Scleroderma Case Study: Difference between revisions
No edit summary |
No edit summary |
||
| Line 77: | Line 77: | ||
Measurement of Oral Aperture<sup>9</sup> | Measurement of Oral Aperture<sup>9</sup> | ||
<sup></sup> | <sup></sup> | ||
<sup></sup> | <sup></sup> | ||
| Line 157: | Line 157: | ||
Based on Evaluation and examination information patient should be educated on proper protection of affected joints with education on temperature monitoring to reduce symptoms. Light range of motion should be built in to the intervention in a safe manor to preserve range that will progress to light strengthening of affected joint as long as joint integrity is not in jeopardy. | Based on Evaluation and examination information patient should be educated on proper protection of affected joints with education on temperature monitoring to reduce symptoms. Light range of motion should be built in to the intervention in a safe manor to preserve range that will progress to light strengthening of affected joint as long as joint integrity is not in jeopardy. | ||
<br> | |||
== Intervention == | == Intervention == | ||
| Line 263: | Line 263: | ||
Immunosuppressants - treatment during the acute phase of the disease<sup>10</sup> | Immunosuppressants - treatment during the acute phase of the disease<sup>10</sup> | ||
<br> | <br> | ||
== Outcomes == | == Outcomes == | ||
Findings Over time | Findings Over time | ||
== Discussion == | == Discussion == | ||
Revision as of 03:19, 30 March 2015
Author/s[edit | edit source]
Catelin Infante, Jessica Frederick, Kristin Casagrand, Jarrod Smith from the Bellarmine University Physical Therapy Program's Pathophysiology of Complex Patient Problems Project.
Patient Characteristics[edit | edit source]
- Demographic Information: (occupation/vocation, gender, age, etc.)
Native American
Female
Born and raised in Oklahoma
Works in a factory
Thirty-five years old
Family history of rheumatoid arthritis on mother's side
- Medical diagnosis if applicable
Scleroderma
- Co-morbidities
Hypertension, Type II Diabetes
- Previous care or treatment
Previous physical therapy for low back pain
Examination[edit | edit source]
- Subjective
Ms. Smith comes into the clinic complaining of joint pain and muscle weakness, especially in her hands, hips and shoulders1. She explains that she has been having trouble making it through a full day of work because her body feels limited and she just cannot reach as well for boxes at her job because "her arms won't go up that far". She also has noticed that she gets out of breath and sometimes has chest pain when she lifts a lot too quickly2. Mrs. Smith indicates that her fingers often feel very swollen and stiff and sometimes feel "stuck" in a bent position1. She reports that for several months she has been getting a really cold, numb feeling in her fingers throughout the day, especially when she is sitting in the air conditioning at her office3. Overall, she has just not felt well for the past few months either. When she eats, she has trouble fully opening her mouth to put food in2. Then, when she lies down at night after dinner, she gets a feeling of heartburn and sometimes feels she has to vomit1. However, she says she has been eating poorly lately, so it's probably her fault she hasn't felt well. Additionally, Mrs. Smith reports losing 20 pounds in the past month without any lifestyle changes. Her goals for therapy are to decrease her joint pain and to get her muscles stronger so she doesn't struggle at work any longer. Her focus is on getting her hands and arms "back to normal" because they are what she uses most in her job.
