Rocky Mountain Spotted Fever: Difference between revisions
mNo edit summary |
No edit summary |
||
| (6 intermediate revisions by 4 users not shown) | |||
| Line 28: | Line 28: | ||
<ref name="2008 incidence">CDC incidence map http://www.cdc.gov/rmsf/stats/</ref><br> | <ref name="2008 incidence">CDC incidence map http://www.cdc.gov/rmsf/stats/</ref><br> | ||
[[Image:Rmsf month.jpg|500px|graph courtesy of:http://www.cdc.gov/rmsf/stats/]]<br> | [[Image:Rmsf month.jpg|500px|graph courtesy of:http://www.cdc.gov/rmsf/stats/]]<br> | ||
| Line 78: | Line 76: | ||
<br> | <br> | ||
[[Image:Rash2.jpg|400px|Typical rash seen with Rocky Mountain spotted fever]] | [[Image:Rash2.jpg|400px|Typical rash seen with Rocky Mountain spotted fever]] | ||
== Medications | == <ref>Typical rash of RMSF http://search.creativecommons.org/?q=rocky%20mountain%20spotted%20fever#</ref> Medications == | ||
Doxycycline is the standard medication prescribed when physicians are suspicious of RMSF.<ref name="CDC1" /> Adults are prescribed to take 200mg by mouth or IV two times per day.<ref name="Johnson" /> Children who weigh less than 100lbs are to take 2mg/lb by mouth and those children who weigh above 100lbs are suggested to take the same dosage as an adult, 200mg by mouth or IV, two times per day.<ref name="Johnson" /> There has been some previous cause for concern that older medications such as tetracyclines may cause staining of a child's permanent adult teeth, however, recent treatment with doxycycline has not been shown to cause staining.<ref name="CDC1" /><ref name="Minniear">Minniear T, Buckingham S. Managing Rocky Mountain spotted fever. Expert Reviews. Anti Infect. Ther.7(9),1131-1137(2009)</ref> Medical treatment should be continued for a minimum of 3 days after one's fever had decreased. Typically, medical treatment of this disease will last anywhere from 7-14 days in length.<ref name="CDC1" /><br>If an allergy to doxycycline exists or a if a women is pregnant, other medications are available as treatment.<ref name="CDC1" /> Chlorampenicol is another antibiotic that may be prescribed, however, this medication has some adverse side effects such as: aplastic anemia and grey baby syndrome.<ref name="CDC1" /> Recommended dosing for Chloramphenicol is 500mg via IV divided 2 times per day for 7 days. General antibiotics have not been found to be effective against RMSF and sulfa drugs may actually worsen the infection.<ref name="CDC1" />Tetracyclines have been found to increase hypthrombiemic effects of anticoagulants, and they have also been found to decrease the effectiveness of common oral contraceptives.<ref name="Johnson" /> | |||
Doxycycline is the standard medication prescribed when physicians are suspicious of RMSF.<ref name="CDC1" /> Adults are prescribed to take 200mg by mouth or IV two times per day.<ref name="Johnson" /> Children who weigh less than 100lbs are to take 2mg/lb by mouth and those children who weigh above 100lbs are suggested to take the same dosage as an adult, 200mg by mouth or IV, two times per day.<ref name="Johnson" /> There has been some previous cause for concern that older medications such as tetracyclines may cause staining of a child's permanent adult teeth, however, recent treatment with doxycycline has not been shown to cause staining.<ref name="CDC1" /><ref name="Minniear">Minniear T, Buckingham S. Managing Rocky Mountain spotted fever. Expert Reviews. Anti Infect. Ther.7(9),1131-1137(2009)</ref> Medical treatment should be continued for a minimum of 3 days after one's fever had decreased. Typically, medical treatment of this disease will last anywhere from 7-14 days in length.<ref name="CDC1" /><br> | |||
