Snapping Hip and Trochanteric Bursitis: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) m (Text replacement - "[[Extracorporeal Shockwave Therapy (ESWT)" to "[[Extracorporeal Shockwave Therapy ") |
||
| (16 intermediate revisions by 5 users not shown) | |||
| Line 6: | Line 6: | ||
== Snapping Hip Syndrome (SHS) == | == Snapping Hip Syndrome (SHS) == | ||
Three types of [[Snapping Hip Syndrome|snapping hip syndrome]] have been identified: external, internal, and intra-articular types, with the external type being the most common.<ref>Radiopedia Snapping hip syndrome Available:https://radiopaedia.org/articles/snapping-hip-syndrome?lang=us (accessed 30/10.2022)</ref> | |||
=== External Snapping Hip Syndrome (ESHS) === | === External Snapping Hip Syndrome (ESHS) === | ||
External (lateral) snapping hip is a painful condition also known as lateral coxa saltans | External (lateral) snapping hip is a painful condition (also known as lateral coxa saltans), occurring in about 10% of the general population.<ref name=":2">Randelli F, Mazzoleni MG, Fioruzzi A, Giai Via A, Calvisi V, Ayeni OR. [https://link.springer.com/article/10.1007/s00167-020-06305-w#citeas Surgical interventions for external snapping hip syndrome]. Knee Surg Sports Traumatol Arthrosc. 2021 Aug;29(8):2386-2393. </ref> | ||
* ''External extra-articular'' snapping is caused either by the posterior [[Iliotibial Band Syndrome|iliotibial band]] or the anterior aspect of the [[Gluteus Maximus|gluteus maximus]] as they move over the greater trochanter during hip flexion / extension or hip internal / external rotation.<ref name=":0">Yen YM, Lewis CL, Kim YJ. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4961351/pdf/nihms721941.pdf Understanding and Treating the Snapping Hip]. Sports Med Arthrosc Rev. 2015 Dec;23(4):194-9. </ref> This may lead to the inflammation of the trochanteric bursa.<ref name=":0" /> | |||
* Individuals with the ESHS may also have [[Coxa Vara / Coxa Valga|coxa vara]], fibrotic scar tissue, a prominent greater trochanter, smaller lateral pelvic width, or have had surgery in the past for anterolateral knee instability.<ref name=":1">Idjadi J, Meislin R. Symptomatic snapping hip: targeted treatment for maximum pain relief. The Physician and Sportsmedicine 2004;32(1):25-31.</ref><ref>Byrd JT. [http://www.iortho.com.my/media/members032010_docs/sports/hip/snapping_hip.pdf Snapping hip.] Operative Techniques in Sports Medicine 2005;13(1):46-54.</ref> | |||
=== Internal Snapping Hip Syndrome (ISHS) === | === Internal Snapping Hip Syndrome (ISHS) === | ||
''Internal'' ''extra-articular'' snapping is caused by the iliopsoas tendon | ''Internal'' ''extra-articular'' snapping is caused by the [[iliopsoas]] tendon snapping over the iliopectinal eminence or the femoral head and is more likely to occur while the hip flexors are contracting. Other proposed ''extra-articular'' mechanisms of this condition include:<ref name=":0" /> | ||
* | * Accessory iliopsoas tendon slips | ||
* | * Iliopsoas snapping over a ridge at the lesser trochanter | ||
* | * Snapping of the [[iliofemoral ligament]] over the femoral head | ||
* | * Subluxation of the long head of the [[Biceps Femoris|biceps]] at the [[ischium]] | ||
* | * Snapping at the [[Pelvic Landmarks|anterior inferior iliac spine]].<ref name=":0" /> | ||
=== Intra-Articular Snapping Hip === | === Intra-Articular Snapping Hip === | ||
'' | ''Intra-articular'' factors can also lead to the development of snapping hip symptoms, including labral tears, ligamentum teres (ligament of the head of the femur) tears, loose bodies such as osteochondral fragments, or joint instability. | ||
==== Clinically Relevant Anatomy ==== | ==== Clinically Relevant Anatomy ==== | ||
| Line 27: | Line 30: | ||
===== Iliotibial Band ===== | ===== Iliotibial Band ===== | ||
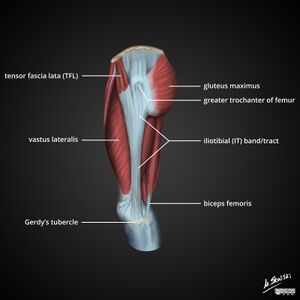
The [[Iliotibial Band Syndrome|iliotibial band]] (ITB) is a thick band of fascia that runs on the lateral side of the thigh from the iliac crest and inserts at the knee.<ref>Baker RL, Fredericson M. Iliotibial Band Syndrome in Runners: Biomechanical Implications and Exercise Interventions. Physical médicine and réhabilitation clinics of North America, 2016; 27(1):53-77</ref> It is composed of dense fibrous connective tissue that originates from the anterior fibres of the tensor fasciae late and the posterior fibres of the gluteus maximus. After running down on the lateral thigh | The [[Iliotibial Band Syndrome|iliotibial band]] (ITB) is a thick band of fascia that runs on the lateral side of the thigh from the iliac crest and inserts at the knee.<ref>Baker RL, Fredericson M. Iliotibial Band Syndrome in Runners: Biomechanical Implications and Exercise Interventions. Physical médicine and réhabilitation clinics of North America, 2016; 27(1):53-77</ref> It is composed of dense fibrous connective tissue that originates from the anterior fibres of the tensor fasciae late and the posterior fibres of the gluteus maximus. After running down on the lateral thigh most of its fibres insert onto the tibial tubercle, some insert into the gluteus maximum tendon, the lateral femoral epicondyle and distal lateral border of the patella.<ref name=":2" /> During hip flexion, the ITB moves anterior to the greater trochanter and during hip extension it runs posterior to it.<ref name=":0" /> | ||
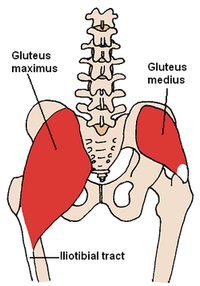
On the lateral aspect of the hip joint, there are three subgluteal bursae: greater trochanter bursa, subgluteus medius bursa, | On the lateral aspect of the hip joint, there are three subgluteal bursae: greater trochanter bursa, subgluteus medius bursa, and subgluteus minimus bursa. The trochanteric bursa is the largest of the three and it covers the insertion of the gluteus medius tendon and the posterior aspect of the greater trochanter. Its primary role is to reduce friction between the tendons of the gluteus medius and the ITB when they pass over the greater trochanter.<ref>Weerakkody, Y., Bell, D. [https://radiopaedia.org/articles/hip-bursae-1 Hip bursae]. Reference article, Radiopaedia.org. (accessed on 13 Mar 2022) <nowiki>https://doi.org/10.53347/rID-64260</nowiki></ref> | ||
The iliotibial band | The iliotibial band is involved in hip stabilisation during single leg stance and ambulation when the band acts as a tendon of the [[Tensor Fascia Lata|tensor fasciae latae]] (TFL) and the [[Gluteus Maximus|gluteus maximus]]. The contraction of the gluteus maximus and the TFL muscles cause tightening of the band. | ||
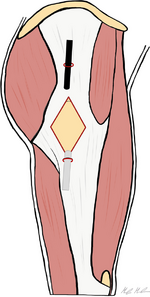
[[File:Gluteus Medius.PNG|thumb|alt=|286x286px]] | [[File:Gluteus Medius.PNG|thumb|alt=|286x286px]] | ||
===== Gluteus Maximus ===== | ===== Gluteus Maximus ===== | ||
[[Gluteus Maximus|Gluteus maximus]] originates at the outer slope of the dorsal segment of the iliac crest, the gluteal surface of the ilium, dorsal surface of the lower part of the sacrum, side of the coccyx, and the sacrotuberous ligament. It also shares its attachment to the thoracolumbar fascia with the ipsilateral [[Multifidus | [[Gluteus Maximus|Gluteus maximus]] originates at the outer slope of the dorsal segment of the iliac crest, the gluteal surface of the ilium, dorsal surface of the lower part of the sacrum, side of the coccyx, and the sacrotuberous ligament. It also shares its attachment to the thoracolumbar fascia with the ipsilateral [[Lumbar Multifidus|multifidus]] and contralateral [[Latissimus Dorsi Muscle|latissimus dorsi]]. The muscle inserts onto the gluteal tuberosity and the iliotibial band. | ||
Gluteus | Gluteus maximus is primarily involved in hip extension, external rotation and abduction. Its function is essential to maintain an erect posture. | ||
[[File:Iliopsoas Anatomy.png|thumb|alt=|403x403px]] | [[File:Iliopsoas Anatomy.png|thumb|alt=|403x403px]] | ||
===== Iliopsoas ===== | ===== Iliopsoas ===== | ||
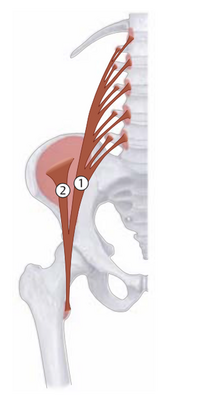
[[ | The [[iliopsoas]] muscle complex is made up of three muscles: [[iliacus]], [[Psoas Major|psoas major]] and [[Psoas Minor|psoas minor.]]<ref name=":0" /> It can work as a unit, but the three muscles all have separate functions. The iliopsoas originates at the fusion of the psoas major and iliacus muscles. This fusion occurs at the level of L5-S2, and the combined muscles pass from the pelvis to the thigh under the inguinal ligament. The iliopsoas muscle inserts into the lesser trochanter of the femur via the psoas tendon. | ||
