Sleep Apnea: Difference between revisions
No edit summary |
No edit summary |
||
| Line 45: | Line 45: | ||
* Prevalence also increases with age, and when individuals reach 50 years of age or more, there are as many women as men who develop the disorder.<span style="line-height: 1.5em;"> </span> | * Prevalence also increases with age, and when individuals reach 50 years of age or more, there are as many women as men who develop the disorder.<span style="line-height: 1.5em;"> </span> | ||
* <span style="line-height: 1.5em;">Genetics and abnormalities or conditions of the craniofacial morphology also increase the likelihood of OSA. Individuals with a first-degree relative with OSA were at a 1.5-2x increased risk of developing OSA</span><ref name=":0" /><span style="line-height: 1.5em;">.</span><ref name="prevalence2">Lam J, Sharma S, Lam B. Obstructive sleep apnea: Definitions, epidemiology & natural history. Indian J Med Res 2010;131:165-170. http://pharexmedics.com/wp-content/uploads/2015/11/sleepapnea_ebook.pdf (accessed 3 April 2016).</ref> | * <span style="line-height: 1.5em;">Genetics and abnormalities or conditions of the craniofacial morphology also increase the likelihood of OSA. Individuals with a first-degree relative with OSA were at a 1.5-2x increased risk of developing OSA</span><ref name=":0" /><span style="line-height: 1.5em;">.</span><ref name="prevalence2">Lam J, Sharma S, Lam B. Obstructive sleep apnea: Definitions, epidemiology & natural history. Indian J Med Res 2010;131:165-170. http://pharexmedics.com/wp-content/uploads/2015/11/sleepapnea_ebook.pdf (accessed 3 April 2016).</ref> | ||
* <span style="line-height: 1.5em;">OSA is common in individuals who spend long periods of time sitting and driving, such as commercial truck drivers.</span><ref name="Management" /> | * <span style="line-height: 1.5em;">OSA is common in individuals who spend long periods of time sitting and driving, such as commercial truck drivers.</span><ref name="Management">Epstein L, Kristo D, Strollo Jr. P, Friedman N, Malhotra A, Patil S, et al. Clinical Guideline for the Evaluation, Management and Long-term Care of Obstructive Sleep Apnea in Adults. Journal of Clinical Sleep Medication 2009; 5(3): 263-276. http://pharexmedics.com/wp-content/uploads/2015/11/sleepapnea_ebook.pdf (accessed 3 April 2016).</ref> | ||
<sup></sup> | <sup></sup> | ||
| Line 66: | Line 66: | ||
== Treatment == | == Treatment == | ||
For adults, the use of continuous positive airway pressure (CPAP) is the most effective treatment | [[Image:CPAP.png|right|250x200px|https://en.wikipedia.org/wiki/Positive_airway_pressure]]For adults, the use of continuous positive airway pressure (CPAP) is the most effective treatment | ||
* Adherence to nightly CPAP use can result in near complete resolution of symptoms. | * Adherence to nightly CPAP use can result in near complete resolution of symptoms. | ||
* For patients unable or unwilling to use CPAP or those who will be unable to access electricity reliably, custom fitted and titrated oral appliances can be used to bring the lower jaw forward and relieve airway obstruction. | * For patients unable or unwilling to use CPAP or those who will be unable to access electricity reliably, custom fitted and titrated oral appliances can be used to bring the lower jaw forward and relieve airway obstruction. | ||
| Line 78: | Line 78: | ||
== Evaluation == | == Evaluation == | ||
# Nighttime in-laboratory Level 1 polysomnography (PSG) is the standard gold test for diagnosis of obstructive sleep apnea. During the test, patients are monitored with EEG leads, pulse oximetry, temperature and pressure sensors to detect nasal and oral airflow, respiratory impedance plethysmography or similar resistance belts around the chest and abdomen to detect motion, an ECG lead, and EMG sensors to detect muscle contraction in the chin, chest, and legs. A hypopnea can be based on one of two criteria. It can either be a reduction in airflow of at least 30% for more than 10 seconds associated with at least 4% oxygen desaturation or a reduction in airflow of at least 30% for more than 10 [[Image:Pediatric polysomnogram.jpg|right|200x160px|https://en.wikipedia.org/wiki/Polysomnography|frameless]]seconds associated with at least 3% oxygen desaturation or an arousal from sleep on EEG.<ref name=":0" /> | # Nighttime in-laboratory Level 1 polysomnography (PSG) is the standard gold test for diagnosis of obstructive sleep apnea. During the test, patients are monitored with EEG leads, pulse oximetry, temperature and pressure sensors to detect nasal and oral airflow, respiratory impedance plethysmography or similar resistance belts around the chest and abdomen to detect motion, an ECG lead, and EMG sensors to detect muscle contraction in the chin, chest, and legs. A hypopnea can be based on one of two criteria. It can either be a reduction in airflow of at least 30% for more than 10 seconds associated with at least 4% oxygen desaturation or a reduction in airflow of at least 30% for more than 10 [[Image:Pediatric polysomnogram.jpg|right|200x160px|https://en.wikipedia.org/wiki/Polysomnography|frameless]]seconds associated with at least 3% oxygen desaturation or an arousal from sleep on EEG.<ref name=":0" /> | ||
Image R; Polysomnography testing child. | Image R; Polysomnography testing child. | ||
