Rupture Long Head Biceps: Difference between revisions
Leana Louw (talk | contribs) No edit summary |
Kim Jackson (talk | contribs) m (Text replacement - "[[Biceps brachii" to "[[Biceps Brachii") |
||
| (18 intermediate revisions by 4 users not shown) | |||
| Line 5: | Line 5: | ||
</div> | </div> | ||
== Introduction == | |||
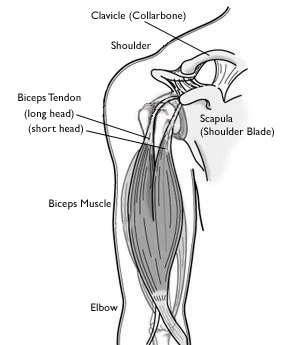
[[Image:A00031F01.jpg|right]]The [[Biceps Brachii|biceps brachii muscle]] has two heads, one originating from the coracoid process (short head) and the other from the supraglenoid tubercle of the scapula and superior labrum (long head biceps). The long head (LHB) contributes to the stability of the glenohumeral joint. The majority of biceps rupture involves the LH. Rupture of the LHB tendon can be treated conservatively. Patients generally recover successfully if they receive a timely diagnosis and treatment | |||
Chronic LHB rupture is defined as a tendon tear for more than 4 weeks. Chronic rupture may be due to missed diagnosis or failure of conservative treatment. MRI helps differentiate partial and complete tears of the biceps tendon<ref name=":1">Hsu D, Anand P, Chang KV. [https://www.ncbi.nlm.nih.gov/books/NBK513235/?report=printable Biceps tendon rupture]. StatPearls [Internet]. 2020 Apr 20.Available:https://www.ncbi.nlm.nih.gov/books/NBK513235/?report=printable (accessed 30.9.2021)</ref>. | |||
== Pathophysiology == | |||
[[File:Coronal section of the tendon of long head of biceps Primal.png|right|frameless|399x399px]] | |||
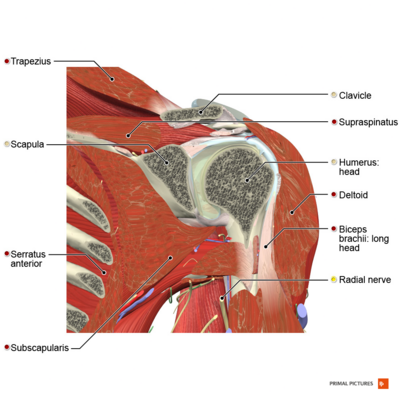
The LH originates at the supraglenoid tubercle and is attached to the dorsal aspect of the radial tuburosity.<ref name="p3">Shunke M, Schulte E, Schumacher U. Anatomische atlas Prometheus: Algemene anatomie en bewegingsapparaat. Bohn Stafleu Van Loghum: Nederland, 2005.</ref> It runs intra-articularly over the humeral head and follows the bicipital groove distal to the [[Glenohumeral Joint|glenohumeral joint]].<ref name="p8">Elser F, Braun S, Dewing CB, Giphart JE, Millett PJ. [https://drmillett.com/wp-content/uploads/articles/Anatomy%20Function%20Injuries%20and%20Treatment%20of%20the%20Long%20Head%20of%20Biceps%20Brachii%20Tendon%20.pdf Anatomy, function, injuries, and treatment of the long head of the biceps brachii tendon.] Arthroscopy: The Journal of Arthroscopic & Related Surgery 2011;27(4):581-92.</ref> It functions as dynamic stabilizer of the [[Glenohumeral Joint|glenohumeral joint]], as well as a depressor of the humeral head.<ref name="p2">Warner JJ, McMahon PJ. [https://journals.lww.com/jbjsjournal/Abstract/1995/03000/The_role_of_the_long_head_of_the_biceps_brachii_in.6.aspx The role of the long head of the biceps brachii in superior stability of the glenohumeral joint.] JBJS 1995;77(3):366-72.</ref> | |||
* Age, overuse, smoking, and corticosteroid use contribute to tendon degeneration and, later, tendinopathy. | |||
* The proximal tendon rupture in most cases occurs at the tendon-labral junction or the bony attachment<ref name=":1" />. | |||
Image 2: Coronal section of the tendon of long head of biceps. | |||
== Epidemiology == | |||
# Biceps tendon rupture mainly occurs in individuals between 40 and 60 years who already have a history of shoulder problems. | |||
# It mostly affects the dominant arm.<ref name="p2" /> | |||
# A biceps tendon tear can also occur in younger individuals, but usually after a traumatic fall on an outstretched arm, heavy weightlifting or consistently sport activities such as snowboarding and soccer.<ref name="p4">Quach T, Jazayeri R, Sherman OH, Rosen JE. [https://web.a.ebscohost.com/abstract?direct=true&profile=ehost&scope=site&authtype=crawler&jrnl=19369719&AN=52315050&h=zPKRB5jHHBp92ct%2bOL132SPmNQ6bHB6LgV0mIgg0iavWGv1pJgpy6sUhiy4LgNcZEhDDoIS9OXXP0qhuAc6uGQ%3d%3d&crl=c&resultNs=AdminWebAuth&resultLocal=E Distal Biceps Tendon Injuries.] Bulletin of the NYU hospital for joint diseases 2010;68(2).</ref><ref name="p5">Medscape. Biceps rupture. Available from: https://emedicine.medscape.com/article/327119-overview (accessed 06/01/2019).</ref> | |||
== | == Etiology == | ||