The iliopsoas bursa is the largest bursa of the hip joint and is located deep to the iliopsoas musculotendinous junction and anterior to the hip joint capsule. The bursa | The iliopsoas bursa is the largest bursa of the hip joint and is located deep to the iliopsoas musculotendinous junction and anterior to the hip joint capsule. The bursa is believed to communicate with the hip joint in ~15% of patients. It helps the muscle glide and slide over the front of the hip during movement.<ref>Bordoni B, Varacallo M. [https://www.ncbi.nlm.nih.gov/books/NBK531508/ Anatomy, Bony Pelvis and Lower Limb, Iliopsoas Muscle.] [Updated 2021 Jul 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: <nowiki>https://www.ncbi.nlm.nih.gov/books/NBK531508/</nowiki></ref> | ||
The iliopsoas muscle is the strongest hip flexor and assists in | The iliopsoas muscle is the strongest hip flexor and assists in external rotation of the femur. It is essential for correct standing and sitting lumbar posture, and during walking and running. | ||
=== Pathophysiology === | === Pathophysiology === | ||
* External | * External snapping hip | ||
** | ** Visual component to the snap observed by the patient when the ITB slides from the ''anterior to posterior'' aspect of the greater trochanter during hip movement from ''extension to flexion.'' This is usually caused by the thickening of the posterior ITB and/or the anterior portion of the gluteus maximus.<ref name=":3">Walker P, Ellis E, Scofield J, Kongchum T, Sherman WF, Kaye AD. Snapping Hip Syndrome: A Comprehensive Update. Orthopaedic Reviews. 2021;13(2).</ref> | ||
* Internal | * Internal snapping hip | ||
** | ** Audible component to the snap when the movement of the iliopsoas tendon from the ''lateral to the medial'' position is restricted during hip ''extension and internal rotation''. This restriction can be caused by the femoral head or pectineal eminence of the pelvis.<ref name=":3" /> | ||
* Intra-articular | * Intra-articular snapping hip | ||
** | ** Pathological process of the hip joint when loose bodies, acetabular labral tears, or osteochondral fractures can interfere with the articulation of the femoral head into the acetabulum.<ref name=":3" /><br> | ||
=== Clinical Presentation === | === Clinical Presentation === | ||
Individuals with ''external snapping hip'' syndrome typically describe a sensation that feels like hip dislocation. With ''internal snapping hip,'' patients describe a feeling of the hip joint being "stuck" or locked and they report hearing the sound of snapping. The intermittent sound of clicking or catching characterises ''intra-articular'' pathology. | |||
Additionally patients may report: | Additionally patients may report: | ||
* | * Pain | ||
* | * Muscle weakness | ||
* | * Activity limitations<ref name=":1" /> | ||
=== Evaluation === | === Evaluation === | ||
==== Physiotherapy Assessment ==== | ==== Physiotherapy Assessment ==== | ||
The physiotherapy assessment includes the patient's history, physical examination and special tests. | |||
===== Patient's History ===== | ===== Patient's History ===== | ||
* symptoms | * Description of symptoms (location, sensation, timing and duration) | ||
* | * Impact on activities of daily living | ||
===== Physical Examination ===== | ===== Physical Examination ===== | ||
| Line 85: | Line 88: | ||
===== Special Tests ===== | ===== Special Tests ===== | ||
External | '''External snapping hip syndrome:''' | ||
* FADIR test including flexion, adduction and internal rotation or impingement | * FADIR test including flexion, adduction and internal rotation or impingement | ||
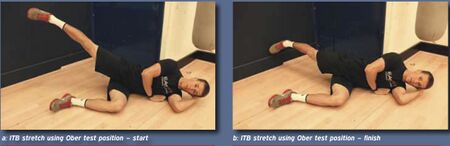
* [[Ober's Test|Ober's test]]: assessment of the ITB tightness<ref name=":10" /> | * [[Ober's Test|Ober's test]]: assessment of the ITB tightness<ref name=":10" /> | ||
| Line 93: | Line 96: | ||
Internal | '''Internal snapping hip syndrome:''' | ||
* Dynamic testing (loop-the-loop): starting at [[FABER Test|FABER]] (flexion, abduction and external rotation) | * Dynamic testing (loop-the-loop): starting at [[FABER Test|FABER]] (flexion, abduction and external rotation) position and moving into EADIR (extension, adduction and internal rotation) position. Positive test: snapping of the iliopsoas tendon<ref name=":11" /> | ||
*[[Thomas Test|Thomas test]]: positive test indicates psoas contracture<ref name=":12" /> | *[[Thomas Test|Thomas test]]: positive test indicates psoas contracture<ref name=":12" /> | ||
* [https://www.physio-pedia.com/Snapping_Hip_Syndrome?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal#Examination Stinchfield Test]: The patient lies supine with the hip flexed at 30°. The patient is asked to fully flex the hip, while the | * [https://www.physio-pedia.com/Snapping_Hip_Syndrome?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal#Examination Stinchfield Test]: The patient lies supine with the hip flexed at 30°. The patient is asked to fully flex the hip, while the examiner applies a resistance force. Pain in the anterior groin indicates a positive test. | ||
| Line 110: | Line 113: | ||
==== Imaging ==== | ==== Imaging ==== | ||
* X-Ray: no typical findings indicative of coxa saltans interna on | * X-Ray: no typical findings indicative of coxa saltans interna on x-ray. Evidence of femoroacetabular impingement can be found on a plain X-ray.<ref name=":0" /> | ||
* MRI: not specific for | * MRI: not specific for iliopsoas involvement. May assist with the diagnosis of iliopsoas bursa or iliopsoas muscle inflammation. This modality helps to visualise a thickened ITB and focal thickening of the gluteus maximus when ESHS is suspected.<ref name=":0" /> | ||
* Ultrasound: | * Ultrasound: helps to visualise the dynamic motion of the iliopsoas tendon, but requires a skilled clinician to perform and interpret results.<ref name=":0" /><ref>Winston P, Awan R, Cassicy JD et al. Clinical examination and ultrasound of self-reported snapping hip syndrome in elite ballet dancers. Am J Sports Med. 2007;35:118-126.</ref> | ||
* Dynamic sonography: able to detect the movement of the ITB over the greater trochanter. | * Dynamic sonography: able to detect the movement of the ITB over the greater trochanter. | ||
* Iliopsoas bursography: under fluoroscopy bursa is filled with contrast to | * Iliopsoas bursography: under fluoroscopy, bursa is filled with contrast to visualise the tendon moving back and forth. This imaging is performed to confirm ISHS syndrome.<ref name=":0" /> | ||
=== Management / Interventions === | === Management / Interventions === | ||
[[File:ITB stretch.jpg|thumb| | [[File:ITB stretch.jpg|thumb|450x450px|Iliotibial Band stretch|alt=]] | ||
==== Conservative Management ==== | ==== Conservative Management ==== | ||
''Goal'': to improve pain, | ''Goal'': to improve pain, increase flexibility and equalise the limb length discrepancy if needed. | ||
A conservative approach should be continued for at least 6 months and the following strategies are recommended:<ref name=":2" />[[File:Iliopsoas stretch.jpg|thumb|Iliopsoas stretch]] | |||
# Rest, icing and anti-inflammatories should be advocated to reduce inflammation<ref name=":0" /> | # Rest, icing and anti-inflammatories should be advocated to reduce inflammation<ref name=":0" /> | ||
# Muscle tightness causing the snapping must be identified: passive and active stretching | # Muscle tightness causing the snapping must be identified: passive and active stretching programme specific to the ITB and the iliopsoas muscles to be initiated <ref name=":0" /> | ||
# Single | # Single leg stance exercises (ESHS)<ref name=":18" /> | ||
# Lateral walking with | # Lateral walking with theraband (ESHS)<ref name=":18" /> | ||
# Hip hiking exercises (ESHS)<ref name=":18" /> | # Hip hiking exercises (ESHS)<ref name=":18" /> | ||
# Movements that provoke the snap should be avoided | # Movements that provoke the snap should be avoided | ||
# Sports activities must be reduced | # Sports activities must be reduced | ||
# Active | # Active release techniques<ref name=":18">Spina AA. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1924651/ External coxa saltans (snapping hip) treated with Active Release Techniques: a case report]. J Can Chiropr Assoc. 2007 Mar;51(1):23-9.</ref> | ||
# Use of modalities: | # Use of modalities: laser therapy or [[Extracorporeal Shockwave Therapy |extracorporeal shockwave therapy ESWT]]<ref>Frizziero A, Vittadini F, Pignataro A, Gasparre G, Biz C, Ruggieri P, Masiero S. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5193517/pdf/281-292.pdf Conservative management of tendinopathies around hip]. Muscles Ligaments Tendons J. 2016 Dec 21;6(3):281-292. </ref> | ||
[[File:ITB release technique.png|thumb| | [[File:ITB release technique.png|thumb|297x297px|<small>''Ilizaliturri’s ITB release technique. Adapted from: Randelli F, Mazzoleni MG, Fioruzzi A, Giai Via A, Calvisi V, Ayeni OR. Surgical interventions for external snapping hip syndrome.''</small> |alt=]] | ||