If an allergy to doxycycline exists or a if a women is pregnant, other medications are available as treatment.<ref name="CDC1" /> Chlorampenicol is another antibiotic that may be prescribed, however, this medication has some adverse side effects such as: aplastic anemia and grey baby syndrome.<ref name="CDC1" /> Recommended dosing for Chloramphenicol is 500mg via IV divided 2 times per day for 7 days. General antibiotics have not been found to be effective against RMSF and sulfa drugs may actually worsen the infection.<ref name="CDC1" /> | |||
Tetracyclines have been found to increase hypthrombiemic effects of anticoagulants, and they have also been found to decrease the effectiveness of common oral contraceptives.<ref name="Johnson" /> | |||
== Diagnostic Tests/Lab Tests/Lab Values == | == Diagnostic Tests/Lab Tests/Lab Values == | ||
| Line 110: | Line 93: | ||
<br> | <br> | ||
Overall, the initial diagnosis of RMSF is made based on the clinical signs and symptoms.<ref name="CDC1" /><ref name="Minniear" /><ref name="Lacz" /> Data that is gathered later via specific laboratory tests will confirm the working diagnosis of RMSF. Thus it is extremely important to begin a course of antibiotic therapy if RMSF is suspected as soon as possible. | Overall, the initial diagnosis of RMSF is made based on the clinical signs and symptoms.<ref name="CDC1" /><ref name="Minniear" /><ref name="Lacz" /> Data that is gathered later via specific laboratory tests will confirm the working diagnosis of RMSF. Thus it is extremely important to begin a course of antibiotic therapy if RMSF is suspected as soon as possible.<br> | ||
<br> | |||
The gold standard for the diagnosis of RMSF is the indirect immunofluorescence assay (IFA) with the ''R. ricettsii'' antigen.<ref name="CDC1" /> This method has a high sensitivity and specificity rated at 94%<ref name="Lacz" />. This is performed by obtaining two serum samples and then comparing the IgG and IgM antibody titers<ref name="CDC1" /><ref name="Lacz" /><ref name="Minniear" />. Ideally, the first serum test should be completed as early as possible when symptoms first set in, and the second sample be tested 2-4 weeks after the initial test.<ref name="CDC1" /> A four fold increase in these antibody titers confirms the diagnosis of RMSF.<ref name="CDC1" /><ref name="Minniear" /><ref name="Lacz" /> | The gold standard for the diagnosis of RMSF is the indirect immunofluorescence assay (IFA) with the ''R. ricettsii'' antigen.<ref name="CDC1" /> This method has a high sensitivity and specificity rated at 94%<ref name="Lacz" />. This is performed by obtaining two serum samples and then comparing the IgG and IgM antibody titers<ref name="CDC1" /><ref name="Lacz" /><ref name="Minniear" />. Ideally, the first serum test should be completed as early as possible when symptoms first set in, and the second sample be tested 2-4 weeks after the initial test.<ref name="CDC1" /> A four fold increase in these antibody titers confirms the diagnosis of RMSF.<ref name="CDC1" /><ref name="Minniear" /><ref name="Lacz" /> | ||
| Line 161: | Line 142: | ||
*Take protective measure to limit tick exposure - wear light-colored long sleeves and pants, tuck pant legs into your socks, and wear insect repellents that contain DEET | *Take protective measure to limit tick exposure - wear light-colored long sleeves and pants, tuck pant legs into your socks, and wear insect repellents that contain DEET | ||