# LHB rupture is generally not due to a unique mechanism of injury but is highly correlated with rotator cuff disease. | |||
# Risk factors include age, smoking, obesity, use of corticosteroids, and overuse. Rare causes include the use of quinolones, diabetes, lupus, and chronic kidney disease.<ref name=":1" /> | |||
=== | == Characteristics/Clinical presentation == | ||
Patients with a long head biceps rupture report a wide variety of symptoms.<ref name="p5" /> | |||
== | Trauma:<ref name="p4" /> | ||
* Audible pop | |||
* Sharp anterior shoulder pain with or without snapping sensation<ref name="p5" /> | |||
* Pain:<ref name="p5" /> | * Pain:<ref name="p5" /> | ||
** With overhead activities | ** With overhead activities | ||
** Anterior shoulder pain that may get worse at night<ref name="p5" /> | ** Anterior shoulder pain that may get worse at night<ref name="p5" /> | ||
Associated pathologies that may lead to rupture of long head of biceps: | |||
*[[Rotator Cuff Tears|Rotator cuff tears]]<ref name="p7">Chen CH, Chen CH, Chang CH, Su CI, Wang KC, Wang IC, Liu HT, Yu CM, Hsu KY. [https://www.researchgate.net/profile/I_Chun_Wang/publication/228069967_Classification_and_analysis_of_pathology_of_the_long_head_of_the_biceps_tendon_in_complete_rotator_cuff_tears/ Classification and analysis of pathology of the long head of the biceps tendon in complete rotator cuff tears.] Chang Gung Med J 2012;35(3):263-70.</ref> | |||
* Tendonitis<ref name="p5" /> | |||
* Shoulder impingement<ref name="p5" /> | |||
* Popeye deformity<ref name="p5" /> | |||
* Popeye deformity<ref name="p5" /> | |||
{{#ev:youtube|h_DhU9H2uBw|200}} | {{#ev:youtube|h_DhU9H2uBw|200}} | ||
== Diagnostic procedures == | == Diagnostic procedures == | ||
| Line 65: | Line 53: | ||
*Assessment of the shoulder and arm contour:<ref name="p2" /> | *Assessment of the shoulder and arm contour:<ref name="p2" /> | ||
**(+) Popeye sign | **(+) Popeye sign | ||
**Descent of the [[Biceps | **Descent of the [[Biceps Brachii|biceps]] muscle in the middle part of the arm (more obvious with contraction)<ref name="p3" /> | ||
*Muscle power: Shoulder and elbow<ref name="p3" /> | *Muscle power: Shoulder and elbow<ref name="p3" /> | ||
*Range of motion: Shoulder and elbow<ref name="p2" /> | *Range of motion (ROM): Shoulder and elbow<ref name="p2" /> | ||
*Special tests:<ref name="p2" /> | *Special tests:<ref name="p2" /> | ||
** [[Yergasons Test|Yergason's test]] : Positive if pain is reproduced in the bicipital groove during the test | **[[Yergasons Test|Yergason's test]] : Positive if pain is reproduced in the bicipital groove during the test | ||
** [[Speeds Test|Speeds test]] | |||
* [[Speeds Test|Speeds test]] | ** [https://www.physio-pedia.com/Elbow_Hook_Test?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal#share Hook test] | ||
<div class="row"><div class="col-md-4"> {{#ev:youtube|7fcDs0H3-xo|250}}Hook test | |||
</div> | |||
{{#ev:youtube| | </div> | ||
== Special investigations == | |||
* [[MRI Scans|MRI]]: | * [[MRI Scans|MRI]]: | ||
