Rupture Long Head Biceps: Difference between revisions
Leana Louw (talk | contribs) No edit summary |
Leana Louw (talk | contribs) No edit summary |
||
| Line 51: | Line 51: | ||
** Tendonitis<ref name="p5" /> | ** Tendonitis<ref name="p5" /> | ||
** Shoulder impingement<ref name="p5" /> | ** Shoulder impingement<ref name="p5" /> | ||
* Popeye deformity | * Popeye deformity<ref name="p5" /> | ||
{{#ev:youtube|h_DhU9H2uBw|200}} | {{#ev:youtube|h_DhU9H2uBw|200}} | ||
== Differential diagnosis == | == Differential diagnosis == | ||
* [[Acromioclavicular Joint Disorders|Acromioclavicular joint separations]] | * [[Acromioclavicular Joint Disorders|Acromioclavicular joint separations]] | ||
* [[Gout]] | * [[Gout]] | ||
* Rotator cuff disease | * Rotator cuff disease | ||
* [[Septic (Infectious) Arthritis|Septic arthritis]]<ref name="p5" / | * [[Septic (Infectious) Arthritis|Septic arthritis]] | ||
<ref name="p5" /> | |||
== Diagnostic procedures == | == Diagnostic procedures == | ||
Revision as of 21:14, 14 January 2019
Original Editor - Cynthia Meert
Top Contributors - Bianca Geeroms, Leana Louw, Cynthia Meert, Admin, Lucinda hampton, Rachael Lowe, Kim Jackson, Anas Mohamed, WikiSysop, 127.0.0.1, Naomi O'Reilly, Linde Van Droogenbroeck, Claire Knott, Amrita Patro and Wanda van Niekerk
This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! (18 May 2024)
Definition/Description[edit | edit source]
A biceps tendon rupture often occur after a sudden contraction of the biceps with resistance to flexion of the elbow and supination of the forearm. This can further be aggravated by the intrinsic degeneration of the tendon release and frictional wear of the tendon belly. This intrinsic degeneration is caused by improper training or fatigue. Inordinate stresses can be placed on the biceps as it attempts to compensate for other muscles. This can lead to attrition and failure, either within the tendon substance or at its origin.[1]
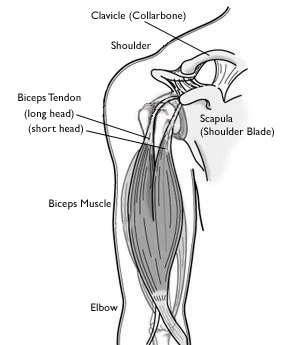
Clinically relevant anatomy[edit | edit source]
The biceps brachii muscle consists of 2 parts: The long head and the short head. The long head originates at the supraglenoid tubercle and is attached to the dorsal aspect of the radial tuburosity.[2] It runs intra-articularly over the humeral head and follows the bicipital groove distal to the glenohumeral joint.[3] It functions as dynamic stabilizer of the glenohumeral joint, as well as a depressor of the humeral head.[4] The short head is a functions more in elbow flexor, while the long head functions more in forearm supination.[5]
The parts of the tendon differ in shape. The intra-articular part is wide and flat while the extra-articular part is rounder and smaller.[3] The articular portion of the long head of biceps is vascularly supplied by the anterior circumflex artery, mostly to the proximal tendon.[3] The distal portion is fibrocartilaginous and avascular.[3] Soft-tissue stabilizes the extra-articular long head of biceps when it enters the bicipital groove en this is built by fibers of the coracohumeral ligament, superior glenohumeral ligament and parts of the subscapularis tendon.[3]
Epidemiology/Etiology[edit | edit source]
Epidemiology[edit | edit source]
Biceps tendon rupture mainly occurs in individuals between 40 and 60 years who already have a history of shoulder problems. It mostly affects the dominant arm.[4] A biceps tendon tear can also occur in younger individuals, but usually after a traumatic fall on an outstretched arm, heavy weightlifting or consistently sport activities such as snowboarding and soccer.[5][6]
Etiology[edit | edit source]
Tendon rupture usually results from sudden contraction of the biceps associated with resisted elbow flexion and supination of the forearm. A possible predisposing role is played by intrinsic degeneration of the tendon tissue or frictional wear of the tendon belly.[1]
Risk factors[edit | edit source]
- Age: Older people have put more years of wear and tear on their tendons than younger people.[1]
- Heavy overhead activities[1]
- Shoulder overuse - repetitive strain injuries:[1][7]
- Can lead to additional shoulder injuries, including tendonitis, shoulder impingement, and rotator cuff injuries
- Having any of these conditions puts more stress on the biceps tendon, making it more likely to weaken or tear
- Smoking: Nicotine use can affect nutrition in the tendon[1]
- Corticosteroids: Linked to increased muscle and tendon weakness[1]
- Gender: More common in men (most likely primarily from vocational or avocational factors)[4]
Characteristics/Clinical presentation[edit | edit source]
Patients with a long head biceps rupture report a wide variety of symptoms.[6]
- Trauma:[5]
- Audible pop
- Sharp anterior shoulder pain with or without snapping sensation[6]
- Pain:[6]
- With overhead activities
- Anterior shoulder pain that may get worse at night[6]
- Associated pathologies that may lead to rupture of long head of biceps:
- Rotator cuff tears[8]
- Tendonitis[6]
- Shoulder impingement[6]
- Popeye deformity[6]
Differential diagnosis[edit | edit source]
- Acromioclavicular joint separations
- Gout
- Rotator cuff disease
- Septic arthritis
Diagnostic procedures[edit | edit source]