| Line 91: | Line 90: | ||
*Oximetry: analyze oxygen saturation of hemoglobin to help identify individuals unlikely to have OSA.<ref name="diagnose3" /><br> | *Oximetry: analyze oxygen saturation of hemoglobin to help identify individuals unlikely to have OSA.<ref name="diagnose3" /><br> | ||
== | == Morbidities associated with OSA == | ||
* OSA induced biological changes include intermittent hypoxia, intermittent hypercapnia, intrathoracic pressure changes, sympathetic activation and sleep fragmentation. | |||
* OSA can cause metabolic dysregulation, endothelial dysfunction, systemic inflammation, oxidative stress and hypercoagulation, and neurohumoral changes. | |||
* There is evidence suggesting that OSA is independently associated with metabolic syndrome. | |||
* OSA has been shown to increase the risk for systemic hypertension, [[Pulmonary Hypertension|pulmonary vascular disease]], [[Coronary Artery Disease (CAD)|ischemic heart disease]], cerebral vascular disease, [[Heart Failure|congestive heart failure]] and [[Heart Arrhythmias: Assessment|arrhythmias]]<ref>Vijayan VK. [https://www.medscape.com/viewarticle/775550 Morbidities associated with obstructive sleep apnea.] Expert review of respiratory medicine. 2012 Oct 1;6(5):557-66.Available from:https://www.medscape.com/viewarticle/775550 (last accessed 6.10.2020)</ref><sup></sup><sup></sup><sup></sup><sup></sup> | |||
* | |||
* | |||
[ | |||
<sup></sup><sup></sup><sup></sup | |||
== Physical Therapy Management == | == Physical Therapy Management == | ||
| Line 197: | Line 135: | ||
*Nocturnal Frontal Lobe Epilepsy<ref name="epilepsy">Cho J, Kim D, Noh K, Kim S, Lee J, Kim J. Nocturnal frontal lobe epilepsy presenting as obstructive type sleep apnea. J Epilepsy Res 2011; 1(2): 74-76. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3952334/ (accessed 8 April 2016)</ref> | *Nocturnal Frontal Lobe Epilepsy<ref name="epilepsy">Cho J, Kim D, Noh K, Kim S, Lee J, Kim J. Nocturnal frontal lobe epilepsy presenting as obstructive type sleep apnea. J Epilepsy Res 2011; 1(2): 74-76. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3952334/ (accessed 8 April 2016)</ref> | ||
*REM Behaviour Disorder<ref name="pharm" /> | *REM Behaviour Disorder<ref name="pharm">Booth A, Djavadkhani Y, Marshall N. A critical review of the treatment options available for obstructive sleep apnoea: an overview of the current literature available on treatment methods for obstructive sleep apnoea and future research directions. Bioscience Horizons 2014;7(0):1-8. http://biohorizons.oxfordjournals.org/content/7/hzu011.full.pdf (accessed 4 April 2016).</ref> | ||
*Periodic Limb Movement Disorder<ref name="pharm" /> <ref name="diagnose5">Downey III R, Rowley J, Wickramasinghe H, Gold P. Obstructive Sleep Apnea Differential Diagnoses. Emedicinemedscapecom. 2016. Available at: http://emedicine.medscape.com/article/295807-differential. Accessed April 9, 2016.</ref> | *Periodic Limb Movement Disorder<ref name="pharm" /> <ref name="diagnose5">Downey III R, Rowley J, Wickramasinghe H, Gold P. Obstructive Sleep Apnea Differential Diagnoses. Emedicinemedscapecom. 2016. Available at: http://emedicine.medscape.com/article/295807-differential. Accessed April 9, 2016.</ref> | ||
*Central Sleep Apnea<ref name="pharm" /> <ref name="diagnose5" /> | *Central Sleep Apnea<ref name="pharm" /> <ref name="diagnose5" /> | ||
Revision as of 07:25, 6 October 2020
Original Editors - Ylice Bridges and Irena Tran
Top Contributors - Irena Tran, Ylice Bridges, Lucinda hampton, Venugopal Pawar, Kim Jackson, 127.0.0.1, Elaine Lonnemann, Admin, WikiSysop, Adam Vallely Farrell and Lilian Ashraf
Definition/Description[edit | edit source]
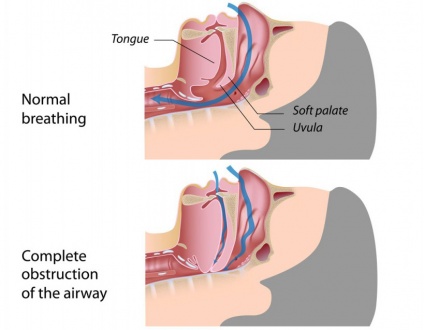
Sleep apnea is a disorder in which breathing is interrupted or paused during sleep. The pauses in breathing can last a few seconds to minutes and are long enough to:
- Disrupt sleep
- Decrease level of oxygen in the blood
- Increase level of carbon dioxide in the blood
These breathing interruptions can occur more than 30 times an hour and significantly impair the quality of sleep. Because of this, sleep apnea is a leading cause of excessive daytime sleepiness.[1]
There are three types of sleep apnea: central, obstructive and mixed. Obstructive sleep apnea is the most common and the main focus of this article.
