Scoliosis
Top Contributors - Lucas De Bondt, Amrita Patro, Lydia Xenou, Gregory Maes, Lucinda hampton, Kim Jackson, Nikhil Benhur Abburi, Admin, Selena Horner, Lieselot Longe, Oyemi Sillo, Ellen De Boitselier, Evan Thomas, Aminat Abolade, Liese Bosman, Jason Coldwell, Laure VanderDonckt, 127.0.0.1, WikiSysop, Blessed Denzel Vhudzijena, Linde Van Droogenbroeck, Ginika Jemeni, Scott Buxton, Ellen Hopmans, Derycker Andries and Vidya Acharya
Search Strategy[edit | edit source]
Keywords: Scoliosis, physical therapy, prevalence, rehabilitation, physiotherapy,…
Databases: PubMed, Pedro, Web of Knowledge, Cochrane Library, Library of the VUB, Medscape, ...
Definition/Description[edit | edit source]
Scoliosis is a three-dimensional deformative abnormality of the spine. Scoliosis is defined by the Cobb angle of spine curvature in the coronal plane, and is often accompanied by vertebral rotation in the transverse plane and hypokyphosis in the sagittal plane. These abnormalities in the spine, costal-vertebral joints, and the rib cage produce a ‘convex’ and ‘concave’ hemithorax. The rotation component starts when the scoliosis becomes more pronounced. This is called a torsion-scoliosis, causing a gibbus.
Scoliosis can be present from birth. It is then called congenitive scoliosis. Congenital scoliosis represents a spinal malformation due to defects of formation, segmentation or mixed ones. It is characterised by a longitudinal and rotational imbalance.[1]
Other sorts of scoliosis can be developed during growth, any causes for this are still not found. We then speak of Weiss Scoliosis 2011, 6:17. Approximately 85% of cases are idiopathic. Based on the age of presentation, scoliosis is further categorised as infantile, juvenile or adolescent idiopathic. Adolescent idiopathic scoliosis (AIS) has the highest prevalence of the three categories. This type of scoliosis is present at age ten and lasts till the end of growth. Its prevalence is dependent on the curvature of the spine and gender of the patient.[2] Epidemiological studies have demonstrated that IS is significantly more frequent in girls than boys, reaching a ratio of 4 : 1.26 Anwer et al. (2015) described a prevalence of 2,5% with a Cobb angle larger then 10 degrees. They also stated that a variety of risk factors may result in a higher curve progression. These factors include the following: female gender, age of 10–12 years, absence of menarche, presence of thoracic curves, curve size at presentation >25 degrees, Risser sign of 0-1, and residual growth potential.[3]
Clinically Relevant Anatomy[edit | edit source]
The vertebral columm normally consists of 24 separate bony vertebrae, together with 5 fused vertebrae that form the sacrum, and usually 4 fused vertebrae that form the coccyx. These 24 separate vertebrae can be divided in three categories: 7 cervical vertebrae, 12 thoracic vertebrae and 5 lumbar vertebrae. Variations can occur such as Hemivertebrae and fused vertebrae. The anterior pillar of the spine has weight-bearing and shock-absorbing functions. There is an intervertebral disc between adjacent vertebral bodies; with the exception of the first and second cervical vertebrae. Each disc consists of a nucleus pulposis surrounded by an annulus fibrosis. The posterior pillar comprises the apophyseal joints that are formed by the articular facets on the articular processes.
When viewed from the side, the vertebral column displays five curves in the upright posture:[4]
• Cervical curves
There are two normally occurring curves in the cervical spine: the upper cervical curve extending from the occiput to the axis, and the longer lordotic curve of the lower cervical spine extending from the axis to the second thoracic vertebrae. The lower cervical curve is convex forwards and is the reverse of the upper cervical curve.