==== Surgical Intervention ==== | ==== Surgical Intervention ==== | ||
''Goal'': to release the contracted ITB or the iliopsoas to resolve the snap<ref>Pierce TP, Kurowicki J, Issa K, Festa A, Scillia AJ, McInerney VK. External snapping hip: a systematic review of outcomes following surgical intervention: External snapping hip systematic review. Hip Int. 2018 Sep;28(5):468-472. </ref> | ''Goal'': to release the contracted ITB or the iliopsoas to resolve the snap<ref>Pierce TP, Kurowicki J, Issa K, Festa A, Scillia AJ, McInerney VK. External snapping hip: a systematic review of outcomes following surgical intervention: External snapping hip systematic review. Hip Int. 2018 Sep;28(5):468-472. </ref> | ||
External | '''External snapping hip:''' | ||
# Fractional lengthening of the tendon | # Fractional lengthening of the tendon | ||
| Line 144: | Line 147: | ||
The lengthening procedures include: Z-shaped release, formal Z-lengthening, cross-shaped release and release of the gluteus maximus tendon insertion to the femur.<ref name=":0" /><ref name=":2" /> | The lengthening procedures include: Z-shaped release, formal Z-lengthening, cross-shaped release and release of the gluteus maximus tendon insertion to the femur.<ref name=":0" /><ref name=":2" /> | ||
Internal | '''Internal snapping hip:''' | ||
# Anterior approach to release the posteromedial tendinous portion of the iliopsoas | # Anterior approach to release the posteromedial tendinous portion of the iliopsoas | ||
| Line 150: | Line 153: | ||
== Trochanteric Bursitis == | == Trochanteric Bursitis == | ||
Lateral hip pain due to the inflammation of the bursa usually as a consequence of microtraumas produces a condition called trochanteric bursitis or greater trochanteric pain syndrome (GTPS).<ref>Seidman AJ, Varacallo M. [https://www.ncbi.nlm.nih.gov/books/NBK538503/ Trochanteric bursitis.] StatPearls [Internet]. 2020 Jun 29.</ref><ref name=":4">Crutchfield CR, Padaki AS, Holuba KS, Arney MM, O'Connor MJ, Menge TJ, Lynch TS. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8662929/pdf/IOJ-2021-045.pdf Open Versus Arthroscopic Surgical Management for Recalcitrant Trochanteric Bursitis: A Systematic Review]. Iowa Orthop J. 2021 Dec;41(2):45-57. </ref> It affects females between the age of 40 to 60 most commonly.<ref name=":5">Pandya R. Snapping Hip and Trochanteric Bursitis. Physiopedia Course, 2022.</ref>The abnormal hip biomechanics is the leading cause of development of the symptoms where the gluteus medius and minimus tendinopathy along with or without bursitis can lead to this painful lateral hip syndrome.<ref name=":5" /> | Lateral hip pain due to the inflammation of the bursa, usually as a consequence of microtraumas, produces a condition called [[Trochanteric Bursitis|trochanteric bursitis]] or [[Greater Trochanteric Pain Syndrome|greater trochanteric pain syndrome]] (GTPS).<ref>Seidman AJ, Varacallo M. [https://www.ncbi.nlm.nih.gov/books/NBK538503/ Trochanteric bursitis.] StatPearls [Internet]. 2020 Jun 29.</ref><ref name=":4">Crutchfield CR, Padaki AS, Holuba KS, Arney MM, O'Connor MJ, Menge TJ, Lynch TS. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8662929/pdf/IOJ-2021-045.pdf Open Versus Arthroscopic Surgical Management for Recalcitrant Trochanteric Bursitis: A Systematic Review]. Iowa Orthop J. 2021 Dec;41(2):45-57. </ref> It affects females between the age of 40 to 60 most commonly.<ref name=":5">Pandya R. Snapping Hip and Trochanteric Bursitis. Physiopedia Course, 2022.</ref> The abnormal hip [[biomechanics]] is the leading cause of development of the symptoms where the [[Gluteus Medius|gluteus medius]] and [[Gluteus Minimus|minimus]] tendinopathy along with or without [[bursitis]] can lead to this painful lateral hip syndrome.<ref name=":5" /> | ||
[[File:Trochanteric Bursitis.jpg|thumb|Trochanteric bursitis]] | [[File:Trochanteric Bursitis.jpg|thumb|Trochanteric bursitis]] | ||
==== Clinically Relevant Anatomy ==== | ==== Clinically Relevant Anatomy ==== | ||
A bursa or bursae (plural form) is a membrane sac lined by a synovial membrane or synovium | A bursa or bursae (plural form) is a membrane sac lined by a synovial membrane or [[Synovium & Synovial Fluid|synovium]] containing the [[Synovial Fluid Analysis|synovial fluid]].<ref name=":6" /> It is located between bone and surrounding soft tissue and near a joint.<ref name=":6">Mercadante JR, Marappa-Ganeshan R. [https://www.ncbi.nlm.nih.gov/books/NBK554438/ Anatomy, Skin Bursa.] [Updated 2021 Jul 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: <nowiki>https://www.ncbi.nlm.nih.gov/books/NBK554438/</nowiki></ref> Its role is to lubricate and reduce tension and friction between the soft tissue/bone interface. It also acts as a shock absorber during the movement of muscles and joints. Detailed information on the mechanism of injury or the pathological process of bursitis is available [[Bursitis|here]]. | ||
In the case of [[Trochanteric Bursitis]], two bursae are commonly involved: | In the case of [[Trochanteric Bursitis|trochanteric bursitis]], two bursae are commonly involved: | ||
# Subgluteus | # Subgluteus medius bursa - located above the greater trochanter and underneath the insertion of the gluteus medius. | ||
# Subgluteus | # Subgluteus maximus bursa - located between the greater trochanter and the insertion of the gluteus medius and gluteus maximus muscles. | ||
==== Pathophysiology ==== | ==== Pathophysiology ==== | ||
Altered lower extremity biomechanics and imbalances lead to the development of the GTPS. The aetiology of this syndrome is multifactorial<ref name=":4" /> and the following issues are believed to contribute to its presence: | Altered lower extremity biomechanics and imbalances lead to the development of the GTPS. The aetiology of this syndrome is multifactorial<ref name=":4" /> and the following issues are believed to contribute to its presence: | ||
* A lower femoral neck-shaft angle <ref name=":7">Schapira D, Nahir M, Scharf Y. Trochanteric bursitis: a common clinical problem. Arch Phys Med Rehabil. 1986 Nov;67(11):815-7.</ref><ref>Fearon A, Stephens S, Cook J, Smith P, Neeman T, Cormick W, Scarvell J. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3597182/pdf/bjsports-2011-090744.pdf The relationship of femoral neck-shaft angle and adiposity to greater trochanteric pain syndrome in women. A case-control morphology and anthropometric study]. Br J Sports Med. 2012 Sep;46(12):888-92. </ref> | * A lower femoral neck-shaft angle<ref name=":7">Schapira D, Nahir M, Scharf Y. Trochanteric bursitis: a common clinical problem. Arch Phys Med Rehabil. 1986 Nov;67(11):815-7.</ref><ref>Fearon A, Stephens S, Cook J, Smith P, Neeman T, Cormick W, Scarvell J. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3597182/pdf/bjsports-2011-090744.pdf The relationship of femoral neck-shaft angle and adiposity to greater trochanteric pain syndrome in women. A case-control morphology and anthropometric study]. Br J Sports Med. 2012 Sep;46(12):888-92. </ref> | ||
* Recently increased activities levels <ref name=":7" /><ref name=":8">Mellor R, Bennell K, Grimaldi A, Nicolson P, Kasza J, Hodges P, Wajswelner H, Vicenzino B. | * Recently increased activities levels<ref name=":7" /><ref name=":8">Mellor R, Bennell K, Grimaldi A, Nicolson P, Kasza J, Hodges P, Wajswelner H, Vicenzino B. [https://www.bmj.com/content/bmj/361/bmj.k1662.full.pdf Education plus exercise versus cortico- steroid injection use versus a wait and see approach on global outcome and pain from gluteal tendinopathy: prospective, single-blinded, randomised clinical trial]. BMJ, 2018;2(361):k1662. </ref> | ||
* Improper footwear<ref name=":7" /> | * Improper footwear<ref name=":7" /> | ||