- Obstructive sleep apnea (OSA) is caused by repeated partial or complete obstruction of the upper airway that diminishes or stops breathing.
- Central sleep apnea occurs when the brain is less sensitive to changes in carbon dioxide levels in the blood and fails to send signals to the respiratory muscles to breathe deeper.
- Mixed sleep apnea is a combination of both obstructive and central sleep apnea episodes.[1]
Etiology[edit | edit source]
Sleep apnea occurs when there is not enough space to accommodate sufficient airflow in a portion of the upper airway during sleep.
- When muscle tone is decreased, the result is a repetitive total or partial collapse of the airway.
- In children, the most common cause of obstructive sleep apnea is enlarged tonsils and/or adenoids.
- In adults, it is most commonly associated with obesity, male sex, and advancing age.[2]
Factors that contribute to airway obstruction are:[3]
- Obesity
- Large neck circumference
- Large tongue or tonsils
- Narrow airway due to bony structures of head and neck
- Taking sedative medication
- Drinking alcohol
- Smoking
- Nasal congestion
Medical disorders associated with OSA include:
- Stroke
- Hypothyroidism
- Metabolic syndrome
- Acromegaly
- Neurological disorders (eg myasthenia gravis)[2]
Epidemiology[edit | edit source]
- In the United States, it has been reported that 4% of men and 2% of women meet criteria for obstructive sleep apnea.
- More recently, prevalence has been reported to be as high as 14% of men and 5% of women in the United States.
- Prevalence is higher in Hispanic, African American, and Asian populations[2].
- Prevalence also increases with age, and when individuals reach 50 years of age or more, there are as many women as men who develop the disorder.
- Genetics and abnormalities or conditions of the craniofacial morphology also increase the likelihood of OSA. Individuals with a first-degree relative with OSA were at a 1.5-2x increased risk of developing OSA[2].[4]
- OSA is common in individuals who spend long periods of time sitting and driving, such as commercial truck drivers.[5]
Characteristics/Clinical Presentation[edit | edit source]
- Typical adult obstructive sleep apnea patient
- Overweight or obese middle-aged male or postmenopausal female with excessive daytime sleepiness and loud nightly snoring.
- May also complain of waking to gasp for breath or choking, sleep maintenance insomnia, night sweats, nighttime reflux, and nocturia in the absence of excessive nighttime liquid intake.
- Typically larger than average neck circumference (17 inches in males) with crowded oropharynx and large tongue.
- Retrognathism (an abnormal posterior positioning of the maxilla or mandible relative to the facial skeleton and soft tissues) may be present.
Patients with refractory atrial fibrillation, resistant hypertension, and history of a stroke should be screened for sleep apnea regardless of symptoms[2].
2. Typical child with obstructive sleep apnea
- Loud nightly snoring
- May be hyperactive rather than sleepy
- May have academic difficulties.
- These children can be incorrectly diagnosed with attention deficit hyperactivity disorder (ADHD).
- Night sweats, nighttime reflux, sleep maintenance insomnia, restless sleep with frequent limb movements, and secondary nocturnal enuresis may also be present.
- A physical exam is often notable for adenoidal facies ( long, open-mouthed face of children with adenoid hypertrophy[6]), tonsillar hypertrophy, hyponasal speech, and high arched palate.