*Frequently examine yourself if you are in suspected tick infested areas | *Frequently examine yourself if you are in suspected tick infested areas | ||
If an attached tick is found, it is important to remove it as quickly as possible. Health professionals recommend that protective gloves be worn during this process . It is best to remove the tick via tweezers as close to the skin as possible and carefully pull it out. Take precaution to not squeeze or twist the tweezers upon removal. As soon as possible, disinfect the wound area as well as your hands. It is not advised to burn ticks out or the topical application of petroleum jelly <ref name="Dantas-Torres" />. | |||
If an attached tick is found, it is important to remove it as quickly as possible. Health professionals recommend that protective gloves be worn during this process . It is best to remove the tick via tweezers as close to the skin as possible and carefully pull it out. Take precaution to not squeeze or twist the tweezers upon removal. As soon as possible, disinfect the wound area as well as your hands. It is not advised to burn ticks out or the topical application of petroleum jelly <ref name="Dantas-Torres" />. | |||
== Systemic Involvement == | == Systemic Involvement == | ||
| Line 209: | Line 185: | ||
*Cranial nerve damage | *Cranial nerve damage | ||
*Permanent blindness | *Permanent blindness | ||
*Permanent deafness | *Permanent deafness | ||
". | |||
== Physical Therapy Management == | |||
== Physical Therapy Management | |||
Rocky Mountain spotted fever is an infectious disease that a physical therapist can not diagnosis and treat. It is important for a physical therapist to recognize the signs and symptoms that are not congruent with a disorder of the musculoskeletal system so they can be referred to a physician for further examination. One important piece of subjective information a physical therapist needs to gather during the initial evaluation is if the individual has recently been out in the woods or other outdoor areas where ticks can thrive, or if they own pets that spend time outdoors as well as indoors. Pets can commonly bring the vectors of RMSF into the home.<br> | Rocky Mountain spotted fever is an infectious disease that a physical therapist can not diagnosis and treat. It is important for a physical therapist to recognize the signs and symptoms that are not congruent with a disorder of the musculoskeletal system so they can be referred to a physician for further examination. One important piece of subjective information a physical therapist needs to gather during the initial evaluation is if the individual has recently been out in the woods or other outdoor areas where ticks can thrive, or if they own pets that spend time outdoors as well as indoors. Pets can commonly bring the vectors of RMSF into the home.<br> | ||
== <span style="">Differential Diagnosis </span> | == <span style="">Differential Diagnosis </span> == | ||
*Meningoceccemia<ref name="Dantas-Torres" /><ref name="Johnson" /> | *Meningoceccemia<ref name="Dantas-Torres" /><ref name="Johnson" /> | ||
| Line 258: | Line 232: | ||
*Sylvatic flying squirrel-associated ''Rickettsia prowazekii'' infection<ref name="Johnson" /> | *Sylvatic flying squirrel-associated ''Rickettsia prowazekii'' infection<ref name="Johnson" /> | ||
== Case Reports/ Case Studies | == Case Reports/ Case Studies == | ||