- Self-Report Outcome Measures
Health Assessment Questionnaire Disability Index (HAQ-DI)4: 1.1
Disabilities of Arm, Shoulder, and Hand Questionnaire (DASH)5: 34
Verbal Pain Intensity Scale: "Severe pain"
- Physical Performance Measures
Grip strength (R)6: 20.7 kg
Grip strength (L)6: 19.18 kg
Pinch strength (R)6: 4.27 kg
Pinch strength (L)6: 3.98 kg
Oral aperture7: 28 mm
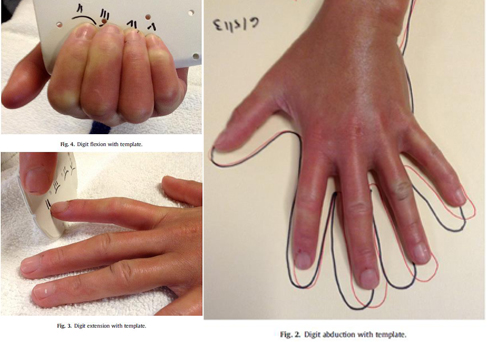
Measurement of Oral Aperture9
- Objective
MMT: WNL except for the following
4/5 finger and thumb abduction, adduction, flexion, extension
4/5 wrist flexion and extension
3+/5 shoulder flexion and abduction
3+/5 hip flexion and abduction
ROM: WNL except for the following
Decreased flexion and extension in all finger MCP and IP joints
Decreased wrist flexion and extension
Decreased hip extension and abduction
Reflexes: WNL
Sensation: Decreased facial sensation
- ICF Findings
Impairments1,2,8
Patient has stiffening around fingers and what appears to be finger flexion contractures developing
Patient has noticeable hard deposits palpated around UE joints
Patient has slurred speech due to difficulty fully opening mouth. The skin around the face is thickened and has begun to cause puckering
Pt has dyspnea and chest pain upon exertion
Activity Limitations1,2,8
Patient is unable to complete activities in supine secondary to reflux symptoms
Patient is unable to complete overhead activities due to decreased shoulder ROM
Patient is unable to complete more than 30 minutes of repetitive movements due to fatigue, muscle weakness and joint pain
Environmental Factors8
Patient is employed as a packer at a plastics company
Patient is a smoker of 20 years
Clinical Impression[edit | edit source]
- After Ms. Smith's assessment, we have determined that she has decreased range of motion in her fingers and wrists, decreased cardiovascular endurance, decreased muscle mobility, as well as increased muscle weakness and fatigue. All of these impairments have impacted her functional ability to do activities at home and in the work place. Physical therapy could benefit Ms. Smith by improving her impairments that were found and by providing patient education on management of her condition. The interventions during PT would include active joint range of motion, strengthening exercises and aerobic exercises to improve endurance, as well as education on a home exercise program and management of the symptoms of her condition. With the help of physical therapy, Ms. Smith would likely be able to reach her goals for improving her strength and endurance and decreasing her joint pain so that she can particpate in more activities at home, work and in the community.
Summarization of Examination Findings[edit | edit source]
Targeted intervention for Physical therapy for this patient would be improving available range of motion, joint protection and preservation along with patient education.
Based on Evaluation and examination information patient should be educated on proper protection of affected joints with education on temperature monitoring to reduce symptoms. Light range of motion should be built in to the intervention in a safe manor to preserve range that will progress to light strengthening of affected joint as long as joint integrity is not in jeopardy.
Intervention[edit | edit source]
- Phases of Interventions
Edematous Stage:
Patient Education (About the disease; treatment of Raynaud's disease - dress in layers, monitor temperature changes, avoid air conditioning if possible, avoid things that cause vasoconstriction like smoking, cold temperatures and emotional stress)10,11
Orthotic and adaptive equipment needs11,12
Light range of motion exercises11,12,13
Joint protection strategies (light weight splints)10
Fatigue management (Four P's of energy conservation - prioritize, plan activities, pace activities and promote correct posture through proper body mechanics)11
Sclerotic Stage:
Paraffin/heat modalities for hands and fingers (vascular system may be affected with this condition, so the patient might have a higher risk for burns)11,12,13,14
Passive range of motion exercises progressing to active-assisted range of motion, then to active range of motion, can add a sustained stretch for five seconds at end range (finger flexion/extension and abduction/adduction, wrist flexion/extension - can use hand clasp with wrist extension stretch)1,10,11,12,13
12
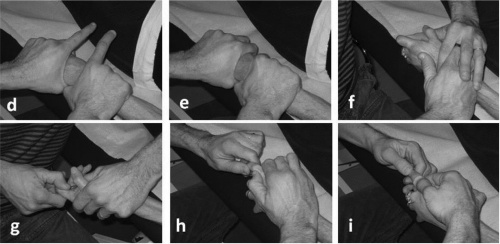
Soft tissue mobilizations13,14
Joint manipulations (Traction)11,12,13,14
14
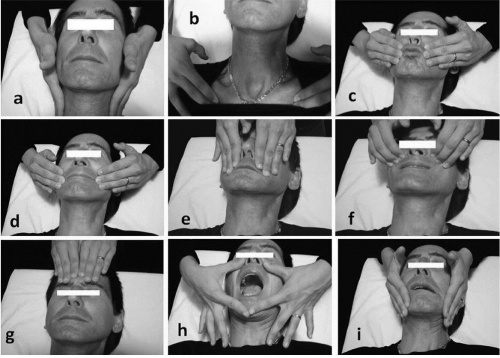
Kabat's method to improve mouth opening (activation of orbicularis oris, zygomaticus, levator labii, nasalis, frontalis and corrugator muscles by exaggerated facial movements) - progress from active-assisted ROM to active ROM11,13,14
14
Soft tissue massage13,14
Aquatic therapy (Upper and lower extremity range of motion and strengthening exercises, walking, squatting, marching, etc)10,14
Cycle ergometer12
Resistive training12,13
- Dosage and Parameters
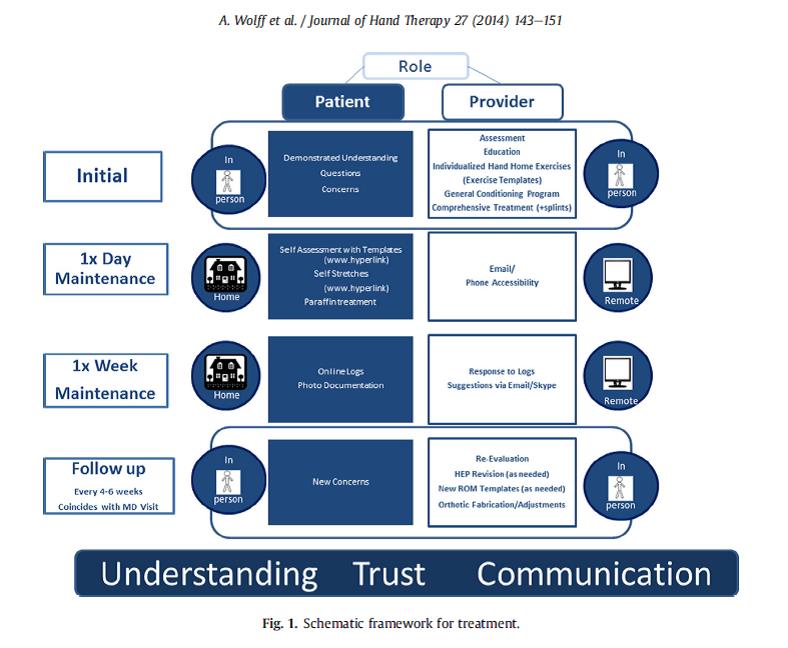
SMART framework - combines physical therapy sessions with self-management of care through a home exercise program. The PT session focuses on designing an individualized program for each patient in order to treat their specific impairments and goals. The sessions are planned less frequently during the week, but spaced out over a longer period of time. This is to help shift the focus of the care to self-managed that way the patient can manage their condition for the long-term. The HEP uses exercises, self-stretches and paraffin to help the patient manage their condition at home. The patient is given 4-5 exercises that are performed 1-2 times per day, for 5 days per week.12
12
Each physical therapy session is specific for each individual because of the varying presentation of scleroderma. The physician should be consulted frequently about the proper treatment for each patient.12,13,14
- Rationale for Progression
As the same for the dosage and parameters, each individual has a different presentation of scleroderma and the associated symptoms and impairments.12,13,14 Each individual should progress through their rehabilitation according to their reaction to the exercises. Each should be monitored closely, especially with the aerobic exercise, and progressed in a safe manner according to their bodies' response to exercise. The physical therapist must also consider the phase of the disease that the patient is in and their progression through the disease phases.
- Co-interventions if applicable
Occupational Therapy
Joint preservation principles1
Devices for independent living1
Medications
Disease modifying drugs (Penicillamine) - treatment of disease processes10
ACE inhibitors - treatment of acute hypertension/pulmonary hypertension and renal complications10
Nonsteroidal anti-inflammatory drugs (NSAIDs) - treatment of joint inflammation10
Antibiotics/Oral Tetracyclines (Minocycline, doxycycline) - treatment for disease by reduction of pain, severity of condition and quality of life10
Analgesics - treatment of pain10
Prazosin, Ilioprost and Cisaprost for Raynaud's Level A1
Methotrexate and Calcium channel blockers - treatment of Raynaud's Level B1,10
Immunosuppressants - treatment during the acute phase of the disease10
Outcomes[edit | edit source]
Findings Over time
Discussion[edit | edit source]
Summary Statement which should include related findings in the literature, potential impact on clinical practices
Related Pages[edit | edit source]
http://www.physio-pedia.com/Scleroderma
http://www.niams.nih.gov/Health_Info/Scleroderma/default.asp
http://www.scleroderma.org/site/PageNavigator/patients_whatis.html
http://www.mayoclinic.org/diseases-conditions/scleroderma/basics/definition/con-20021378
References[edit | edit source]
References will automatically be added here, see adding references tutorial.