Patients with Down syndrome and any other condition associated with hypotonia should be screened for obstructive sleep apnea regardless of symptoms.[2]
Treatment[edit | edit source]
For adults, the use of continuous positive airway pressure (CPAP) is the most effective treatment
- Adherence to nightly CPAP use can result in near complete resolution of symptoms.
- For patients unable or unwilling to use CPAP or those who will be unable to access electricity reliably, custom fitted and titrated oral appliances can be used to bring the lower jaw forward and relieve airway obstruction.
- Severe obstructive sleep apnea can be treated with BiPAP as well and is better tolerated by patients who require higher pressure settings (greater than 15 cm to 20 cm H2O).
- For all patients, it is important to address any concomitant nasal obstruction with nasal steroids for allergic rhinitis or surgically for nasal valve collapse.
- For obstructive sleep apnea with a strong positional component. Positioning devices to keep a patient on his or her side can be an option.
- Weight loss is recommended and can often decrease the severity of obstructive sleep apnea, it is not usually curative by itself.
- The primary treatment for obstructive sleep apnea in a child is tonsillectomy and adenoidectomy. The consideration for surgery should be balanced with the severity of symptoms, physical exam, and age. In mild cases, a trial of montelukast and nasal steroids may be enough to reduce the apnea-hypopnea index to goal.
- There are surgical options for adults, but these are usually reserved for severe obstructive sleep apnea and patients unable to tolerate noninvasive treatment modalities due to surgical risks and varying efficacy.[2]
Evaluation[edit | edit source]
- Nighttime in-laboratory Level 1 polysomnography (PSG) is the standard gold test for diagnosis of obstructive sleep apnea. During the test, patients are monitored with EEG leads, pulse oximetry, temperature and pressure sensors to detect nasal and oral airflow, respiratory impedance plethysmography or similar resistance belts around the chest and abdomen to detect motion, an ECG lead, and EMG sensors to detect muscle contraction in the chin, chest, and legs. A hypopnea can be based on one of two criteria. It can either be a reduction in airflow of at least 30% for more than 10 seconds associated with at least 4% oxygen desaturation or a reduction in airflow of at least 30% for more than 10 seconds associated with at least 3% oxygen desaturation or an arousal from sleep on EEG.[2]
Image R; Polysomnography testing child.
2. Home sleep tests (HST) have gained popularity due to their relative accessibility and lower cost. They are appropriate for adults with a high pretest probability for sleep apnea and no significant medical comorbidities (advanced congestive heart failure, COPD, and neurologic disorders). These are level 3 sleep tests consisting of pulse oximetry, heart rate monitoring, temperature and pressure sensors to detect nasal and oral airflow, resistance belts around the chest and abdomen to detect motion, and a sensor to detect body position.[2][7]
Other testing may include
- History: possible risk factors, co-morbidities, snoring, and what a normal night of sleep is like to him/her.[8]
- Indices: AHI (apnea-hypopnea index), RDI (respiratory disturbance index)[3]
- Clinical Examination: nose, tonsils, palate, tongue, neck circumference, upper airways.[8] [9] Findings are predominantly inconclusive and requires training for proper assessment.[8]
- Questionnaires: Epworth Sleepiness Score (ESS) for daytime sleepiness; Berlin questionnaire for common OSA risk factors and symptoms.[8]
- Oximetry: analyze oxygen saturation of hemoglobin to help identify individuals unlikely to have OSA.[9]
Morbidities associated with OSA[edit | edit source]
- OSA induced biological changes include intermittent hypoxia, intermittent hypercapnia, intrathoracic pressure changes, sympathetic activation and sleep fragmentation.
- OSA can cause metabolic dysregulation, endothelial dysfunction, systemic inflammation, oxidative stress and hypercoagulation, and neurohumoral changes.
- There is evidence suggesting that OSA is independently associated with metabolic syndrome.
- OSA has been shown to increase the risk for systemic hypertension, pulmonary vascular disease, ischemic heart disease, cerebral vascular disease, congestive heart failure and arrhythmias[10]
Physical Therapy Management[edit | edit source]
Although there is little research providing sound evidence based physical therapy interventions for OSA at this time, it often goes undiagnosed providing opportunities for physical therapists to identify, educate and refer patients who present with signs and symptoms of OSA. Undiagnosed OSA is associated with increased risk of hypertension, cardiovascular disease, motor vehicle accidents and reduced quality of life[11].
