going activity in the spinal cord interneurons.
Descending Motor Pathways[edit | edit source]
The descending pathways, convey the motor commands and are involved in the control of movement. In humans, the major motor pathways include:
Corticospinal (Pyramidal) Tract[edit | edit source]
Extrapyramidal and Pyramidal tracts
Carries information from the cerebral cortex to the spinal cord. Also called the pyramidal tract as it is the only point where all the fibres are collected together without contamination by other fibre tracts in the medullary pyramids of the brain stem. Primary motor cortex is the main source of input to this tract, but the premotor and supplementary motor cortex also contribute fibres. Its projections are primarily contralateral and have a strong influence on the activity of groups of spinal motoneurones, which innervate distal muscles of the hands and feet. Most of the fibers, approximately 85%, cross the midline in the decussation of the pyramids in the brain stem and then descend through the spinal cord in the lateral corticospinal tract, while the other 15% cross within the spinal cord at the level they terminate and are carried within the medial corticospinal tract. According to Harvey (2008), the cervical upper motor neurons are centrally located within the corticospinal tract while the lumbar and sacral neurons are peripherally located, which explains neurological patterns of loss seen with certain types of incomplete spinal cord injuries where the peripheral rim of the spinal cord is undamaged. [7]
Reticulospinal Tract[edit | edit source]
This tract begins in the caudal reticular formation in the pons and medulla. The fibres from the medullary portion descend in the dorsolateral funiculus of the cord near the corticospinal fibres, whereas the fibres from the pontine region travel in the ventromedial portion of the spinal cord. These pathways are predominantly bilateral and have the largest density of projections to axial and proximal muscles. Provides both excitable and inhibitory effects on the interneurons in the spinal cord, and to a lesser extent, it also acts on the motor neurons. Its main action is to dampen down activity in the spinal cord. without this pathway, there is increased extensor tone observed. [7]
Vestibulospinal Tract[edit | edit source]
Originates from Deiters nucleus in the medulla and innervates the extensor and axial muscles. The vestibulospinal tracts receive limited input from the cortical motor areas as they arise in the vestibular nuclei, which receive main input from the balance organs of the ear. Their projections to the spinal cord are mostly bilateral and to proximal and axial muscles. It is involved in balance control and posture. [7]
Rubrospinal Tract[edit | edit source]
Originates from the magnocellular part of the red nucleus in the brain. It projects towards common structures with the CoST, particularly those involved with distal motor control. There is debate as to how significant this tract is in humans, is quite prominent in the cat. [7]
Autonomic Pathways[edit | edit source]
Autonomic nerves are also carried by the spinal cord. Sympathetic nerves exit the vertebral canal via thoraco-lumbar spinal nerves, and parasympathetic nerves exit via sacral spinal nerves. As a result individuals with a cervical lesion lose supraspinal control of the entire sympathetic nervous system and of the sacral part of the parasympathetic nervous system. Individuals with thoracic, lumbar or sacral lesions lose varying amounts of supraspinal control of the sympathetic and parasympathetic nervous system as determined by the level of the lesion. Some parasympathetic fibres are carried within cranial nerves and are unaffected by spinal cord injury. [7]
| [8] |
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Rohkamm Reinhard. Color Atlas of Neurology. Thieme; 2014 Sep 2.
- ↑ Spinal Cord. Blausen Medical. Retrieved on 26 January 2016.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 Moore KL, Agur AM, Dalley AF. Essential Clinical Anatomy. Philadelphia: Lippincott Williams & Wilkins; 2002 Mar.
- ↑ Francisco de Assis Aquino Gondim et al., Topographic and Functional Anatomy of the Spinal Cord, Medshape, 2015
- ↑ Designed by Freepik at http://www.freepik.com
- ↑ Spinal Cord. Blausen Medical. Retrieved on 26 January 2016.
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 Harvey L. Management of Spinal Cord Injuries: A Guide for Physiotherapists. Elsevier Health Sciences; 2008 Jan 10
- ↑ Handwritten tutorials. Spinal Pathways 1 - Spinal Cord Anatomy and Organisation. Available from: http://www.youtube.com/watch?v=5B87zsAKmWc [last accessed 29/08/16]
![Spinal Column [5]](/images/thumb/7/74/42282-O3EL6G.jpg/400px-42282-O3EL6G.jpg)
![Spinal Cord Sectional Anatomy [6]](/images/thumb/a/ad/Spinal_Cord_Sectional_Anatomy.png/400px-Spinal_Cord_Sectional_Anatomy.png)