** Axial and parasagittal planes needed<ref name="p6">Zanetti M, Weishaupt D, Gerber C, Hodler J. [https://www.researchgate.net/profile/Christian_Gerber/publication/13675460_Tendinopathy_and_rupture_of_the_tendon_of_the_long_head_of_the_biceps_brachii_muscle_Evaluation_with_MR_arthrography/links/0912f50c0ae536492a000000.pdf Tendinopathy and rupture of the tendon of the long head of the biceps brachii muscle: evaluation with MR arthrography.] American journal of roentgenology 1998;170(6):1557-61.</ref> | ** Axial and parasagittal planes needed<ref name="p6">Zanetti M, Weishaupt D, Gerber C, Hodler J. [https://www.researchgate.net/profile/Christian_Gerber/publication/13675460_Tendinopathy_and_rupture_of_the_tendon_of_the_long_head_of_the_biceps_brachii_muscle_Evaluation_with_MR_arthrography/links/0912f50c0ae536492a000000.pdf Tendinopathy and rupture of the tendon of the long head of the biceps brachii muscle: evaluation with MR arthrography.] American journal of roentgenology 1998;170(6):1557-61.</ref> | ||
* [[Ultrasound Scans|Ultrasound]] | * [[Ultrasound Scans|Ultrasound]] | ||
<ref name="p1" /> | <ref name="p1">Gumina S, Carbone S, Perugia D, Perugia L, Postacchini F. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3080507/ Rupture of the long head biceps tendon treated with tenodesis to the coracoid process. Results at more than 30 years]. International orthopaedics 2011;35(5):713-6.</ref> | ||
== Outcome measures == | == Outcome measures == | ||
| Line 85: | Line 74: | ||
* [[Constant-Murley Shoulder Outcome Score|Constant-Murley score]]<ref name="p3" /><ref name="p4" /> | * [[Constant-Murley Shoulder Outcome Score|Constant-Murley score]]<ref name="p3" /><ref name="p4" /> | ||
== | == Conservative Management == | ||
Anti-inflammatory medications can be used to reduce the underlying inflammatory process that may predispose tendons to rupture. When tendons are stressed or partially disrupted, anti-inflammatory medications can be used as analgesia.<ref name="p6" /> | Anti-inflammatory medications can be used to reduce the underlying inflammatory process that may predispose tendons to rupture. When tendons are stressed or partially disrupted, anti-inflammatory medications can be used as analgesia.<ref name="p6" /> | ||
Non-operative management is considered appropriate for older patients or patients who do not require a high level of supination strength.<ref name="p5" /> This is also considered for subacute or chronic biceps tendon tears.<ref name="p9">Pugach S, Pugach IZ. [https://mdedge-files-live.s3.us-east-2.amazonaws.com/files/s3fs-public/Document/September-2017/6203JFP_Article3.pdf When is a conservative approach best for proximal biceps tendon rupture?] Journal of Family Practice 2013;62(3):134-7.</ref> | |||
Non-operative management is considered appropriate for older patients or patients who do not require a high level of supination strength.<ref name="p5" /> | |||
== | == Conservative management: Physiotherapy == | ||
Conservative management of long head of biceps rupture take 4-6 weeks on average. The treatment takes 4-6 weeks, 2-3 times in a week. | |||
Treatment consists of: | |||
# Mobilization and flexibility exercises to improve the shoulder ROM. Followed by strength and stretching exercises. The muscle will also be static trained. | |||
# At home there will be home exercises. The exercises are extension and flexion and supination and pronation exercises. | |||
When rehabilitaing the BBLH remenber beyond 30°, the BBLH, even though contracting, does not create a noteworthy elevation moment and it cannot serve as a dynamic shoulder stabilizer in higher ranges of elevation. | |||
* Exercises planned to rehabilitate the shoulder. should involve low level elevation, which can increase the BBLH dynamic role in stabilizing the joint when elevated to 30° or less. | |||
== | * Incorporating eccentric contractions through the lower range of elevation would be appropriate since this could mimic the deceleration phase of the overhead throwing motion<span class="reference" id="cite_ref-:2_6-2"></span><ref>Landin D, Thompson M, Jackson MR. Actions of the biceps brachii at the shoulder: a review. Journal of clinical medicine research. 2017 Aug;9(8):667.Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5505302/<nowiki/>(accessed 10.1.2022)</ref>. | ||