Physical Therapists can educate patients on OSA:
- Signs and symptoms
- Risk factors
- Associated co-morbidities
- How to get diagnosed/tested
- Risks of undiagnosed OSA
Exercises For Obstructive Sleep Apnea[edit | edit source]
EXERCISES FOR THE TONGUE
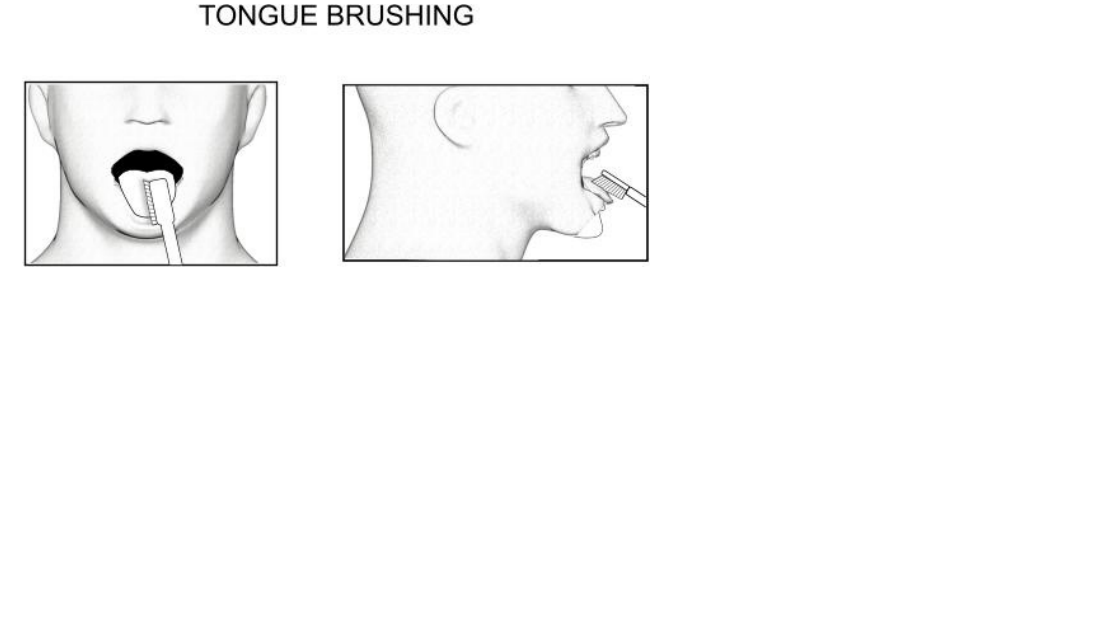
TONGUE BRUSHING
Method:
1. With your toothbrush brush the top and sides of your tongue, while your tongue is sitting on the floor of your mouth.
2. Repeat the individual sections 5 times each.
3. Complete the exercise three times daily.
Purpose – to strengthen the tongue muscles-with the added advantage of maintaining great oral hygiene!
TONGUE SLIDE
Method:
1. Looking straight ahead, position the tip of your tongue against the back of your top, front teeth.