• Thoracic curve
This curve is concave forwards, extending from T2 to T12. The concavity is due to greater depth of the posterior parts of the vertebral bodies in this region. In the upper part there is often a slight lateral curve with the convexity directed to either the right or left.
• Lumbar curve
The lumbar curve is convex forwards and extends from T2 to the lumbosacral junction.
• Sacral curve
The curve extends from the lumbosacral junction to the coccyx. Its anterior concavity faces downwards and forwards.
Epidemiology /Etiology[edit | edit source]
Scoliosis may be structural or non-structural.
I. Non-structural scoliosisCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
A non-structural curve will usually have no rotational element, being a pure coronal plane deformity. A non-structural scoliosis may be due to:
- Pelvic tilt secondary to leg length inequality
- Pain or irritation (seen with disc prolapsed and other painful conditions, such as osteoid osteoma, typically triggering muscle spasm).
The key feature of non-structural scoliosis is that the curve is reversible. It will spontaneously straighten when the underlying cause is corrected or removed. For example: In the case of pelvic tilt scoliosis, the curve will disappear when the pelvis is leveled and this can be achieved by sitting the patient or by equalizing any leg-length-discrepancy with blocks.
II. Structural scoliosisCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
A structural curve will usually have a rotational element. The structural scoliosis is irreversible and may be classified according to the underlying etiology:
- Idiopathic scoliosis (70%) = Scoliosis without detectable underlying cause. This is the most common type.
- Congenital scoliosis (15%) = The scoliosis is present from birth. The vertebral disorders that cause congenital scoliosis may be due to either failure of formation or failure of segmentation or a combination of these, leading to a mixed deformity.
- Neuromuscular scoliosis (10%) = Scoliosis due to neuromuscular diseases such as cerebral palsy, poliomyelitis,….
- Trauma, tumour and infection are also possible causes, but are not frequently encountered.
- Rare conditions, including hereditary and mesenchymal abnormalities such as neurofibromatosis, Marfan’s syndrome, EhlerseDanlos syndrome etc. make up the remainder.
Characteristics/Clinical Presentation[edit | edit source]
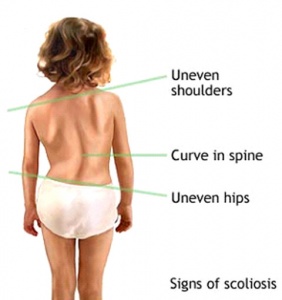
Symptoms for scoliosis can be:
- Sideways curvature of the spine
- Sideways body posture
- One shoulder raised higher than the other
- Clothes not hanging properly
- Local muscular aches
- Local ligament pain
Diagnostic Procedures[edit | edit source]
The most common diagnostic procedures are:
- X-rays of the spine
- Measuring the leg length.
- A bone scan, MRI, or computed tomography (CT) scan may be necessary in difficult diagnostic problems.
Examination[edit | edit source]
Screening procedures for scoliosis are done either by the Adam forward bend test or using other optical techniques like a scoliometer, while the radiographic measurement of Cobb angle is considered as the golden standard.
The Cobb angle is the angle between lines drawn along the upper end plate of the most tilted vertebrae above the curve’s apex and the lower end plate of the most tilted vertebrae below the apex.
The Adam forward bend test can be performed in both standing and sitting position. In standing position, the examined person is asked to bend forward looking down, keeping the feet together, the knees straightened, shoulders loose and hands positioned in front of knees or shins with elbows straight and palms opposed. If the scoliosis is present in both standing as bending position, the scoliosis is structural. If the scoliosis is present in standing position but disappears when the examined person is bended forward, the scoliosis is not structural.
In the sitting position, the examined person is seated on a chair with a height of 40 cm. The examined person is asked to bend forward and place his head between the knees, with his shoulders loose, elbows straight and hands positioned between the knees.