* Hormonal changes after menopause <ref name=":7" /><ref>Ganderton C, Semciw A, Cook J, Pizzari T. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4910216/pdf/12905_2016_Article_311.pdf Does menopausal hormone therapy (MHT), exercise or a combination of both, improve pain and function in postmenopausal women with greater trochanteric pain syndrome (GTPS)? A randomised controlled trial]. BMC Women's Health. 2016 Jun 16;16:32. </ref> | * Hormonal changes after menopause<ref name=":7" /><ref>Ganderton C, Semciw A, Cook J, Pizzari T. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4910216/pdf/12905_2016_Article_311.pdf Does menopausal hormone therapy (MHT), exercise or a combination of both, improve pain and function in postmenopausal women with greater trochanteric pain syndrome (GTPS)? A randomised controlled trial]. BMC Women's Health. 2016 Jun 16;16:32. </ref> | ||
* Degeneration or tendinopathy in the gluteus medius and minimus musculature | * Degeneration or tendinopathy in the gluteus medius and minimus musculature<ref>Ho GW, Howard TM. Greater trochanteric pain syndrome: more than bursitis and iliotibial tract friction. Curr Sports Med Rep. 2012 Sep-Oct;11(5):232-8. </ref> | ||
* Repetitive microtrauma to the bursa caused by friction between the greater trochanter and iliotibial band<ref>Rothschild B. Trochanteric area pain, the result of a quartet of bursal inflammation. World J Orthop. 2013 Jul 18;4(3):100-2. </ref> | * Repetitive microtrauma to the bursa caused by friction between the greater trochanter and iliotibial band<ref>Rothschild B. Trochanteric area pain, the result of a quartet of bursal inflammation. World J Orthop. 2013 Jul 18;4(3):100-2. </ref> | ||
| Line 174: | Line 177: | ||
The following clinical presentation may occur: | The following clinical presentation may occur: | ||
* | * Pain at the lateral side of the hip radiating down<ref name=":5" /> | ||
* | * Difficulties with side-lying on the affected side<ref name=":5" /> | ||
* | * Pain while walking<ref name=":5" /> | ||
* | * Gait abnormalities <ref name=":5" /> | ||
* | * Tenderness over the greater trochanter<ref name=":8" /> | ||
* | * Pain interfering with sleep and physical function<ref name=":8" /> | ||
Differential | Differential diagnosis: | ||
* [[Iliotibial Band Syndrome]] | * [[Iliotibial Band Syndrome|Iliotibial band syndrome]] | ||
* [[Snapping Hip Syndrome]] | * [[Snapping Hip Syndrome|Snapping hip syndrome]] | ||
* Gluteus | * Gluteus medius tendon dysfunction and tears | ||
* [[Meralgia Paraesthetica|Meralgia | * [[Meralgia Paraesthetica|Meralgia paresthetica]] | ||
* Referred | * Referred rain | ||
* [[Osteoarthritis]] | * [[Osteoarthritis]] | ||
* [[Low Back Pain|Lower | * [[Low Back Pain|Lower back pain]] | ||
* [[Pelvic Floor and Other Pelvic Disorders|Pelvic | * [[Pelvic Floor and Other Pelvic Disorders|Pelvic pathology]] | ||
=== Evaluation === | === Evaluation === | ||
| Line 199: | Line 202: | ||
===== Patient's History ===== | ===== Patient's History ===== | ||
* symptoms | * Description of symptoms (pain) | ||
* | * Impact on activities of daily living | ||
===== Physical Examination ===== | ===== Physical Examination ===== | ||
* Observation | * Observation | ||
** Observe patient's posture in sitting and standing: watch for slightly flexed posture, slouch position, leaning to uninvolved side. <ref name=":9">Grumet RC, Frank RM, Slabaugh MA, Virkus WW, Bush-Joseph CA, Nho SJ. Lateral hip pain in an athletic population: differential diagnosis and treatment options. Sports Health. 2010 May;2(3):191-6.</ref> | ** Observe patient's posture in sitting and standing: watch for slightly flexed posture, slouch position, leaning to uninvolved side.<ref name=":9">Grumet RC, Frank RM, Slabaugh MA, Virkus WW, Bush-Joseph CA, Nho SJ. Lateral hip pain in an athletic population: differential diagnosis and treatment options. Sports Health. 2010 May;2(3):191-6.</ref> | ||
** Watch a patient walk: look at pelvic obliquity, the hip tendency to move into adduction while ambulating.<ref name=":5" /><ref name=":13" /> | ** Watch a patient walk: look at pelvic obliquity, the hip tendency to move into adduction while ambulating.<ref name=":5" /><ref name=":13" /> | ||
{{#ev:youtube|v=ZUPQp5oxXj8|300}}<ref name=":13">kenzothiazepine. Trendelenburg Gait. 2012. Available from: https://www.youtube.com/watch?v=ZUPQp5oxXj8 [last accessed 15/03/2022]</ref> | {{#ev:youtube|v=ZUPQp5oxXj8|300}}<ref name=":13">kenzothiazepine. Trendelenburg Gait. 2012. Available from: https://www.youtube.com/watch?v=ZUPQp5oxXj8 [last accessed 15/03/2022]</ref> | ||
* Palpation | * Palpation: | ||
** Palpate the iliotibial band and watch for tightness, irritation, pain, trigger points.<ref name=":5" /> | ** Palpate the iliotibial band and watch for tightness, irritation, pain, trigger points.<ref name=":5" /> | ||
** Check the lumbar spine, sacroiliac joints, ischium, iliac crest, lateral aspect of the greater trochanteric bursa, muscle bellies and the pubic symphysis to determine a potential source of hip symptoms or pain.<ref name=":9" /> | ** Check the lumbar spine, sacroiliac joints, ischium, iliac crest, lateral aspect of the greater trochanteric bursa, muscle bellies and the pubic symphysis to determine a potential source of hip symptoms or pain.<ref name=":9" /> | ||
* Range of motion assessment: | * Range of motion assessment: check active hip flexion, internal and external rotation, abduction and adduction. Movement can reproduce pain in the injured area. | ||
* Muscle strength assessment: assess major muscle groups acting on the hip joint. Hip abductor weakness is a common finding and testing the abductors can provoke lateral hip pain during the examination. | * Muscle strength assessment: assess major muscle groups acting on the hip joint. Hip abductor weakness is a common finding and testing the abductors can provoke lateral hip pain during the examination. | ||
* Functional assessment: mobility, gait. Look for any limb length discrepancy, weakness and heel strike which contributes to the function of the gluteus maximus.<ref>Woodley SJ, Nicholson HD, Livingstone V, Doyle TC, Meikle GR, Macintosh JE, Mercer SR. Lateral hip pain: findings from magnetic resonance imaging and clinical examination. journal of orthopaedic & sports physical therapy. 2008 Jun;38(6):313-28.</ref> | * Functional assessment: mobility, gait. Look for any limb length discrepancy, weakness and heel strike which contributes to the function of the gluteus maximus.<ref>Woodley SJ, Nicholson HD, Livingstone V, Doyle TC, Meikle GR, Macintosh JE, Mercer SR. Lateral hip pain: findings from magnetic resonance imaging and clinical examination. journal of orthopaedic & sports physical therapy. 2008 Jun;38(6):313-28.</ref> Inability to perform a putting on socks test, which requires the patient to sit with one leg crossed over in the figure 4 position, may indicate that changes are occurring in the hip joint. These changes can lead to osteoarthritis or trochanteric bursitis. | ||
===== Special Tests ===== | ===== Special Tests ===== | ||
* Jump | * Jump sign: patient in side-lying, so the affected side is on top, apply pressure around the lateral hip or the greater trochanteric region.<ref name=":5" /> This test a positive predictive value of about 83% for confirmation for the MRI.<ref name=":5" /> | ||
* Single leg stance test: patient to stand for 30 seconds on one leg. | * Single leg stance test: patient to stand for 30 seconds on one leg. The test is positive when the patient is not able to hold the balance. This test has almost a hundred per cent positive predictive value that confirms the MRI findings.<ref name=":5" /> | ||
* FADIR test | * FADIR test | ||
* [[FABER Test|FABER test]]<ref name=":14" /> | * [[FABER Test|FABER test]]<ref name=":14" /> | ||
* [[Ober's Test|Ober's test]] | * [[Ober's Test|Ober's test]] | ||
* Step | * Step down and step pp test<ref name=":15" /> | ||
* [[Trendelenburg Test|Trendelenburg test]] | * [[Trendelenburg Test|Trendelenburg test]] | ||
| Line 240: | Line 243: | ||
* Ultrasound: shows distension of the greater trochanteric bursa by anechoic or hypoechoic fluid<ref>Gaillard, F., El-Feky, M. [https://radiopaedia.org/articles/trochanteric-bursitis Trochanteric bursitis. Reference article], Radiopaedia.org. (accessed on 15 Mar 2022) <nowiki>https://doi.org/10.53347/rID-15141</nowiki></ref> | * Ultrasound: shows distension of the greater trochanteric bursa by anechoic or hypoechoic fluid<ref>Gaillard, F., El-Feky, M. [https://radiopaedia.org/articles/trochanteric-bursitis Trochanteric bursitis. Reference article], Radiopaedia.org. (accessed on 15 Mar 2022) <nowiki>https://doi.org/10.53347/rID-15141</nowiki></ref> | ||