2. Slide your tongue backward.
3. Repeat 10 times.
Purpose – to tone and strengthen the tongue and throat muscles. 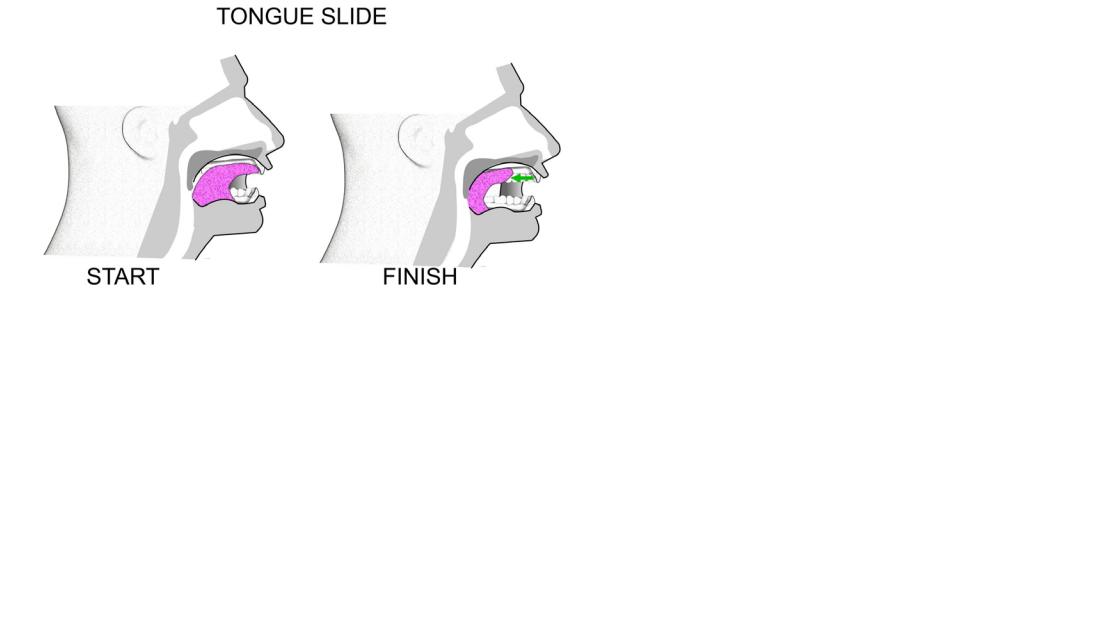 TONGUE FORCES
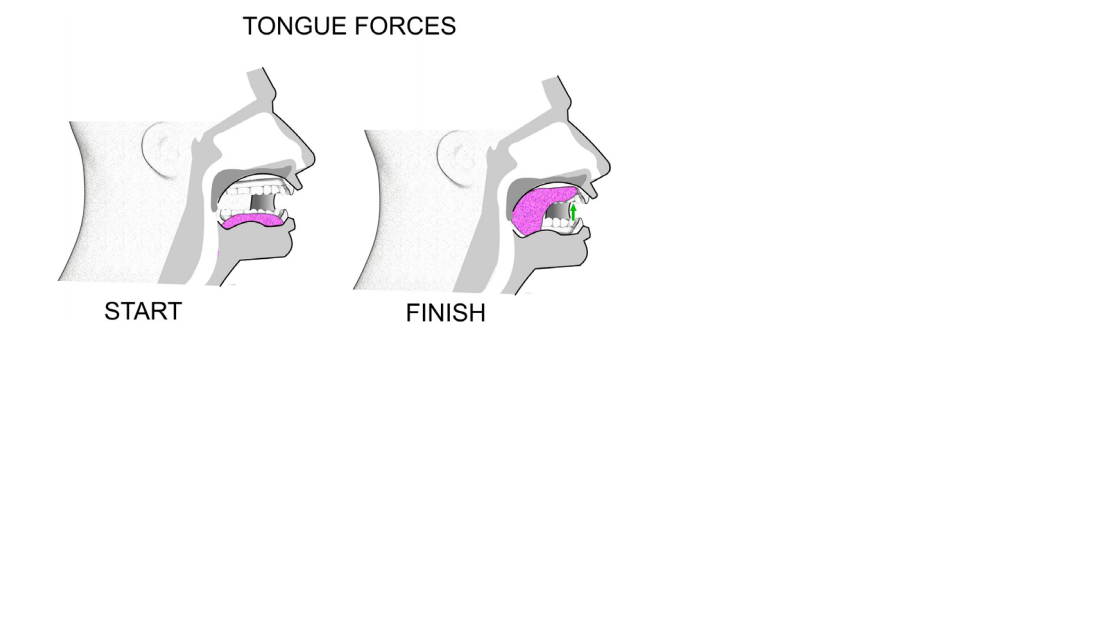
TONGUE FORCES
Method:
1. Forcibly suck your tongue upward until the whole tongue is against your palate.
2. Hold this position for 4 seconds.
3. Repeat 5 times.
Method:
1. Force the back of your tongue downward until the whole tongue is resting on the floor of your mouth.
2. Keep the tip of your tongue touching the back of your lower teeth.
3. Hold for 4 seconds.
4. Repeat 5 times.
Purpose - both of these exercises strengthen the tongue and tone your soft palate.