Most people go back to work after 2-3 weeks but the work is adapted. After 8 weeks the ROM and the strength is back to normal. Normally there aren’t anymore restrictions more but the popeye malformation remains. <ref name="p9" /> | |||
==== Phase 1: Acute phase ==== | |||
'''Week 1''' | |||
*Clinical modalities as needed | |||
*Glenohumeral ROM: | |||
**Joint mobilization to restrict capsular tissue | |||
**Stretching as indicated | |||
**Home exercise programme: | |||
***ross-arm stretch | |||
***Sleeper stretch | |||
***Early scapular strengthening | |||
*Scapular stabilization with instruction in lower [[trapezius]] facilitation | |||
'' | ====Phase 2: Subacute phase, early strengthening==== | ||
'''Week 2''' | |||
*Continue with modalities and ROM. | |||
*Begin [[Rotator Cuff|rotator cuff]] strengthening with theraband: | |||
**Internal/external rotation in 30° abduction | |||
**Low rows (prone, scapular plane abduction (<90°), ceilling punch, biceps and triceps)<br> | |||
''' | ====Phase 3: Advanced strengthening==== | ||
'''Week 3''' | |||
*Continue with strengthening: | |||
**Resisted PNF patterns | |||
**Theraband exercises: | |||
***Bear hug | |||
***Reverse fly | |||
***Internal/external roation at 90° abduction for neuromuscular re-education | |||
**Push-up progression | |||
**Begin with plyometric exercises with both arms, progressing to one arm | |||
**Weight training | |||
* | ====Phase 4: Return to activities==== | ||
'''Week 4''' | |||
*Continue with program | |||
*Re-evaluation with physician and therapist | |||
*Advance to return-to-sport program, as motion and strength allow<ref name="p5" /> | |||
== Surgery == | |||
Non-surgical treatment is usually sufficient for proximal tendon rupture as it is more common in elderly patients. However, residual cosmetic deformity and some intermittent biceps muscle cramping may persist. Younger patients and female patients who are unwilling to accept cosmetic deformity and athletic patients with frequent cramping may opt for surgical intervention in the form of biceps tenodesis. The presence of associated rotator cuff pathology can also influence surgical management. Subpectoral tenodesis is the preferred approach for biceps tenodesis, where the tendon is attached to the bone in the bicipital groove. Sometimes this procedure is done concurrently with arthroscopic rotator cuff pathology treatment. Newer implants like interference screws and bio-absorbable suture anchors can be placed either through the open or arthroscopic approach to secure the tendon in the subpectoral space. All the approaches mentioned above are reported to achieve good clinical outcomes. However, there is limited data to show the superiority of the surgical intervention to the non-surgical approach<ref name=":1" /> | |||
== Post-operative rehabilitation: Physiotherapy management == | |||
Patients have to wear a mastersling for the first 10-14 days after surgery. Only passive range of motion is allowed in that time. Light exercises is done from week 2 to 6, where after it is progressed to functional exercises between week 6 and 8, and progressed to resistance. After this, moderate loading may be tolerated but heavy loading is prohibited for the first few months.<ref name="p7" /> | |||
<u> | ==== Phase 1: Passive (Week 0-2) ==== | ||
<u></u> | |||
*Warm up with pendulum exercises | |||
*Passive ROM | |||
*Full passive elbow flexion/extension ROM | |||
*Full passive forearm supination/pronation ROM | |||
*Full passive shoulder ROM | |||
*Seated scapular retractions<ref name=":0">Krupp RJ, Kevern MA, Gaines MD, Kotara S, Singleton SB. [https://www.jospt.org/doi/pdfplus/10.2519/jospt.2009.2802 Long head of the biceps tendon pain: differential diagnosis and treatment.] Journal of orthopaedic & sports physical therapy 2009;39(2):55-70.</ref> | |||
==== Phase 2: Active (Week 2-6) ==== | |||
* Warm up with pendulum exercises | |||