Physical examination[edit | edit source]
- Special tests:
- Yergason's test : Positive if pain is reproduced in the bicipital groove during the test [4]
- Hook test
Special investigations[edit | edit source]
These studies can create a good image of soft tissues like the biceps tendon. [1]
Outcome measures[edit | edit source]
Examination[edit | edit source]
Diagnosis can be based on clinical examination (grades of recommendation:B) , based on:
- Inspection of the shoulder and arm contour and compare with the contralateral side [4]
- the presence of the classic Popeye sign or a less striking descent of the biceps muscle in the middle part of the arm. (more obvious by contracting the muscle ) [2]
- MRI findings in two planes, axial and parasagittal, is required to diagnose accurate a rupture of the biceps tendon.[9]
- Constant score: [2]
- assesses pain, function, ROM, and strength.[5]
- Pain is allotted a maximum of 15 points, activities of daily living (function) 20 points, ROM 40 points, and strength 25 points. The component scores are summated to achieve a maximum possible total score of 100. A maximum score indicates greater shoulder function.[5]
- Shoulder strength [2] (measured with a MicroFET dynamometer)
- Flexion strength of the forearm[2](measured with a MicroFET dynamometer)
- with the forearm flexed at 90° and the arm adducted to the body, with the hand in full supination
- Perform range-of-motion (ROM) testing of the shoulder and elbow. [4]
- yergason’s test [4]
- speed test [4]
Medical management[edit | edit source]
There is no consensus about surgical repair.
- Generally they do surgery for young, athletic patients or patients who needs maximum supination strength. -> Patients lose up to 20% of supination strength but there is rarely impact on ADL.
- Non-operative management is considered appropriate for older patients or patients who do not require a high level of supination strength. [6]
There are anti-inflammatory medications that can be used to reduce the underlying inflammatory process that may predispose tendons to rupture. When tendons may be stressed or partially disrupted, anti-inflammatory medications can provide an analgesic effect.(Grades of recommendation = F) [9]
Physiotherapy management[edit | edit source]
- without surgery: - we can do mobilizations - control swelling by cold modalities such as cold packs, ice massage - against inflammation: NSAIDs except for contraindications - Preserving ROM:
- Codman pendulum exercises
- Functional exercises
- After surgery: - 10 - 14d: soft sling + light exercises for ROM - 14d - 6 to 8w: functional exercises using pulleys or therapy bands - after 6 à 8w: moderate loading may be tolerated but heavy loading is prohibited for the first months.[8] (LoE: 3B)
- surgery
Before the doctor decides to operate, he considered about the advantages and disadvantages. In this situation, the activities of the patiënts , the way of living and the age are important. The operation is often carried out by young people or people who have a hard work, like a carpenter, port worker,… etc. These people need a maximal supination strenght. There will also be operated when some people can’t accept the Popeye malformation. The operation trial ( tenotomy) includes the attaching torn tendon to the bone. The results of the other studies shows us that the function of the muscle fully recovers and that the strength can go back like it was before the rupture. They also see a good cosmetic result. [10] (LoE: 3B)
postoperative (tenotomy) rehabilitation [11] (LoE: 5)
phase 1: passive
- pendulums to warm-up
- passive ROM
week 1
- full passive elbow flexion/ extension
- full passive forearm supination/pronation
- full passive shoulder ROM
- seated scapular retractions
- phase 2: active
- pendulums to warm-up
- active ROM, with terminal stretch to prescribed limits
Phase 2: active
week 2
- full active shoulder ROM, lawn chair progression
- active elbow flexion/ extension
- full ROM allowed
- active forearm supination/pronation
- full ROM allowed
phase 3: resisted
- pendulums to warm-up and continue the program
week 3
- sport cord internal/ external rotation at 30° abduction
- Prone I,T,Y,W
- Sport cord standing forward punch
- Sport cord low rows
- Sport cord bear hugs
- Biceps curls
- Resisted supination/pronation
Phase 4 : weight training
Week 4
- Keep hands within eyesight, keep elbows bent, minimize overhead activities
- Return to activities
- Computer after 1-2 weeks
- Golf after 4 weeks
- Tennis after 8 weeks [6] [11] (LoE: 5)
2. conservative treatment
Is more used in older patients and who do not need maximal supination strength in their daily life and work. There are some advantages in comparison with the first treatment. Therefore, this treatment is better tolerated and presents fewer complications. The costs are also lower and because there was no operation, the people can get back to work quicker. But with this choice of treatment the strength is 20% lower then before. But it hasn’t have influence at the ADL activities and that maybe is the reason why people hold off an operation. Also doctors recommend this treatment faster when people are afraid or when the injury is too old.