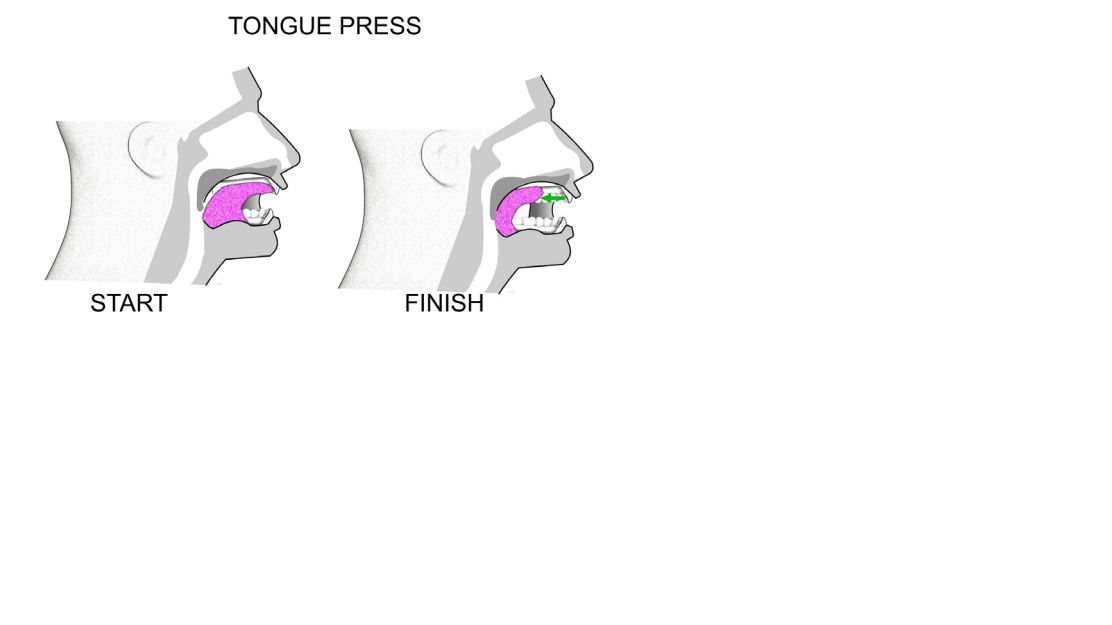
 TONGUE PRESS
TONGUE PRESS
Method:
1. Push your tongue against your hard palate (the top and front of your mouth).
2. Do this for 5 seconds.
3. Slide your tongue backward to the back of your mouth.
4. The initial third of your tongue should be against your hard palate, not just the tip.
5. Keep your jaw open throughout the exercise.
6. Refrain from biting down - keep your teeth apart.
7. Repeat this movement 10 times.
8. Repeat 4 times a day.
Purpose – to strengthen the genioglossus (the main muscle used for sticking your tongue out), and to increase the strength in the hyoid muscles and bone. The hyoid bone is located in the centre of the neck. It sits between the chin and thyroid cartilage.
The exercise assists by putting the hyoid bone in the correct position and keeping it there1.
The hyoid bone is a free moving, u-shaped bone in the neck. The volume of the tongue should reduce too.
Differential Diagnosis[edit | edit source]
Other diagnoses, especially other sleep disorders, may present as OSA due to similar symptoms (ex: fatigue, excessive sleepiness, HTN, sleep disturbance).[12] Alternative diagonses include:
- Nocturnal Frontal Lobe Epilepsy[13]
- REM Behaviour Disorder[14]
- Periodic Limb Movement Disorder[14] [3]
- Central Sleep Apnea[14] [3]
- Insomnia[9]
- Aging and Age-Related Changes (sleeping less, tiredness, nocturia)[9]
- Medications (side effects, multiple prescriptions)[9]
- Hypothyroidism[9] [3]
- Narcolepsy[15] [3]
- Shift Work Sleep Disorder (SWSD)[15]
- Idiopathic Hypersomnia[15]
- Asthma[3]
- Gastroesophageal Reflux Disease (GERD)[3]
- Chronic Obstructive Pulmmonary Disease (COPD)[3]
- Depression[9] [3]
Case Reports/ Case Studies[edit | edit source]
1. Daoulah A, Ocheltree S, Al-Faifi S, Ahmed W, Asrar F, Lotfi A. Sleep apnea and severe bradyarrhythmia – an alternative treatment option: a case report. J Med Case Reports 2015; 9(1): 113-117.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4437673/ (OSA and Bradyarrhythmia)
2. Guimarães T, Colen S, Cunali P, Rossi R, Dal-Fabbro C, Ferraz O, et al. Treatment of obstructive sleep apnea with mandibular advancement appliance over prostheses: A case report. Sleep Science 2015;8(2):103-106.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4608885/ (Treatment of OSA with Mandibular Appliance)
3. Fang H, Miao N, Chen C, Sithole T, Chung M. Risk of Cancer in Patients with Insomnia, Parasomnia, and Obstructive Sleep Apnea: A Nationwide Nested Case-Control Study. J Cancer 2015;6(11):1140-1147.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4615350/ (OSA and Cancer)
4. Cadby G, McArdle N, Briffa T, Hillman D, Simpson L, Knuiman M, et al. Severity of OSA Is an Independent Predictor of Incident Atrial Fibrillation Hospitalization in a Large Sleep-Clinic Cohort Chest. 2015;148(4):945-952.