* MRI: not necessary to diagnose trochanteric bursitis. It can assist with confirming or ruling out possible diagnoses.<ref>Woodley SJ, Nicholson HD, Livingstone V, Doyle TC, Meikle GR, Macintosh JE, Mercer SR. [https://www.jospt.org/doi/pdf/10.2519/jospt.2008.2685 Lateral hip pain: findings from magnetic resonance imaging and clinical examination]. J Orthop Sports Phys Ther. 2008 Jun;38(6):313-28.</ref> | * MRI: not necessary to diagnose trochanteric bursitis. It can assist with confirming or ruling out possible diagnoses.<ref>Woodley SJ, Nicholson HD, Livingstone V, Doyle TC, Meikle GR, Macintosh JE, Mercer SR. [https://www.jospt.org/doi/pdf/10.2519/jospt.2008.2685 Lateral hip pain: findings from magnetic resonance imaging and clinical examination]. J Orthop Sports Phys Ther. 2008 Jun;38(6):313-28.</ref> | ||
=== Management/Interventions === | === Management/Interventions === | ||
[[File:Gluteal tendinopathy va v12.png|thumb|350x350px|<small>''Adapted from: Mellor R, Bennell K, Grimaldi A, Nicolson P, Kasza J, Hodges P, Wajswelner H, Vicenzino B., 2018. Education plus exercise versus cortico- steroid injection use versus a wait and see approach on global outcome and pain from gluteal tendinopathy: a prospective, single-blinded, randomised clinical trial.''</small> |alt=|center]] | |||
==== Conservative Management ==== | ==== Conservative Management ==== | ||
Reports from the literature indicate that about 64% of patients find relief after one year of conservative therapy for trochanteric bursitis and 71% after five years. There is a high rate of recurrence of GTPS symptoms requiring repeated conservative therapy.<ref name=":16">Lustenberger DP, Ng VY, Best TM, Ellis TJ. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3689218/pdf/456671.pdf Efficacy of treatment of trochanteric bursitis: a systematic review.] Clin J Sport Med. 2011;21:447–453.</ref> | Reports from the literature indicate that about 64% of patients find relief after one year of conservative therapy for trochanteric bursitis and 71% after five years. There is a high rate of recurrence of GTPS symptoms requiring repeated conservative therapy.<ref name=":16">Lustenberger DP, Ng VY, Best TM, Ellis TJ. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3689218/pdf/456671.pdf Efficacy of treatment of trochanteric bursitis: a systematic review.] Clin J Sport Med. 2011;21:447–453.</ref> | ||
''Goal'': pain reduction, improvement in functional activities | ''Goal'': pain reduction, improvement in functional activities. | ||
Acute phase | Acute phase: | ||
* | * Activity modification: reduction in the intensity and frequency of running, avoid running on uneven surfaces or banked tracks<ref name=":4" /><ref name=":5" /> | ||
* | * Position modification: sleeping on the uninvolved side with a pillow in between the knees or by the side<ref name=":5" /> | ||
* | * Ice<ref name=":4" /><ref name=":5" /> | ||
* | * Oral NSAIDs (non-steroidal anti-inflammatory drugs), and corticosteroid and platelet-rich plasma (PRP) injections<ref name=":4" /><ref>Ali M, Oderuth E, Atchia I, Malviya A. [https://academic.oup.com/jhps/article/5/3/209/5087803?login=true The use of platelet-rich plasma in the treatment of greater trochanteric pain syndrome: a systematic literature review.] Journal of Hip Preservation Surgery. 2018 Aug;5(3):209-19.</ref> | ||
* | * Superficial release with soft tissue therapy<ref name=":5" /> | ||
* | * Taping<ref name=":5" /> | ||
* | * Shockwave therapy: may be used under special circumstances<ref name=":5" /><ref>Furia J, Rompe J, Maffulli N. Low-energy extracorporeal shock wave therapy as a treatment for greater trochanteric pain syndrome. Am J Sports Med. 2009; 37:1806–1813.</ref><ref>Rompe J, Segal N, Cacchio A, et al. Home training, local corticosteroid injection, or radial shock wave therapy for greater trochanteric pain syndrome. Am J Sports Med. 2009; 37:1981–1990.</ref> | ||
* | * Ultrasound therapy: not enough evidence<ref name=":5" /> | ||
[[File:3 quad hip abd hep2go.JPG|thumb|206x206px|Hip abductors strengthening exercises]] | [[File:3 quad hip abd hep2go.JPG|thumb|206x206px|Hip abductors strengthening exercises]] | ||
Subacute phase: | Subacute phase: | ||
* | * Strengthening of the abductors of the hip<ref name=":5" /> | ||
* [[File:Adductors stretch.jpg|thumb|Adductors stretch]] | * [[File:Adductors stretch.jpg|thumb|Adductors stretch]]Stretching of adductors<ref name=":5" /> | ||
* | * Activity modification: avoid hip adduction (legs crossing)<ref name=":5" /> | ||
* | * Exercise modification: avoid excessive ITB stretching exercises<ref name=":5" /> | ||
==== Surgical Intervention ==== | ==== Surgical Intervention ==== | ||
Cases with abductor tears or intra articular pathology confirmed by imaging do not respond well to conservative management and often require surgical intervention.<ref name=":4" /> | Cases with abductor tears or intra articular pathology confirmed by imaging do not respond well to conservative management and often require surgical intervention.<ref name=":4" /> | ||
''Goal'': | ''Goal'': pain reduction | ||
* Trochanteric bursectomy with or without iliotibial band release: good treatment option in grades 1 and 2 tendinopathy<ref name=":4" /><ref name=":17">Ladurner A, Fitzpatrick J, O’Donnell JM. [https://journals.sagepub.com/doi/full/10.1177/23259671211016850 Treatment of Gluteal Tendinopathy: A Systematic Review and Stage-Adjusted Treatment Recommendation]. Orthopaedic Journal of Sports Medicine. 2021 Jul 29;9(7).</ref> | * Trochanteric bursectomy with or without iliotibial band release: good treatment option in grades 1 and 2 tendinopathy<ref name=":4" /><ref name=":17">Ladurner A, Fitzpatrick J, O’Donnell JM. [https://journals.sagepub.com/doi/full/10.1177/23259671211016850 Treatment of Gluteal Tendinopathy: A Systematic Review and Stage-Adjusted Treatment Recommendation]. Orthopaedic Journal of Sports Medicine. 2021 Jul 29;9(7).</ref> | ||
| Line 291: | Line 293: | ||
[[Category:Hip - Interventions]] | [[Category:Hip - Interventions]] | ||
[[Category:Hip - Assessment and Examination]] | [[Category:Hip - Assessment and Examination]] | ||
[[Category:Plus Content]] | |||
Latest revision as of 18:26, 9 January 2024
Top Contributors - Ewa Jaraczewska, Jess Bell, Kim Jackson, Lucinda hampton and Tarina van der Stockt
Snapping Hip Syndrome (SHS)[edit | edit source]
Three types of snapping hip syndrome have been identified: external, internal, and intra-articular types, with the external type being the most common.[1]
External Snapping Hip Syndrome (ESHS)[edit | edit source]
External (lateral) snapping hip is a painful condition (also known as lateral coxa saltans), occurring in about 10% of the general population.[2]
- External extra-articular snapping is caused either by the posterior iliotibial band or the anterior aspect of the gluteus maximus as they move over the greater trochanter during hip flexion / extension or hip internal / external rotation.[3] This may lead to the inflammation of the trochanteric bursa.[3]
- Individuals with the ESHS may also have coxa vara, fibrotic scar tissue, a prominent greater trochanter, smaller lateral pelvic width, or have had surgery in the past for anterolateral knee instability.[4][5]
Internal Snapping Hip Syndrome (ISHS)[edit | edit source]
Internal extra-articular snapping is caused by the iliopsoas tendon snapping over the iliopectinal eminence or the femoral head and is more likely to occur while the hip flexors are contracting. Other proposed extra-articular mechanisms of this condition include:[3]
- Accessory iliopsoas tendon slips
- Iliopsoas snapping over a ridge at the lesser trochanter
- Snapping of the iliofemoral ligament over the femoral head
- Subluxation of the long head of the biceps at the ischium
- Snapping at the anterior inferior iliac spine.[3]
Intra-Articular Snapping Hip[edit | edit source]
Intra-articular factors can also lead to the development of snapping hip symptoms, including labral tears, ligamentum teres (ligament of the head of the femur) tears, loose bodies such as osteochondral fragments, or joint instability.