#Stallings MD S. Rocky Mountain Spotted Fever and Pregnancy: A Case Report and Review of the Literature. Obstetrical and Gyneocological Surgery 2001;56;1:37-42 | #Stallings MD S. Rocky Mountain Spotted Fever and Pregnancy: A Case Report and Review of the Literature. Obstetrical and Gyneocological Surgery 2001;56;1:37-42 | ||
* | *https://www.ncbi.nlm.nih.gov/pubmed/11140862<br> | ||
#Bergeron JW, Braddon RL, Kaelin DL. Persisting impairment following Rocky Mountain Spotted Fever: a case report. Arch Phys Med Rehabilitation 1997; 78: 1277-80. | #Bergeron JW, Braddon RL, Kaelin DL. Persisting impairment following Rocky Mountain Spotted Fever: a case report. Arch Phys Med Rehabilitation 1997; 78: 1277-80. | ||
* | *https://www.ncbi.nlm.nih.gov/pubmed/9365362<br> | ||
== Resources | == Resources == | ||
Centers for Disease Control website: <br> | Centers for Disease Control website: <br>http://www.cdc.gov/rmsf/<br> | ||
Mayo Clinic website: <br> | Mayo Clinic website: <br>http://www.mayoclinic.com/health/rocky-mountain-spotted-fever/DS00600<br> | ||
Emedicine website: <br>[http://www.medicinenet.com/rocky_mountain_spotted_fever/article.htm. http://www.medicinenet.com/rocky_mountain_spotted_fever/article.htm]<br> | Emedicine website: <br>[http://www.medicinenet.com/rocky_mountain_spotted_fever/article.htm. http://www.medicinenet.com/rocky_mountain_spotted_fever/article.htm]<br> | ||
| Line 281: | Line 255: | ||
Kids Health website:<br> [http://kidshealth.org/parent/infections/skin/rocky.html kidshealth.org/parent/infections/skin/rocky.html] | Kids Health website:<br> [http://kidshealth.org/parent/infections/skin/rocky.html kidshealth.org/parent/infections/skin/rocky.html] | ||
== References == | == References == | ||
<references /><br> | <references /><br> | ||
[[Category:Medical]] [[Category: | [[Category:Medical]] | ||
[[Category:Global Health]] | |||
[[Category:Bellarmine Student Project]] | |||
[[Category:Communicable Diseases]] | |||
Latest revision as of 09:19, 5 January 2022
Original Editors - David Grinnell from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - David Grinnell, Admin, Evan Thomas, Daniele Barilla, Lucinda hampton, Nupur Smit Shah, Rishika Babburu, Elaine Lonnemann, Wendy Walker, WikiSysop and Kim Jackson
Definition/Description[edit | edit source]
Rocky Mountain Spotted Fever (RMSF) is a tick borne disease, due to an intracellular pathogen known as Rickettsia rickettsi.[1] This pathogen is carried by ticks and is transmitted to humans via a bite from an infected tick; thus it is considered and infectious disease as well as a zoonotic disease. Three known ticks in the United States carry this pathogen: the American dog tick (Dermacentor variabilis), Rocky Mountain wood tick (Dermacentor andersoni) and the brown dog tick (Rhipicephalus sanguineous). The American dog tick carries the pathogen in the western United States, and the wood tick carries the pathogen in the eastern United States.[2] This infection was first described in the Rocky Mountains in Idaho in 1896. Howard Ricketts found the causative agent in the early 1900’s. [1] This systemic infectious disease is treatable, however, if left untreated it can be fatal.
Prevalence[edit | edit source]
United States[edit | edit source]
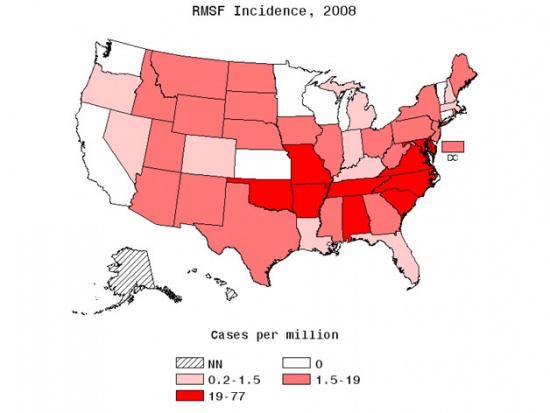
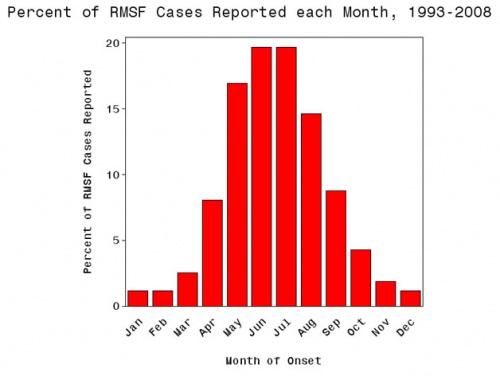
Between 1993 and 1996, there were 1253 reported cases of Rocky Mountain Spotted Fever (RMSF). This amount of confirmed incidence is roughly 2.2 cases per million. [1] Since that time period there has been some increase in confirmed cases. In 2008, the number of cases jumped to approximately 8 per million. However, the number of fatalities has decreased and currently is about 0.5%.