The scoliometer is an inclinometer designed to measure trunk asymmetry, or axial trunk rotation. It’s used at three areas: at upper thoracic (T3-T4), main thoracic (T5-T12) and at the thoraco-lumbar area (T12-L1 or L2-L3). If the measurement is equal to 0°, there is a symmetry at the particular level of the trunk. An asymmetry at the particular level of the trunk is found, if the scoliometer measurement is equal to any other valueCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title.
Medical Management
[edit | edit source]
Management of congenital scoliosis
The therapeutic options in cases of congenital scoliosis include conservative or surgical approaches.
I. Conservative treatment
With regard to conservative treatment of patients with congenital scoliosis, it should be noted that there are limited data available in the literature. A review (level of evidence 2) concluded that patients with specific types of segmentation failures, like unilateral unsegmented bars, will not benefit from conservative treatment, while the same applies to formation failures with curves of > 20 degrees in infancy. Nevertheless, there are reports that a conservative approach might be beneficial in mild cases with formation failures in the first three years of life. Furthermore, the review concluded that in patients with formation failures further investigation is needed to document where a conservative approach (bracing treatment) would be necessary. In general, most congenital scoliotic curves are not flexible and therefore are resistant to repair with bracing. For this reason, the use of braces mainly aims to prevent the progression of secondary curves that develop above and below the congenital curve, causing imbalance. In these cases, they may be applied until skeletal maturityCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title.
II. Surgical treatment
Spinal surgery in patients with congenital scoliosis is regarded as a safe procedure and many authors claim that surgery should be performed as early as possible to prevent the development of severe local deformities and secondary structural deformities that would require more extensive fusion later. Most of the time Surgery is performed during adolescence, but newer techniques allow good correction to be accomplished into early adulthood. The goals for surgical treatment are to prevent progression and to improve spinal alignment and balance. The hips and shoulders should be level, and the head over the sacrum while maintaining sagittal alignment. The spine is corrected with a combination of rods, hooks, screws and wires while being fused by bone graft – either from the patient, a cadaver or artificially. On the other hand, early and late complications are also described in literature, concerning not only intraoperative and immediate postoperative problems, but also the safety and efficacy of the spinal instrumentation and the possibility of developing neurological disorders and the long-term effect these may have on both lung function and the quality of life. A review (2011, level of evidence 2) concluded that patients with segmentation failures should be treated surgically early, according to the rate of deformity formation and certainly before the pubertal growth spurt to try to avoid cor-pulmonale, even though there is lack of evidence for that in the long-termCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title.
Physical Therapy Management
[edit | edit source]
Scoliosis is not just a lateral curvature of the spine, it’s a three dimensional condition. To manage scoliosis, we need to work in three planes: the sagittal, frontal and transverse. Different methods have already been studied.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
The conservative therapy consists of: physical exercises, bracing, manipulation, electrical stimulation and insoles. There is still discussion about the fact that conservative therapy is effective or not. Some therapists follow the ‘wait and see’ method. This means that at one moment; the Cobb degree threshold will be achieved. Then, the only possibility is a spinal surgery.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
The physical therapist has three important tasks: to inform, advice and instruct.
For the treatment of scoliosis, it’s not only important to do the correct exercises but the physical therapist also needs to inform the patient about his/her situation (if the patient is still a child, then he needs to inform the parents too). An educational program makes sure that the therapy accuracy from the patient improves. Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Some physical therapists recommend a brace to prevent the worsening of the scoliosis. An often used brace is the Milwaukee brace. Nevertheless the evidence for bracing is controversial. Maruyama T., Nakao Y. and Takeshita T. studied the effect of bracing in a review (2011). They compared brace treatment with no-treatment, other conservative treatments or surgery. The analyzed outcome measures were the radiological progression of the curve, surgery and quality of life. Results demonstrate that brace treatment is better than no-treatment (observation) or electrical stimulation. There is also no negative influence on the quality of life of patients with an idiopathic scoliosis. We can conclude that bracing is recommended as a treatment for female patients with a Cobb angle of 25-35°. The evidence level of some studies in the review was limited, so further research is necessary.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
In the literature there is evidence that exercises have beneficial effects on patients with idiopathic scoliosis.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
The aims of the physical therapy consist of:Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title[Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
• Autocorrection 3D
• Coordination
• Equilibrium
• Ergonomy
• Muscular endurance/ strength
• Neuromotorial control of the spine
• Increase of ROM
• Respiratory capacity/ education
• Side-shift
• Stabilisation
In the literature there are different exercise therapies.