* Active ROM, with terminal stretch to prescribed limits | |||
* Full active shoulder ROM, lawn chair progression | |||
*Full active elbow flexion/extension ROM | |||
* | *Full active forearm supination/pronation ROM | ||
* | |||
==== Phase 3: Resisted (Week 6-8) ==== | |||
* Warm up with pendulum exercises | |||
* | * Theraband exercises: | ||
**Shoulder internal/external rotation at 30° abduction | |||
**Standing forward punch | |||
**Low rows | |||
* | **Bear hugs | ||
*Prone I,T,Y,W. | |||
* | |||
* | |||
* | |||
* | |||
* | |||
* | |||
*Biceps curls | *Biceps curls | ||
*Resisted supination/pronation | *Resisted supination/pronation | ||
==== Phase 4: Weight training (Week 8+) ==== | |||
*Keep hands within eyesight, keep elbows bent, minimize overhead activities | *Keep hands within eyesight, keep elbows bent, minimize overhead activities | ||
*Return to activities | *Return to normal activities: | ||
**Computer work after 1-2 weeks | |||
**Golf after 4 weeks | |||
**Tennis after 8 weeks<ref name=":0" /><ref name="p5" /> | |||
== Resources == | == Resources == | ||
* [https://www.moveforwardpt.com/SymptomsConditionsDetail.aspx?cid=a97cf498-c31a-4f0d-b4c2-3f5bdbcebba2 Physical Therapist's Guide to Biceps Tendon Rupture] | |||
* [https://www.healio.com/orthopedics/arthroscopy/news/print/orthopedics-today/%7B95443cbd-bc23-4f6a-adfb-0f4df8a0330b%7D/surgical-technique-arthroscopic-and-subpectoral-long-head-of-biceps-tenodesis Biceps tendon repair surgery] | |||
== Clinical Bottom Line == | == Clinical Bottom Line == | ||
Long head of biceps ruptures commonly occur in the population between 40 and 60 with predisposing shoulder problems. It can also occur in the younger, active population. It is characterized by a Popeye sign at the biceps. Conservative management consisting of analgesia and physiotherapy is the treatment of choice for the older population, and for patients that does not need full supination strength, as an up to 20% loss with biceps ruptures are normally present. Surgery consisting of a tenotomy and re-attachment of the tendon are mostly reserved for the younger, more active population; patients who cannot aesthetically accept the Popeye appearance; as well as patients needing full supination strength (mostly for manual labour). Physiotherapy plays a massive role in both the conservative, as well as post-surgical management of a long head of biceps rupture. | |||
== References == | == References == | ||
| Line 211: | Line 181: | ||
[[Category:Sports Medicine]] | [[Category:Sports Medicine]] | ||
[[Category:Occupational Health]] | [[Category:Occupational Health]] | ||
[[Category:Elbow]] | |||
[[Category:Shoulder]] | |||
[[Category:Conditions]] | |||
[[Category:Elbow - Conditions]] | |||
[[Category:Shoulder - Conditions]] | |||
Latest revision as of 14:54, 10 January 2022
Original Editor - Cynthia Meert
Top Contributors - Bianca Geeroms, Leana Louw, Cynthia Meert, Admin, Rachael Lowe, Kim Jackson, Lucinda hampton, Anas Mohamed, WikiSysop, Naomi O'Reilly, Linde Van Droogenbroeck, Claire Knott, Amrita Patro, Wanda van Niekerk and 127.0.0.1
Introduction[edit | edit source]
The biceps brachii muscle has two heads, one originating from the coracoid process (short head) and the other from the supraglenoid tubercle of the scapula and superior labrum (long head biceps). The long head (LHB) contributes to the stability of the glenohumeral joint. The majority of biceps rupture involves the LH. Rupture of the LHB tendon can be treated conservatively. Patients generally recover successfully if they receive a timely diagnosis and treatment
Chronic LHB rupture is defined as a tendon tear for more than 4 weeks. Chronic rupture may be due to missed diagnosis or failure of conservative treatment. MRI helps differentiate partial and complete tears of the biceps tendon[1].