Clinically Relevant Anatomy[edit | edit source]
Iliotibial Band[edit | edit source]
The iliotibial band (ITB) is a thick band of fascia that runs on the lateral side of the thigh from the iliac crest and inserts at the knee.[6] It is composed of dense fibrous connective tissue that originates from the anterior fibres of the tensor fasciae late and the posterior fibres of the gluteus maximus. After running down on the lateral thigh most of its fibres insert onto the tibial tubercle, some insert into the gluteus maximum tendon, the lateral femoral epicondyle and distal lateral border of the patella.[2] During hip flexion, the ITB moves anterior to the greater trochanter and during hip extension it runs posterior to it.[3]
On the lateral aspect of the hip joint, there are three subgluteal bursae: greater trochanter bursa, subgluteus medius bursa, and subgluteus minimus bursa. The trochanteric bursa is the largest of the three and it covers the insertion of the gluteus medius tendon and the posterior aspect of the greater trochanter. Its primary role is to reduce friction between the tendons of the gluteus medius and the ITB when they pass over the greater trochanter.[7]
The iliotibial band is involved in hip stabilisation during single leg stance and ambulation when the band acts as a tendon of the tensor fasciae latae (TFL) and the gluteus maximus. The contraction of the gluteus maximus and the TFL muscles cause tightening of the band.
Gluteus Maximus[edit | edit source]
Gluteus maximus originates at the outer slope of the dorsal segment of the iliac crest, the gluteal surface of the ilium, dorsal surface of the lower part of the sacrum, side of the coccyx, and the sacrotuberous ligament. It also shares its attachment to the thoracolumbar fascia with the ipsilateral multifidus and contralateral latissimus dorsi. The muscle inserts onto the gluteal tuberosity and the iliotibial band.
Gluteus maximus is primarily involved in hip extension, external rotation and abduction. Its function is essential to maintain an erect posture.
Iliopsoas[edit | edit source]
The iliopsoas muscle complex is made up of three muscles: iliacus, psoas major and psoas minor.[3] It can work as a unit, but the three muscles all have separate functions. The iliopsoas originates at the fusion of the psoas major and iliacus muscles. This fusion occurs at the level of L5-S2, and the combined muscles pass from the pelvis to the thigh under the inguinal ligament. The iliopsoas muscle inserts into the lesser trochanter of the femur via the psoas tendon.
The iliopsoas bursa is the largest bursa of the hip joint and is located deep to the iliopsoas musculotendinous junction and anterior to the hip joint capsule. The bursa is believed to communicate with the hip joint in ~15% of patients. It helps the muscle glide and slide over the front of the hip during movement.[8]
The iliopsoas muscle is the strongest hip flexor and assists in external rotation of the femur. It is essential for correct standing and sitting lumbar posture, and during walking and running.
Pathophysiology[edit | edit source]
- External snapping hip
- Visual component to the snap observed by the patient when the ITB slides from the anterior to posterior aspect of the greater trochanter during hip movement from extension to flexion. This is usually caused by the thickening of the posterior ITB and/or the anterior portion of the gluteus maximus.[9]
- Internal snapping hip
- Audible component to the snap when the movement of the iliopsoas tendon from the lateral to the medial position is restricted during hip extension and internal rotation. This restriction can be caused by the femoral head or pectineal eminence of the pelvis.[9]
- Intra-articular snapping hip
- Pathological process of the hip joint when loose bodies, acetabular labral tears, or osteochondral fractures can interfere with the articulation of the femoral head into the acetabulum.[9]
- Pathological process of the hip joint when loose bodies, acetabular labral tears, or osteochondral fractures can interfere with the articulation of the femoral head into the acetabulum.[9]
Clinical Presentation[edit | edit source]
Individuals with external snapping hip syndrome typically describe a sensation that feels like hip dislocation. With internal snapping hip, patients describe a feeling of the hip joint being "stuck" or locked and they report hearing the sound of snapping. The intermittent sound of clicking or catching characterises intra-articular pathology.
Additionally patients may report:
- Pain
- Muscle weakness
- Activity limitations[4]
Evaluation[edit | edit source]
Physiotherapy Assessment[edit | edit source]
The physiotherapy assessment includes the patient's history, physical examination and special tests.
Patient's History[edit | edit source]
- Description of symptoms (location, sensation, timing and duration)
- Impact on activities of daily living
Physical Examination[edit | edit source]
- Joint palpation: snapping palpated over the anterior hip indicates coxa saltans interna
- Range of motion assessment
- Strength assessment
- Pain assessment (Visual Analogue Scale)
- Functional assessment including gait assessment.
Special Tests[edit | edit source]
External snapping hip syndrome:
- FADIR test including flexion, adduction and internal rotation or impingement
- Ober's test: assessment of the ITB tightness[10]
- Hip active flexion followed by passive extension and abduction: positive test reproduces the snapping over the greater trochanter.
- Hula hoop test is an alternative test when the hip is adducted and circumducted in a standing position. Positive test: snapping is reproduced over the greater trochanter
- Biomechanical abnormalities (Trendelenburg sign)
Internal snapping hip syndrome:
- Dynamic testing (loop-the-loop): starting at FABER (flexion, abduction and external rotation) position and moving into EADIR (extension, adduction and internal rotation) position. Positive test: snapping of the iliopsoas tendon[11]
- Thomas test: positive test indicates psoas contracture[12]
- Stinchfield Test: The patient lies supine with the hip flexed at 30°. The patient is asked to fully flex the hip, while the examiner applies a resistance force. Pain in the anterior groin indicates a positive test.
Imaging[edit | edit source]
- X-Ray: no typical findings indicative of coxa saltans interna on x-ray. Evidence of femoroacetabular impingement can be found on a plain X-ray.[3]
- MRI: not specific for iliopsoas involvement. May assist with the diagnosis of iliopsoas bursa or iliopsoas muscle inflammation. This modality helps to visualise a thickened ITB and focal thickening of the gluteus maximus when ESHS is suspected.[3]
- Ultrasound: helps to visualise the dynamic motion of the iliopsoas tendon, but requires a skilled clinician to perform and interpret results.[3][13]
- Dynamic sonography: able to detect the movement of the ITB over the greater trochanter.
- Iliopsoas bursography: under fluoroscopy, bursa is filled with contrast to visualise the tendon moving back and forth. This imaging is performed to confirm ISHS syndrome.[3]
Management / Interventions[edit | edit source]
Conservative Management[edit | edit source]
Goal: to improve pain, increase flexibility and equalise the limb length discrepancy if needed.