An important one is the conservative three-dimensional Schroth method consisting of curve-specific exercises and corrective breathing techniques. The purpose of these exercises is to derotate, deflex and to correct the spine in the sagittal plane while elongating the spine. The patient needs to be focused about re-establishing spinal symmetry. The key to a successful therapy is to work consistently to correct the spine. Another – difficult- part of the therapy is to learn to shorten the muscles on the convex side of the spine and lengthen the muscles on the concave side of the side. This because the muscles become imbalanced on opposite sides.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
The exercise position approaches the functional/structural threshold. Schroth therapy takes advantage of the overcorrected positions. Basic corrections are reviewed by using mirrors in front and at the back of the patient. This posture requires concentration and coordination, applying the correct breathing, and well-adapted muscle length and tension.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
But there are also other exercises that have been found effective. Scientific Exercises Approach to Scoliosis (SEAS) exercises is for example been found effective in reducing the rate of progression of scoliosis compared with usual care and help to avoid brace prescription. Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
The SEAS exercises are, according to the Italian Scientific Spine Institute (ISICO), based on a specific form of Active Self-correction (ASC), that is taught individually to each single patient. This is to achieve the maximum possible correction. ASC is then associated with stabilising exercises that include neuromotor control, proprioceptive training and balance. The exercises are also incorporated into their daily living activities. SEAS approach does also involve the parents. They are getting together with the patiënt a cognitive-behavioral approach to maximize compliance to treatment.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
We mentioned earlier that one of the aims is respiratory capacity/education. The severity of the curvature can cause a pressure on airways and lungs. The patient can experience trouble while breathing. Therefore the therapist must insert breathing exercises to complete his/her management. If the risk of pulmonary dysfunction (as a result of the pressure of the spine) is too high, surgery is indicated.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Solache-Carranco and M.G. Sánchez-Bringas (2011) studied the effectiveness of a respiratory rehabilitation program in children with scoliosis. This are the techniques that they used:
- Respiratory education techniques (abdominal-diaphragmatic ventilation, thoracic mobilisation, ventilation at rest and during activities of daily living). This for mobilisation and prevention of stiffness of chest and skeletal muscles.
- Postural drainage and vibration to evacuate mucus and decrease the resistance of the airways.
- Relaxation techniques to make sure that the patients would have better control of respiration (to counteract dyspnea).
They found that the respiratory rehabilitation had a positive effect on increasing pulmonary function of children with scoliosis.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Management of non–structural scoliosisCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Pilates: This intervention was divided in three parts:
1. Preparation (warming up + stretch)
Warming –up consisted of eight minutes walking on a treadmill or an elliptical machine.
After the warming –up each patient had to do some stretching exercises:
- Spine forward stretching:
- The patient sits on the floor with a straight back and the legs stretched. The patient has to bring her trunk forwards
- Goal: Stretching the posterior muscle chain and mobilizing the vertebral spine
- Upper rolling
- The patient lies supine with the arms besides the body. The patient has to raise both legs till the toes touches the floor. Than this person has to unroll her spine slowly (vertebra by vertebra)
- Goal: stretching the posterior chain, mobilizing the spine and strengthen the abdomen
- Child position
- The patient sits in a four support position and has to stretch her spine, her arms are stretched and she has to push her hands against the floor. Then she has to lower her spine.