Pathophysiology[edit | edit source]
The LH originates at the supraglenoid tubercle and is attached to the dorsal aspect of the radial tuburosity.[2] It runs intra-articularly over the humeral head and follows the bicipital groove distal to the glenohumeral joint.[3] It functions as dynamic stabilizer of the glenohumeral joint, as well as a depressor of the humeral head.[4]
- Age, overuse, smoking, and corticosteroid use contribute to tendon degeneration and, later, tendinopathy.
- The proximal tendon rupture in most cases occurs at the tendon-labral junction or the bony attachment[1].
Image 2: Coronal section of the tendon of long head of biceps.
Epidemiology[edit | edit source]
- Biceps tendon rupture mainly occurs in individuals between 40 and 60 years who already have a history of shoulder problems.
- It mostly affects the dominant arm.[4]
- A biceps tendon tear can also occur in younger individuals, but usually after a traumatic fall on an outstretched arm, heavy weightlifting or consistently sport activities such as snowboarding and soccer.[5][6]
Etiology[edit | edit source]
- LHB rupture is generally not due to a unique mechanism of injury but is highly correlated with rotator cuff disease.
- Risk factors include age, smoking, obesity, use of corticosteroids, and overuse. Rare causes include the use of quinolones, diabetes, lupus, and chronic kidney disease.[1]
Characteristics/Clinical presentation[edit | edit source]
Patients with a long head biceps rupture report a wide variety of symptoms.[6]
Trauma:[5]
- Audible pop
- Sharp anterior shoulder pain with or without snapping sensation[6]
Associated pathologies that may lead to rupture of long head of biceps:
- Rotator cuff tears[7]
- Tendonitis[6]
- Shoulder impingement[6]
- Popeye deformity[6]
Diagnostic procedures[edit | edit source]
Physical examination[edit | edit source]
- Assessment of the shoulder and arm contour:[4]
- Muscle power: Shoulder and elbow[2]
- Range of motion (ROM): Shoulder and elbow[4]
- Special tests:[4]
- Yergason's test : Positive if pain is reproduced in the bicipital groove during the test
- Speeds test
- Hook test
Special investigations[edit | edit source]
- MRI:
- Axial and parasagittal planes needed[8]
- Ultrasound
Outcome measures[edit | edit source]
- Disabilities of the Arm, Shoulder, and Hand (DASH), Quick DASH[7]
- Constant-Murley score[2][5]
Conservative Management[edit | edit source]
Anti-inflammatory medications can be used to reduce the underlying inflammatory process that may predispose tendons to rupture. When tendons are stressed or partially disrupted, anti-inflammatory medications can be used as analgesia.[8]
Non-operative management is considered appropriate for older patients or patients who do not require a high level of supination strength.[6] This is also considered for subacute or chronic biceps tendon tears.[10]
Conservative management: Physiotherapy[edit | edit source]
Conservative management of long head of biceps rupture take 4-6 weeks on average. The treatment takes 4-6 weeks, 2-3 times in a week. Treatment consists of:
- Mobilization and flexibility exercises to improve the shoulder ROM. Followed by strength and stretching exercises. The muscle will also be static trained.