There is some distinction between race in the diagnosis of RMSF. Caucasians are two times more likely to be diagnosed that those of African American decent. Compared to the general population, American Indians are at the greatest risk for contracting the disease. For data that was collected between the years of 2001 and 2005, the American Indian incidence rate was calculated at 16.8 per million, while caucasians were at 4.2 per million, African Americans at 2.6 per million, and Asian/Pacific Islanders at 0.5 cases per million people.[3]
RMSF is more common in males than females; 1.7:1[3]
RMSF has varying incidence rates when age is taken into account. The aging population, specially the 60-69 year old cohort and children between the ages of 5-9 have the highest incidence rate. [3]
- 60-69 year old age group - 3.1 cases per million [3]
- 5-9 year-old age group - 3.3 cases per million [3]
Even though the disease is known as Rocky Mountain spotted fever, it is more commonly found in the eastern United States. Georgia, Maryland, North Carolina, Oklahoma, South Carolina, Tennessee, and Virginia are among the states that have confirmed the largest number of cases. [3]
Worldwide[edit | edit source]
Other cases of RMSF have been confirmed in Canada, Mexico, Central America, Columbia, as well as Brazil. Currently, there haven’t been any confirmed cases of RMSF beyond the boarders of the American continents.[3]
Characteristics/Clinical Presentation[edit | edit source]
The R. ricketttsi pathogen can have numerous systemic manifestations affecting the: cardiac, pulmonary, gastrointestinal, renal, neurological, ocular, musculoskeletal, and integumentary systems.[2] If infected the individual may face moderate to severe illness. The initial symptoms usually will begin 2-14 days after being bitten by an infected tick.[6]
Initial symptoms include [1][2][3][7]
- High fever - reaching temperatures to 102 degrees Fahrenheit (38.9 degrees Celsius) or greater
- Chills
- Severe headache
- Nausea
- Vomiting
- Fatigue
- Loss of appetite
- Abdominal pain - may present as appendicitis
- Conjunctival infection
- Muscle pain
Additional signs and symptoms that may develop include the following:
- A red-spotted rash that spreads to a majority of the body -this rash occurs in approximately 90% of those infected with RMSF and usually appears 2-5 days after the fever has been present
- Restlessness
- Diarrhea
- Aches & pains
- Delirium
After completing a thorough examination, a patient's laboratory workup may show the following results: [2]
- Normal peripheral WBC count
- Thrombocytopenia
- Elevated aminotransferase levels
- Hyponatremia
- Anemia
- Elevated bilirubin level
- Elevated level of creatine kinase
- Elevated CSF and WBC count with monocyte predominance
- Serological tests negative until convalescence
[8] Medications[edit | edit source]
Doxycycline is the standard medication prescribed when physicians are suspicious of RMSF.[7] Adults are prescribed to take 200mg by mouth or IV two times per day.[3] Children who weigh less than 100lbs are to take 2mg/lb by mouth and those children who weigh above 100lbs are suggested to take the same dosage as an adult, 200mg by mouth or IV, two times per day.[3] There has been some previous cause for concern that older medications such as tetracyclines may cause staining of a child's permanent adult teeth, however, recent treatment with doxycycline has not been shown to cause staining.[7][9] Medical treatment should be continued for a minimum of 3 days after one's fever had decreased. Typically, medical treatment of this disease will last anywhere from 7-14 days in length.[7]
If an allergy to doxycycline exists or a if a women is pregnant, other medications are available as treatment.[7] Chlorampenicol is another antibiotic that may be prescribed, however, this medication has some adverse side effects such as: aplastic anemia and grey baby syndrome.[7] Recommended dosing for Chloramphenicol is 500mg via IV divided 2 times per day for 7 days. General antibiotics have not been found to be effective against RMSF and sulfa drugs may actually worsen the infection.[7]Tetracyclines have been found to increase hypthrombiemic effects of anticoagulants, and they have also been found to decrease the effectiveness of common oral contraceptives.[3]
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
Lab tests that will be completed if RMSF is suspected included the following:[3]
- CBC count
- Electrolytes
- Renal function tests
- Liver function tests
- Coagulation panel
Overall, the initial diagnosis of RMSF is made based on the clinical signs and symptoms.[7][9][1] Data that is gathered later via specific laboratory tests will confirm the working diagnosis of RMSF. Thus it is extremely important to begin a course of antibiotic therapy if RMSF is suspected as soon as possible.