- Goal: Stretching the thoracic paravertebral, lumbar and gluteal regions and mobilizing the vertebral spine
- Forward leg pull
- The patient sits in a four support position. Then she has to raise the right arm and leg while the spine stays aligned. Than the same exercise but change arm and leg.
- Goal: Stretching the concavity of the vertebral spine.
2. Specific exercises:
For these exercise they made use of Swiss balls, FlexBall Quarks,.. It’s important that the patients learn to breathe right during exercise.
- Hip movements with a large ball (65 cm diameter)
- Goal: Strengthening the gluteal muscles and developing the equilibrium
- Inverted abdominal skills with a ball (55 cm diameter)
- Goal: Strengthening the infraabdominal region and the ischiotibial muscles.
- Rising into a seated position:
- Goal: Strengthening the M. rectus abdominis
- Lateral spine movement on a step chair with a spring of 0.1410 kgf positioned in the rings to provide major resistance
- Goal: Stretching the lateral muscle chain according to the direction of convexity of the scoliosis
- Lateral spine movement:
- Goal: Stretching the lateral muscle chain according to the direction of convexity of the scoliosis
- Flexibility on the step chair with a spring of 0,1410 kgf positioned in the rings to provide major resistance:
- Goal: Mobilize the spine and stretching the paravertebral thorax and lumbar muscles
3. Returning to a relaxed position (relaxation) :
It consist out three movements, the patient has to repeat each exercise three times for five minutes.
All exercises has to be performed rapidly. The purpose of these exercises are metabolic recovery and relaxation of the used muscles.
Prognosis[edit | edit source]
Surgery
The outcome needs to be age matched since the demands of daily life, professional performance, and leisure activities vary substantially in the different age groups. Most of the patients who are still professionally active do not return to their previous work if it was a physically demanding job, but almost all of those had already stopped working before the surgery, because of pain limitations. When analyzed, regarding their overall daily activity by different questionnaires, most of these patients irrespective of age have improved in almost all categories of quality of life, and the use of regular pain medication is reduced substantially in more than 70% of these patientsCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title.
However for the elderly the outcome is less positive because of the age. The major problem of these patients after surgery, once surgical complications and implant failures have not occurred, is the residual back pain mostly as an expression of muscular spasms and pain due to unbalanced or chronic contractures of the paravertebral musclesCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title.
Bracing
Whether brace treatment for scoliosis is successful is often described using the curve progression of more than 5° before skeletal maturity as a benchmark for bracing failure rather than spine surgeryCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. Some use 10° of curve progression or preventing the curve from reaching 45° at skeletal maturityCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title.
The outcome data should be determined from the percentage of patients with: less than 5° or greater than 6° of progression at maturity, curves exceeding 45° at maturity, and progression resulting in the recommendation for surgery. Bracing studies should have a minimum of 2 years follow up beyond skeletal maturity. The first study to use these criteria determined a brace should prevent progression in 70% of patients to be considered effective]. Regardless of the recommended standardized parameters, the goal of bracing idiopathic curves remains consistent: control the curve, prevent progression, and avoid surgical interventionCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title.
Recent Related Research (from Pubmed)[edit | edit source]
References[edit | edit source]
- ↑ Burnei et al., J Med Life. 2015 Jul-Sep; 8(3): 388–397.Congenital scoliosis: an up-to-date, J Med Life. 2015 Jul-Sep; 8(3): 388–397. (Level of Evidence 4)
- ↑ Joehaimey Johari et al., Relationship between pulmonary function and degree of spinal deformity, location of apical vertebrae and age among adolescent idiopathic scoliosis patients, Singapore Med J 2016; 57(1): 33-38 (Level of Evidence 3)
- ↑ Anwer et al., Effects of Exercise on Spinal Deformities and Quality of Life in Patients with Adolescent Idiopathic Scoliosis, 2015 (Level of evidence: 1A)
- ↑ Alison Middleditch et al., Functional Anatomy of the Spine 2005 2-6p.