http://www.sciencedirect.com/science/article/pii/S0012369215502833 (OSA and A-fib)
5. Meuleners L, Fraser M, Govorko M, Stevenson M. Obstructive Sleep Apnea, Health-Related Factors, and Long Distance Heavy Vehicle Crashes in Western Australia: A Case Control Study. Journal of Clinical Sleep Medicine 2015; 11(4): 413-418.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4365454/ (OSA and MVA)
Resources[edit | edit source]
American Sleep Apnea Association
American Sleep Association (ASA)
References[edit | edit source]
- ↑ 1.0 1.1 Strohl KP. Sleep Apnea [Internet]. Kenilworth (NJ): Merck & Co., Inc.; c2016 [cited 2016 Mar 30]. Available from: http://www.merckmanuals.com/home/lung-and-airway-disorders/sleep-apnea/sleep-apnea
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 Slowik JM, Collen JF. Obstructive Sleep Apnea.(2019)Available from:https://www.ncbi.nlm.nih.gov/books/NBK459252/ (last accessed 5.10.2020)
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 3.9 Downey III R, Rowley J, Wickramasinghe H, Gold P. Obstructive Sleep Apnea Differential Diagnoses. Emedicinemedscapecom. 2016. Available at: http://emedicine.medscape.com/article/295807-differential. Accessed April 9, 2016.
- ↑ Lam J, Sharma S, Lam B. Obstructive sleep apnea: Definitions, epidemiology & natural history. Indian J Med Res 2010;131:165-170. http://pharexmedics.com/wp-content/uploads/2015/11/sleepapnea_ebook.pdf (accessed 3 April 2016).
- ↑ Epstein L, Kristo D, Strollo Jr. P, Friedman N, Malhotra A, Patil S, et al. Clinical Guideline for the Evaluation, Management and Long-term Care of Obstructive Sleep Apnea in Adults. Journal of Clinical Sleep Medication 2009; 5(3): 263-276. http://pharexmedics.com/wp-content/uploads/2015/11/sleepapnea_ebook.pdf (accessed 3 April 2016).
- ↑ Radiopedia Adenoid Facies Available from:https://radiopaedia.org/articles/adenoid-facies-2 (last accessed 6.10.2020)
- ↑ Shayeb M, Topfer L, Stafinski T, Pawluk L, Menon D. Diagnostic accuracy of level 3 portable sleep tests versus level 1 polysomnography for sleep-disordered breathing: a systematic review and meta-analysis. Canadian Medical Association Journal 2013; 186(1):E25-E51. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3883848/pdf/18600e25.pdf (accessed 7 April 2016).
- ↑ 8.0 8.1 8.2 8.3 Maurer J. Early diagnosis of sleep related breathing disorders. GMS Current Topics in Otorhinolaryngology- Head and Neck Surgery 2010; 7(3): 1-20. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3199834/ (accessed 7 April 2016).
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 9.6 Culpepper L, Roth T. Recognizing and managing obstructive sleep apnea in primary care. Prim Care Companion J Clin Psychiatry 2009; 11(6): 330-338. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2805569/ (accessed 9 April 2016)
- ↑ Vijayan VK. Morbidities associated with obstructive sleep apnea. Expert review of respiratory medicine. 2012 Oct 1;6(5):557-66.Available from:https://www.medscape.com/viewarticle/775550 (last accessed 6.10.2020)
- ↑ Young T, Peppard P, Gottlieb D. Epidemiology of Obstructive Sleep Apnea. Am J Respir Crit Care Med 2002;165(9):1217-1239. http://www.atsjournals.org/doi/full/10.1164/rccm.2109080#.Vu73OZMrKYU (accessed 20 March 2016).
- ↑ Culpepper L, Roth T. Recognizing and managing obstructive sleep apnea in primary care. Prim Care Companion J Clin Psychiatry 2009; 11(6): 330-338. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2805569/ (accessed 9 April 2016).
- ↑ Cho J, Kim D, Noh K, Kim S, Lee J, Kim J. Nocturnal frontal lobe epilepsy presenting as obstructive type sleep apnea. J Epilepsy Res 2011; 1(2): 74-76. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3952334/ (accessed 8 April 2016)
- ↑ 14.0 14.1 14.2 Booth A, Djavadkhani Y, Marshall N. A critical review of the treatment options available for obstructive sleep apnoea: an overview of the current literature available on treatment methods for obstructive sleep apnoea and future research directions. Bioscience Horizons 2014;7(0):1-8. http://biohorizons.oxfordjournals.org/content/7/hzu011.full.pdf (accessed 4 April 2016).
- ↑ 15.0 15.1 15.2 McWhirter D, Bae C, Budur K. The assessment, diagnosis, and treatment of excessive sleepiness: practical considerations for the psychiatrist. Psychiatry (Edgmont) 2007;4(9): 26-35. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2880940/ (accessed 9 April 2016).