The gold standard for the diagnosis of RMSF is the indirect immunofluorescence assay (IFA) with the R. ricettsii antigen.[7] This method has a high sensitivity and specificity rated at 94%[1]. This is performed by obtaining two serum samples and then comparing the IgG and IgM antibody titers[7][1][9]. Ideally, the first serum test should be completed as early as possible when symptoms first set in, and the second sample be tested 2-4 weeks after the initial test.[7] A four fold increase in these antibody titers confirms the diagnosis of RMSF.[7][9][1]
Etiology/Causes[edit | edit source]
RMSF is a possibly fatal tick-borne illness. Three known ticks in the United States carry the pathogen R. rickettsii:the American dog tick (Dermacentor variabilis), Rocky Mountain wood tick (Dermacentor andersoni) and the brown dog tick (Rhipicephalus sanguineous). The American dog tick primarily carries the pathogen in the United States, primarily in the western United States. The Rocky Mountain wood tick primarily carries the pathogen in the eastern United States and the brown dog tick is thought to be the vector for the pathogen in Mexico. In addition, there are other tick species that are thought to carry the pathogen. In Central and South America, the Cayenne tick is thought to be the vector for the pathogen.[2]
R. rickettsiiis transmitted to humans via a bite of an infected tick. The tick bites do not cause pain, and many don't know they were exposed to the ticks. The transmission process can be completed in as little as 4 hours extending up to 24 hours. Most cases of RMSF occur between the months of April and September and usually occur in rural settings, however, they are not confined to just the rural community.[3]
R. rickettsii[2]
| Kingdom | Bacteria |
| Phylum | Proteobacterai |
| Class | Alphaproeobacteria |
| Order | Rickettsiales |
| Family | Rickettsiaceae |
| Genus | Rickettsia |
| Species | Rickettsia rickettsii |
Currently, there is no vaccine that will protect against RMSF[1] [2][3]. With precaution one can prevent the transmission of the disease by following these general recommendations:
- Avoid habitats where ticks thrive - wooded, grassy areas, stream banks and trails
- Take protective measure to limit tick exposure - wear light-colored long sleeves and pants, tuck pant legs into your socks, and wear insect repellents that contain DEET
- Frequently examine yourself if you are in suspected tick infested areas
If an attached tick is found, it is important to remove it as quickly as possible. Health professionals recommend that protective gloves be worn during this process . It is best to remove the tick via tweezers as close to the skin as possible and carefully pull it out. Take precaution to not squeeze or twist the tweezers upon removal. As soon as possible, disinfect the wound area as well as your hands. It is not advised to burn ticks out or the topical application of petroleum jelly [2].
Systemic Involvement[edit | edit source]
Rocky Mountain Spotted Fever is a systemic disease in nature. Infected individuals can presented with numerous signs and symptoms that will have an affect on the: integumentary, cardiac, pulmonary, gastrointestinal, renal, neurological, ocular, and musculoskeletal systems.[2] The Rickettsia pathogen reproduces intracellularly after being introduced through the skin via a tick bite. The pathogen is then spread by the bloodstream and the body's lymphatic system.[3]
Integumentary systemm manifestations [3]
- 1-5mm blanchable erthyemathematous macule and this will usually progress to a petechial rash
Cardiovascular system manifestations [3]
- Myocarditis
Renal system manifestations [3]
- Reduced glomerular filtration rate
- Prerenal azotemia
- Focal hepatocellular necrosis
Gastrointestinal system manifestations[3]
- Abdominal pain
- Nausea
- Vomiting
- Diarrhea
- Occult bloody stool
Pulmonary system manifestations [3]
- Noncardiogenic pulmonary edema
- Interstitial pneumonia
- Adult respiratory system distress
Neurological system manifestations [3]
- Encephalitis
- Meningoencephalitis
- Seizure
- Cranial nerve damage
- Permanent blindness
- Permanent deafness
".
Physical Therapy Management[edit | edit source]
Rocky Mountain spotted fever is an infectious disease that a physical therapist can not diagnosis and treat. It is important for a physical therapist to recognize the signs and symptoms that are not congruent with a disorder of the musculoskeletal system so they can be referred to a physician for further examination. One important piece of subjective information a physical therapist needs to gather during the initial evaluation is if the individual has recently been out in the woods or other outdoor areas where ticks can thrive, or if they own pets that spend time outdoors as well as indoors. Pets can commonly bring the vectors of RMSF into the home.