- At home there will be home exercises. The exercises are extension and flexion and supination and pronation exercises.
When rehabilitaing the BBLH remenber beyond 30°, the BBLH, even though contracting, does not create a noteworthy elevation moment and it cannot serve as a dynamic shoulder stabilizer in higher ranges of elevation.
- Exercises planned to rehabilitate the shoulder. should involve low level elevation, which can increase the BBLH dynamic role in stabilizing the joint when elevated to 30° or less.
- Incorporating eccentric contractions through the lower range of elevation would be appropriate since this could mimic the deceleration phase of the overhead throwing motion[11].
Most people go back to work after 2-3 weeks but the work is adapted. After 8 weeks the ROM and the strength is back to normal. Normally there aren’t anymore restrictions more but the popeye malformation remains. [10]
Phase 1: Acute phase[edit | edit source]
Week 1
- Clinical modalities as needed
- Glenohumeral ROM:
- Joint mobilization to restrict capsular tissue
- Stretching as indicated
- Home exercise programme:
- ross-arm stretch
- Sleeper stretch
- Early scapular strengthening
- Scapular stabilization with instruction in lower trapezius facilitation
Phase 2: Subacute phase, early strengthening[edit | edit source]
Week 2
- Continue with modalities and ROM.
- Begin rotator cuff strengthening with theraband:
- Internal/external rotation in 30° abduction
- Low rows (prone, scapular plane abduction (<90°), ceilling punch, biceps and triceps)
Phase 3: Advanced strengthening[edit | edit source]
Week 3
- Continue with strengthening:
- Resisted PNF patterns
- Theraband exercises:
- Bear hug
- Reverse fly
- Internal/external roation at 90° abduction for neuromuscular re-education
- Push-up progression
- Begin with plyometric exercises with both arms, progressing to one arm
- Weight training
Phase 4: Return to activities[edit | edit source]
Week 4
- Continue with program
- Re-evaluation with physician and therapist
- Advance to return-to-sport program, as motion and strength allow[6]
Surgery[edit | edit source]
Non-surgical treatment is usually sufficient for proximal tendon rupture as it is more common in elderly patients. However, residual cosmetic deformity and some intermittent biceps muscle cramping may persist. Younger patients and female patients who are unwilling to accept cosmetic deformity and athletic patients with frequent cramping may opt for surgical intervention in the form of biceps tenodesis. The presence of associated rotator cuff pathology can also influence surgical management. Subpectoral tenodesis is the preferred approach for biceps tenodesis, where the tendon is attached to the bone in the bicipital groove. Sometimes this procedure is done concurrently with arthroscopic rotator cuff pathology treatment. Newer implants like interference screws and bio-absorbable suture anchors can be placed either through the open or arthroscopic approach to secure the tendon in the subpectoral space. All the approaches mentioned above are reported to achieve good clinical outcomes. However, there is limited data to show the superiority of the surgical intervention to the non-surgical approach[1]
Post-operative rehabilitation: Physiotherapy management[edit | edit source]
Patients have to wear a mastersling for the first 10-14 days after surgery. Only passive range of motion is allowed in that time. Light exercises is done from week 2 to 6, where after it is progressed to functional exercises between week 6 and 8, and progressed to resistance. After this, moderate loading may be tolerated but heavy loading is prohibited for the first few months.[7]
Phase 1: Passive (Week 0-2)[edit | edit source]
- Warm up with pendulum exercises
- Passive ROM
- Full passive elbow flexion/extension ROM
- Full passive forearm supination/pronation ROM
- Full passive shoulder ROM
- Seated scapular retractions[12]
Phase 2: Active (Week 2-6)[edit | edit source]
- Warm up with pendulum exercises
- Active ROM, with terminal stretch to prescribed limits
- Full active shoulder ROM, lawn chair progression
- Full active elbow flexion/extension ROM
- Full active forearm supination/pronation ROM
Phase 3: Resisted (Week 6-8)[edit | edit source]
- Warm up with pendulum exercises
- Theraband exercises:
- Shoulder internal/external rotation at 30° abduction
- Standing forward punch
- Low rows
- Bear hugs
- Prone I,T,Y,W.