The treatment takes 4-6 weeks 2-3 times in a week. It consists of mobilization and flexibility exercises to improve the shoulder ROM. After that, there are also strength and stretching exercises. The muscle will also be static trained. At home there will be home exercises. The exercises are extension and flexion and supination en pronation exercises. After a period the pain needs to be lower and the strength have to be better. Most people go back to work after 2-3 weeks but the work is adapted. After 8 weeks the ROM and the strength is back to normal. Normally there aren’t anymore restrictions more but the popeye malformation remains. [10] (LoE: 3B)
Nonoperative rehalitation
Phase1: acute phase
Week 1
- Clinical modalities as needed
- Glenohumeral ROM
- apply appropriate joint mobilization to restrictive capsular tissues
- implement wand stretching as indicated
- supplement with home program
- cross-arm stretch
- sleeper stretch
- Early scapular strengthening
- begin scapular stabilization with instruction in lower trapezius facilitation
phase 2: subacute phase, early strengthening
Week 2
- Continue with modalities and ROM.
- Begin rotator cuff strengthening
- sport cord internal/external rotation in 30° abductee
- sport cord low rows ( prone, scapular plane abduction (<90°), celling punch, biceps en triceps)
phase 3: advanced strengthening
Week 3
- continue with strengthening
- resisted PNF patterns
- sport cord bear hug
- sport cord reverse fly
- sport cord IR/ ER at 90° abduction for neuromuscular re- education
- push-up progression
- begin 2- arm plyometric exercises advancing to 1-arm exercises
- weight training
phase 4: return to activities
week 4
- continue with program
- re-evaluation with physician and therapist
- advance to return-to-sport program, as motion and strength allow [6] (LoE: 5)
Resources[edit | edit source]
add appropriate resources here
Clinical Bottom Line[edit | edit source]
add text here
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Gumina S, Carbone S, Perugia D, Perugia L, Postacchini F. Rupture of the long head biceps tendon treated with tenodesis to the coracoid process. Results at more than 30 years. International orthopaedics 2011;35(5):713-6.
- ↑ 2.0 2.1 2.2 2.3 2.4 Shunke M, Schulte E, Schumacher U. Anatomische atlas Prometheus: Algemene anatomie en bewegingsapparaat. Bohn Stafleu Van Loghum: Nederland, 2005.
- ↑ 3.0 3.1 3.2 3.3 3.4 Elser F, Braun S, Dewing CB, Giphart JE, Millett PJ. Anatomy, function, injuries, and treatment of the long head of the biceps brachii tendon. Arthroscopy: The Journal of Arthroscopic & Related Surgery 2011;27(4):581-92.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 Warner JJ, McMahon PJ. The role of the long head of the biceps brachii in superior stability of the glenohumeral joint. JBJS 1995;77(3):366-72.
- ↑ 5.0 5.1 5.2 5.3 5.4 Quach T, Jazayeri R, Sherman OH, Rosen JE. Distal Biceps Tendon Injuries. Bulletin of the NYU hospital for joint diseases 2010;68(2).
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 6.11 Medscape. Biceps rupture. Available from: https://emedicine.medscape.com/article/327119-overview (accessed 06/01/2019).
- ↑ American Academy of Orthopaedic Surgeons. Biceps tendon tear at the shoulder. Available from: https://orthoinfo.aaos.org/en/diseases--conditions/biceps-tendon-tear-at-the-shoulder/ (Accessed 07/01/2019).
- ↑ 8.0 8.1 8.2 Chen CH, Chen CH, Chang CH, Su CI, Wang KC, Wang IC, Liu HT, Yu CM, Hsu KY. Classification and analysis of pathology of the long head of the biceps tendon in complete rotator cuff tears. Chang Gung Med J 2012;35(3):263-70.
- ↑ 9.0 9.1 ZANETTI MARCO, WEISHAUPT DOMINIK, GERBER CHRISTIAN, HODLER JUERG, ‘tendinopathy and rupture of the tendon of the long head of the biceps brachii muscle: evaluation with MR arthrography, AJR, 1998, 170:1557-1561 (level of evidence = 2B)
- ↑ 10.0 10.1 When is a conservative approach best for proximal biceps tendon rupture?, Sofya Pugach, the journal of family practice, vol 62 nr 3, (level of evidence = 3B)
- ↑ 11.0 11.1 Krupp, Ryan J., et al. "Long head of the biceps tendon pain: differential diagnosis and treatment." Journal of orthopaedic & sports physical therapy 39.2 (2009): 55-70. (level of evidence: 5)