Differential Diagnosis [edit | edit source]
- Meningoceccemia[2][3]
- Enteroviral infection[2]
- Typhus[2]
- Ehrlichiosis[2]
- Immune complex vasculitis[2][3]
- Typhoid fever[2][3]
- Leptospirosis[2]
- Dengue[2]
- Infectious mononucleosis[2][3]
- Bacterial sepsis[2][3]
- Gastroenteritis[2][3]
- Bronchitis[2][3]
- Pneumonia[2][3]
- Hepatitis[3]
- Idiopathic Thrombocytopenic Purpura[3]
- Meningitis[3]
- Henoch-Schonlein Purpura[3]
- Kawasaki Disease[3]
- Measles[3]
- Rubella[3]
- Syphilis[3]
- Ehrlichiosis[3]
- Lyme's Disease[3]
- Q Fever[3]
- Relapsing Fever[3]
- Tularemia[3]
- Toxic Shock Syndrome[3]
- Influenza[3]
- Entervirus infection[3]
- Disseminated gonococcal infection[3]
- Drug hypersensivity[3]
- Staphylococcal sepsis[3]
- Murine typhus[3]
- Rickettsialpox[3]
- Recrudescent typhus[3]
- Sylvatic flying squirrel-associated Rickettsia prowazekii infection[3]
Case Reports/ Case Studies[edit | edit source]
- Stallings MD S. Rocky Mountain Spotted Fever and Pregnancy: A Case Report and Review of the Literature. Obstetrical and Gyneocological Surgery 2001;56;1:37-42
- Bergeron JW, Braddon RL, Kaelin DL. Persisting impairment following Rocky Mountain Spotted Fever: a case report. Arch Phys Med Rehabilitation 1997; 78: 1277-80.
Resources[edit | edit source]
Centers for Disease Control website:
http://www.cdc.gov/rmsf/
Mayo Clinic website:
http://www.mayoclinic.com/health/rocky-mountain-spotted-fever/DS00600
Emedicine website:
http://www.medicinenet.com/rocky_mountain_spotted_fever/article.htm
Medline plus website:
http://www.nlm.nih.gov/medlineplus/ency/article/000654.htm
WebMD website:
http://www.webmd.com/skin-problems-and-treatments/rocky-mountain-spotted-fever
Kids Health website:
kidshealth.org/parent/infections/skin/rocky.html
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Lacz NL, Schwartz RA, Kapila R. Rocky Mountain spotted fever. JEADV 2006, 20, 411-417.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 2.19 2.20 2.21 Dantas-Torres F, Rocky Mountain spotted fever. Lancet Infectious Disease 2007;7:724-732
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 3.17 3.18 3.19 3.20 3.21 3.22 3.23 3.24 3.25 3.26 3.27 3.28 3.29 3.30 3.31 3.32 3.33 3.34 3.35 3.36 3.37 3.38 3.39 3.40 3.41 3.42 3.43 3.44 3.45 3.46 3.47 3.48 3.49 3.50 3.51 Johnson CD, Sinert RH. Tick-Borne Disease, Rocky Mountain Spotted Fever, http://emedicine.medscape.com/article/785659-overview. accessed 3/17/2011
- ↑ CDC incidence map http://www.cdc.gov/rmsf/stats/
- ↑ http://www.cdc.gov/rmsf/stats/
- ↑ Pub Med Health. http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001677/. accessed 3/4/2011
- ↑ 7.00 7.01 7.02 7.03 7.04 7.05 7.06 7.07 7.08 7.09 7.10 7.11 Centers for Disease Control and Prevention: http://www.cdc.gov/rmsf/symptoms/index.html. accessed 3/17/2011
- ↑ Typical rash of RMSF http://search.creativecommons.org/?q=rocky%20mountain%20spotted%20fever#
- ↑ 9.0 9.1 9.2 9.3 Minniear T, Buckingham S. Managing Rocky Mountain spotted fever. Expert Reviews. Anti Infect. Ther.7(9),1131-1137(2009)
- ↑ photo courtsey of: http://search.creativecommons.org/?q=rocky%20mountain%20spotted%20fever#