- Biceps curls
- Resisted supination/pronation
Phase 4: Weight training (Week 8+)[edit | edit source]
- Keep hands within eyesight, keep elbows bent, minimize overhead activities
- Return to normal activities:
Resources[edit | edit source]
Clinical Bottom Line[edit | edit source]
Long head of biceps ruptures commonly occur in the population between 40 and 60 with predisposing shoulder problems. It can also occur in the younger, active population. It is characterized by a Popeye sign at the biceps. Conservative management consisting of analgesia and physiotherapy is the treatment of choice for the older population, and for patients that does not need full supination strength, as an up to 20% loss with biceps ruptures are normally present. Surgery consisting of a tenotomy and re-attachment of the tendon are mostly reserved for the younger, more active population; patients who cannot aesthetically accept the Popeye appearance; as well as patients needing full supination strength (mostly for manual labour). Physiotherapy plays a massive role in both the conservative, as well as post-surgical management of a long head of biceps rupture.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Hsu D, Anand P, Chang KV. Biceps tendon rupture. StatPearls [Internet]. 2020 Apr 20.Available:https://www.ncbi.nlm.nih.gov/books/NBK513235/?report=printable (accessed 30.9.2021)
- ↑ 2.0 2.1 2.2 2.3 Shunke M, Schulte E, Schumacher U. Anatomische atlas Prometheus: Algemene anatomie en bewegingsapparaat. Bohn Stafleu Van Loghum: Nederland, 2005.
- ↑ Elser F, Braun S, Dewing CB, Giphart JE, Millett PJ. Anatomy, function, injuries, and treatment of the long head of the biceps brachii tendon. Arthroscopy: The Journal of Arthroscopic & Related Surgery 2011;27(4):581-92.
- ↑ 4.0 4.1 4.2 4.3 4.4 Warner JJ, McMahon PJ. The role of the long head of the biceps brachii in superior stability of the glenohumeral joint. JBJS 1995;77(3):366-72.
- ↑ 5.0 5.1 5.2 Quach T, Jazayeri R, Sherman OH, Rosen JE. Distal Biceps Tendon Injuries. Bulletin of the NYU hospital for joint diseases 2010;68(2).
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 Medscape. Biceps rupture. Available from: https://emedicine.medscape.com/article/327119-overview (accessed 06/01/2019).
- ↑ 7.0 7.1 7.2 Chen CH, Chen CH, Chang CH, Su CI, Wang KC, Wang IC, Liu HT, Yu CM, Hsu KY. Classification and analysis of pathology of the long head of the biceps tendon in complete rotator cuff tears. Chang Gung Med J 2012;35(3):263-70.
- ↑ 8.0 8.1 Zanetti M, Weishaupt D, Gerber C, Hodler J. Tendinopathy and rupture of the tendon of the long head of the biceps brachii muscle: evaluation with MR arthrography. American journal of roentgenology 1998;170(6):1557-61.
- ↑ Gumina S, Carbone S, Perugia D, Perugia L, Postacchini F. Rupture of the long head biceps tendon treated with tenodesis to the coracoid process. Results at more than 30 years. International orthopaedics 2011;35(5):713-6.
- ↑ 10.0 10.1 Pugach S, Pugach IZ. When is a conservative approach best for proximal biceps tendon rupture? Journal of Family Practice 2013;62(3):134-7.
- ↑ Landin D, Thompson M, Jackson MR. Actions of the biceps brachii at the shoulder: a review. Journal of clinical medicine research. 2017 Aug;9(8):667.Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5505302/(accessed 10.1.2022)
- ↑ 12.0 12.1 Krupp RJ, Kevern MA, Gaines MD, Kotara S, Singleton SB. Long head of the biceps tendon pain: differential diagnosis and treatment. Journal of orthopaedic & sports physical therapy 2009;39(2):55-70.