A conservative approach should be continued for at least 6 months and the following strategies are recommended:[2]
- Rest, icing and anti-inflammatories should be advocated to reduce inflammation[3]
- Muscle tightness causing the snapping must be identified: passive and active stretching programme specific to the ITB and the iliopsoas muscles to be initiated [3]
- Single leg stance exercises (ESHS)[14]
- Lateral walking with theraband (ESHS)[14]
- Hip hiking exercises (ESHS)[14]
- Movements that provoke the snap should be avoided
- Sports activities must be reduced
- Active release techniques[14]
- Use of modalities: laser therapy or extracorporeal shockwave therapy ESWT[15]
Surgical Intervention[edit | edit source]
Goal: to release the contracted ITB or the iliopsoas to resolve the snap[16]
External snapping hip:
- Fractional lengthening of the tendon
- Complete release of the tendinous portion[17]
The lengthening procedures include: Z-shaped release, formal Z-lengthening, cross-shaped release and release of the gluteus maximus tendon insertion to the femur.[3][2]
Internal snapping hip:
- Anterior approach to release the posteromedial tendinous portion of the iliopsoas
- Endoscopic release of the iliopsoas tendon[3][18]
Trochanteric Bursitis[edit | edit source]
Lateral hip pain due to the inflammation of the bursa, usually as a consequence of microtraumas, produces a condition called trochanteric bursitis or greater trochanteric pain syndrome (GTPS).[19][20] It affects females between the age of 40 to 60 most commonly.[21] The abnormal hip biomechanics is the leading cause of development of the symptoms where the gluteus medius and minimus tendinopathy along with or without bursitis can lead to this painful lateral hip syndrome.[21]
Clinically Relevant Anatomy[edit | edit source]
A bursa or bursae (plural form) is a membrane sac lined by a synovial membrane or synovium containing the synovial fluid.[22] It is located between bone and surrounding soft tissue and near a joint.[22] Its role is to lubricate and reduce tension and friction between the soft tissue/bone interface. It also acts as a shock absorber during the movement of muscles and joints. Detailed information on the mechanism of injury or the pathological process of bursitis is available here.
In the case of trochanteric bursitis, two bursae are commonly involved:
- Subgluteus medius bursa - located above the greater trochanter and underneath the insertion of the gluteus medius.
- Subgluteus maximus bursa - located between the greater trochanter and the insertion of the gluteus medius and gluteus maximus muscles.
Pathophysiology[edit | edit source]
Altered lower extremity biomechanics and imbalances lead to the development of the GTPS. The aetiology of this syndrome is multifactorial[20] and the following issues are believed to contribute to its presence:
- A lower femoral neck-shaft angle[23][24]
- Recently increased activities levels[23][25]
- Improper footwear[23]
- Hormonal changes after menopause[23][26]
- Degeneration or tendinopathy in the gluteus medius and minimus musculature[27]
- Repetitive microtrauma to the bursa caused by friction between the greater trochanter and iliotibial band[28]
Clinical Presentation[edit | edit source]
The following clinical presentation may occur:
- Pain at the lateral side of the hip radiating down[21]
- Difficulties with side-lying on the affected side[21]
- Pain while walking[21]
- Gait abnormalities [21]
- Tenderness over the greater trochanter[25]
- Pain interfering with sleep and physical function[25]
Differential diagnosis:
- Iliotibial band syndrome
- Snapping hip syndrome
- Gluteus medius tendon dysfunction and tears
- Meralgia paresthetica
- Referred rain
- Osteoarthritis
- Lower back pain
- Pelvic pathology
Evaluation[edit | edit source]
Physiotherapy Assessment[edit | edit source]
Physiotherapy assessment includes the patient's history, physical examination and special tests.
Patient's History[edit | edit source]
- Description of symptoms (pain)
- Impact on activities of daily living
Physical Examination[edit | edit source]
- Observation
- Palpation:
- Palpate the iliotibial band and watch for tightness, irritation, pain, trigger points.[21]
- Check the lumbar spine, sacroiliac joints, ischium, iliac crest, lateral aspect of the greater trochanteric bursa, muscle bellies and the pubic symphysis to determine a potential source of hip symptoms or pain.[29]
- Range of motion assessment: check active hip flexion, internal and external rotation, abduction and adduction. Movement can reproduce pain in the injured area.
- Muscle strength assessment: assess major muscle groups acting on the hip joint. Hip abductor weakness is a common finding and testing the abductors can provoke lateral hip pain during the examination.
- Functional assessment: mobility, gait. Look for any limb length discrepancy, weakness and heel strike which contributes to the function of the gluteus maximus.[31] Inability to perform a putting on socks test, which requires the patient to sit with one leg crossed over in the figure 4 position, may indicate that changes are occurring in the hip joint. These changes can lead to osteoarthritis or trochanteric bursitis.
Special Tests[edit | edit source]
- Jump sign: patient in side-lying, so the affected side is on top, apply pressure around the lateral hip or the greater trochanteric region.[21] This test a positive predictive value of about 83% for confirmation for the MRI.[21]
- Single leg stance test: patient to stand for 30 seconds on one leg. The test is positive when the patient is not able to hold the balance. This test has almost a hundred per cent positive predictive value that confirms the MRI findings.[21]
- FADIR test
- FABER test[32]
- Ober's test
- Step down and step pp test[33]
- Trendelenburg test
Imaging[edit | edit source]
- Ultrasound: shows distension of the greater trochanteric bursa by anechoic or hypoechoic fluid[34]
- MRI: not necessary to diagnose trochanteric bursitis. It can assist with confirming or ruling out possible diagnoses.[35]
Management/Interventions[edit | edit source]

Conservative Management[edit | edit source]
Reports from the literature indicate that about 64% of patients find relief after one year of conservative therapy for trochanteric bursitis and 71% after five years. There is a high rate of recurrence of GTPS symptoms requiring repeated conservative therapy.[36]
Goal: pain reduction, improvement in functional activities.
Acute phase:
- Activity modification: reduction in the intensity and frequency of running, avoid running on uneven surfaces or banked tracks[20][21]
- Position modification: sleeping on the uninvolved side with a pillow in between the knees or by the side[21]
- Ice[20][21]
- Oral NSAIDs (non-steroidal anti-inflammatory drugs), and corticosteroid and platelet-rich plasma (PRP) injections[20][37]
- Superficial release with soft tissue therapy[21]
- Taping[21]
- Shockwave therapy: may be used under special circumstances[21][38][39]
- Ultrasound therapy: not enough evidence[21]
Subacute phase:
- Strengthening of the abductors of the hip[21]
- Stretching of adductors[21]
- Activity modification: avoid hip adduction (legs crossing)[21]
- Exercise modification: avoid excessive ITB stretching exercises[21]
Surgical Intervention[edit | edit source]
Cases with abductor tears or intra articular pathology confirmed by imaging do not respond well to conservative management and often require surgical intervention.[20]
Goal: pain reduction
- Trochanteric bursectomy with or without iliotibial band release: good treatment option in grades 1 and 2 tendinopathy[20][40]
- Lengthening or release of the ITB and fascia late (Z-plasty)[36]
- Trochanteric reduction osteotomy[36]
- Surgical repair for grades 3 (partial-thickness tears) and 4 (full-thickness tears) tendinopathy: low-level evidence[40]
Resources[edit | edit source]
Walker P, Ellis E, Scofield J, Kongchum T, Sherman WF, Kaye AD. Snapping Hip Syndrome: A Comprehensive Update. Orthopaedic Reviews. 2021;13(2).
Olufade O, Yoo A, Negron G, McDermott H, Jayanthi N. Greater Trochanteric Pain Syndrome (GTPS): A clinical prospective study of treatment options. J Orthop Pract. 2021;1(1).
Pianka MA, Serino J, DeFroda SF, Bodendorfer BM. Greater trochanteric pain syndrome: Evaluation and management of a wide spectrum of pathology. SAGE open medicine. 2021 Jun;9:20503121211022582.
References[edit | edit source]
- ↑ Radiopedia Snapping hip syndrome Available:https://radiopaedia.org/articles/snapping-hip-syndrome?lang=us (accessed 30/10.2022)
- ↑ 2.0 2.1 2.2 2.3 Randelli F, Mazzoleni MG, Fioruzzi A, Giai Via A, Calvisi V, Ayeni OR. Surgical interventions for external snapping hip syndrome. Knee Surg Sports Traumatol Arthrosc. 2021 Aug;29(8):2386-2393.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 Yen YM, Lewis CL, Kim YJ. Understanding and Treating the Snapping Hip. Sports Med Arthrosc Rev. 2015 Dec;23(4):194-9.
- ↑ 4.0 4.1 Idjadi J, Meislin R. Symptomatic snapping hip: targeted treatment for maximum pain relief. The Physician and Sportsmedicine 2004;32(1):25-31.
- ↑ Byrd JT. Snapping hip. Operative Techniques in Sports Medicine 2005;13(1):46-54.
- ↑ Baker RL, Fredericson M. Iliotibial Band Syndrome in Runners: Biomechanical Implications and Exercise Interventions. Physical médicine and réhabilitation clinics of North America, 2016; 27(1):53-77
- ↑ Weerakkody, Y., Bell, D. Hip bursae. Reference article, Radiopaedia.org. (accessed on 13 Mar 2022) https://doi.org/10.53347/rID-64260
- ↑ Bordoni B, Varacallo M. Anatomy, Bony Pelvis and Lower Limb, Iliopsoas Muscle. [Updated 2021 Jul 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK531508/
- ↑ 9.0 9.1 9.2 Walker P, Ellis E, Scofield J, Kongchum T, Sherman WF, Kaye AD. Snapping Hip Syndrome: A Comprehensive Update. Orthopaedic Reviews. 2021;13(2).
- ↑ 10.0 10.1 Sports Injuries And Rehabilitation. Ober`s Test - Hip Special Test. 2017.Available from: https://www.youtube.com/watch?v=6FEvmhjMVNs[last accessed 13/03/2022]
- ↑ 11.0 11.1 The Physio Channel. How to test for a Snapping Clicking Hip. 2018.Available from: https://www.youtube.com/watch?v=xkEq7nGUA1o [last accessed 13/03/2022]
- ↑ 12.0 12.1 John Gibbons. THE PSOAS Muscle - Simple test for tight HIP FLEXORS (Modified Thomas test). 2018. Available from: https://www.youtube.com/watch?v=qsgrMVuataI [last accessed 13/03/2022]
- ↑ Winston P, Awan R, Cassicy JD et al. Clinical examination and ultrasound of self-reported snapping hip syndrome in elite ballet dancers. Am J Sports Med. 2007;35:118-126.
- ↑ 14.0 14.1 14.2 14.3 Spina AA. External coxa saltans (snapping hip) treated with Active Release Techniques: a case report. J Can Chiropr Assoc. 2007 Mar;51(1):23-9.
- ↑ Frizziero A, Vittadini F, Pignataro A, Gasparre G, Biz C, Ruggieri P, Masiero S. Conservative management of tendinopathies around hip. Muscles Ligaments Tendons J. 2016 Dec 21;6(3):281-292.
- ↑ Pierce TP, Kurowicki J, Issa K, Festa A, Scillia AJ, McInerney VK. External snapping hip: a systematic review of outcomes following surgical intervention: External snapping hip systematic review. Hip Int. 2018 Sep;28(5):468-472.
- ↑ Malinowski K, Kalinowski Ł, Góralczyk A, Ribas M, Lund B, Hermanowicz K. External Snapping Hip Syndrome Endoscopic Treatment: “Fan-like” Technique as a Stepwise, Tailor-made Solution.Arthroscopy Techniques, 2020; 9(10): e1553-e1557.
- ↑ Maldonado DR, Lall AC, Battaglia MR, Laseter JR, Chen JW, Domb BG. Arthroscopic Iliopsoas Fractional Lengthening. JBJS Essent Surg Tech. 2018 Nov 28;8(4):e30.
- ↑ Seidman AJ, Varacallo M. Trochanteric bursitis. StatPearls [Internet]. 2020 Jun 29.
- ↑ 20.0 20.1 20.2 20.3 20.4 20.5 20.6 Crutchfield CR, Padaki AS, Holuba KS, Arney MM, O'Connor MJ, Menge TJ, Lynch TS. Open Versus Arthroscopic Surgical Management for Recalcitrant Trochanteric Bursitis: A Systematic Review. Iowa Orthop J. 2021 Dec;41(2):45-57.
- ↑ 21.00 21.01 21.02 21.03 21.04 21.05 21.06 21.07 21.08 21.09 21.10 21.11 21.12 21.13 21.14 21.15 21.16 21.17 21.18 21.19 21.20 21.21 Pandya R. Snapping Hip and Trochanteric Bursitis. Physiopedia Course, 2022.
- ↑ 22.0 22.1 Mercadante JR, Marappa-Ganeshan R. Anatomy, Skin Bursa. [Updated 2021 Jul 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554438/
- ↑ 23.0 23.1 23.2 23.3 Schapira D, Nahir M, Scharf Y. Trochanteric bursitis: a common clinical problem. Arch Phys Med Rehabil. 1986 Nov;67(11):815-7.
- ↑ Fearon A, Stephens S, Cook J, Smith P, Neeman T, Cormick W, Scarvell J. The relationship of femoral neck-shaft angle and adiposity to greater trochanteric pain syndrome in women. A case-control morphology and anthropometric study. Br J Sports Med. 2012 Sep;46(12):888-92.
- ↑ 25.0 25.1 25.2 Mellor R, Bennell K, Grimaldi A, Nicolson P, Kasza J, Hodges P, Wajswelner H, Vicenzino B. Education plus exercise versus cortico- steroid injection use versus a wait and see approach on global outcome and pain from gluteal tendinopathy: prospective, single-blinded, randomised clinical trial. BMJ, 2018;2(361):k1662.
- ↑ Ganderton C, Semciw A, Cook J, Pizzari T. Does menopausal hormone therapy (MHT), exercise or a combination of both, improve pain and function in postmenopausal women with greater trochanteric pain syndrome (GTPS)? A randomised controlled trial. BMC Women's Health. 2016 Jun 16;16:32.
- ↑ Ho GW, Howard TM. Greater trochanteric pain syndrome: more than bursitis and iliotibial tract friction. Curr Sports Med Rep. 2012 Sep-Oct;11(5):232-8.
- ↑ Rothschild B. Trochanteric area pain, the result of a quartet of bursal inflammation. World J Orthop. 2013 Jul 18;4(3):100-2.
- ↑ 29.0 29.1 Grumet RC, Frank RM, Slabaugh MA, Virkus WW, Bush-Joseph CA, Nho SJ. Lateral hip pain in an athletic population: differential diagnosis and treatment options. Sports Health. 2010 May;2(3):191-6.
- ↑ 30.0 30.1 kenzothiazepine. Trendelenburg Gait. 2012. Available from: https://www.youtube.com/watch?v=ZUPQp5oxXj8 [last accessed 15/03/2022]
- ↑ Woodley SJ, Nicholson HD, Livingstone V, Doyle TC, Meikle GR, Macintosh JE, Mercer SR. Lateral hip pain: findings from magnetic resonance imaging and clinical examination. journal of orthopaedic & sports physical therapy. 2008 Jun;38(6):313-28.
- ↑ 32.0 32.1 Clinical Physio. Fabers Test Hip and SIJ | Clinical Physio Premium. 2019.Available from: https://www.youtube.com/watch?v=X6trjwpyjdM [last accessed 15/03/2022]
- ↑ 33.0 33.1 AIF Education. Functional Movement Test - Step Up and Down. 2013.Available from: https://www.youtube.com/watch?v=uUUDSxcO5VY[last accessed 15/03/2022]
- ↑ Gaillard, F., El-Feky, M. Trochanteric bursitis. Reference article, Radiopaedia.org. (accessed on 15 Mar 2022) https://doi.org/10.53347/rID-15141
- ↑ Woodley SJ, Nicholson HD, Livingstone V, Doyle TC, Meikle GR, Macintosh JE, Mercer SR. Lateral hip pain: findings from magnetic resonance imaging and clinical examination. J Orthop Sports Phys Ther. 2008 Jun;38(6):313-28.
- ↑ 36.0 36.1 36.2 Lustenberger DP, Ng VY, Best TM, Ellis TJ. Efficacy of treatment of trochanteric bursitis: a systematic review. Clin J Sport Med. 2011;21:447–453.
- ↑ Ali M, Oderuth E, Atchia I, Malviya A. The use of platelet-rich plasma in the treatment of greater trochanteric pain syndrome: a systematic literature review. Journal of Hip Preservation Surgery. 2018 Aug;5(3):209-19.
- ↑ Furia J, Rompe J, Maffulli N. Low-energy extracorporeal shock wave therapy as a treatment for greater trochanteric pain syndrome. Am J Sports Med. 2009; 37:1806–1813.
- ↑ Rompe J, Segal N, Cacchio A, et al. Home training, local corticosteroid injection, or radial shock wave therapy for greater trochanteric pain syndrome. Am J Sports Med. 2009; 37:1981–1990.
- ↑ 40.0 40.1 Ladurner A, Fitzpatrick J, O’Donnell JM. Treatment of Gluteal Tendinopathy: A Systematic Review and Stage-Adjusted Treatment Recommendation. Orthopaedic Journal of Sports Medicine. 2021 Jul 29;9(7).