Rhabdomyolysis Case Study: Difference between revisions
No edit summary |
No edit summary |
||
| (38 intermediate revisions by 2 users not shown) | |||
| Line 3: | Line 3: | ||
== Author/s == | == Author/s == | ||
Lindsay Matijevich, | <span style="font-size: 13.2799997329712px; line-height: 19.9200000762939px;">Kat Brock, Lindsay Matijevich, </span><span style="font-size: 13.2799997329712px; line-height: 19.9200000762939px;">Evan Scher, and </span><span style="line-height: 1.5em; font-size: 13.2799997329712px;">Katy Wiggins from </span>[http://www.physio-pedia.com/Pathophysiology_of_Complex_Patient_Problems Bellarmine University Physical Therapy Program's Pathophysiology of Complex Patient Problems Project.] | ||
<br> | |||
== Patient Characteristics == | == Patient Characteristics == | ||
Patient is a 55 year old female that reports to your clinic with complaints of low back pain and leg pain. She is teacher at a local high school | Patient is a 55 year old female that reports to your clinic with complaints of low back pain and leg pain. She is a full time teacher at a local high school. She has history of hypertension that is now controlled with diet and exercise but other comorbidities have not been found. The patient disclosed that she had the flu last week but has not been tested or had a diagnosis confirmed. She has had no other treatment prior to this therapy session. | ||
<br> | <br> | ||
| Line 17: | Line 15: | ||
== Examination == | == Examination == | ||
Patient complains of back pain that is making it difficult to sit for long periods at work. She reports bilateral tenderness over her low back and generalized weakness of the lower extremities. She states that she can't afford to miss anymore school so it's important that she get her pain resolved as quickly as possible. She says that she is still fatigued but attributes that to being sick and still not being fully recovered. She also mentions during the evaluation that she felt extremely hot and clammy. Her temperature was taken and measured 101. 3°F. When asked of any other symptoms she has noticed, she remarks that her urine has been unusually dark the past week and almost looks bloody. She also states that she has been experiencing some mild shortness of breath that has been getting worse the past couple days. Again this was attributed to being sick, dehydrated, and deconditioned.<ref>Sauret J, Marinides G, Wang G. Rhabdomyolysis. American Family Physician [serial online]. March 2002;65(5):907-907-12, 777-80, 2p passim. Available from: CINAHL, Ipswich, MA. Accessed March 25, 2015.</ref><br> | Patient complains of back pain that is making it difficult to sit for long periods at work. She reports bilateral tenderness over her low back and generalized weakness of the lower extremities. She states that she can't afford to miss anymore school so it's important that she get her pain resolved as quickly as possible. She says that she is still fatigued but attributes that to being sick and still not being fully recovered. She also mentions during the evaluation that she felt extremely hot and clammy. Her temperature was taken and measured 101. 3°F. When asked of any other symptoms she has noticed, she remarks that her urine has been unusually dark the past week and almost looks bloody. She also states that she has been experiencing some mild shortness of breath that has been getting worse the past couple days. Again this was attributed to being sick, dehydrated, and deconditioned.<ref name="AFP">Sauret J, Marinides G, Wang G. Rhabdomyolysis. American Family Physician [serial online]. March 2002;65(5):907-907-12, 777-80, 2p passim. Available from: CINAHL, Ipswich, MA. Accessed March 25, 2015.</ref><br> | ||
Patient has a history of hypertension but has been able to control it with diet and exercise and has not taken medication for her high blood pressure in 5 years. Her father also has a history of congestive heart failure and type 2 diabetes. She had her gallbladder removed 7 years ago but has had no other major surgeries. She is currently not taking any prescription medications regularly but has been taking over the counter Aleve® for her back and leg pain. | Patient has a history of hypertension but has been able to control it with diet and exercise and has not taken medication for her high blood pressure in 5 years. Her father also has a history of congestive heart failure and type 2 diabetes. She had her gallbladder removed 7 years ago but has had no other major surgeries. She is currently not taking any prescription medications regularly but has been taking over the counter Aleve® for her back and leg pain. | ||
Patient reported outcome measures were used during the evaluation in this case study. The patient completed a Visual Analog Scale (VAS), Lower Extremity Functional Scale (LEFS), and a Oswestry Disability Index (ODI). On the VAS, the patient reported that her pain was a 2/10 at best, a 6/10 at worst, and was currently at a pain level of 3/10. On the LEFS, the patient scored a 30/80 putting her at 37% of her maximum function. On the ODI, the patient scored a 33/50 putting her at 66% disability in the catergory of "crippling back pain." | Patient reported outcome measures were used during the evaluation in this case study. The patient completed a Visual Analog Scale (VAS), Lower Extremity Functional Scale (LEFS), and a Oswestry Disability Index (ODI). On the VAS, the patient reported that her pain was a 2/10 at best, a 6/10 at worst, and was currently at a pain level of 3/10. On the LEFS, the patient scored a 30/80 putting her at 37% of her maximum function.<ref name="LEFS">Lower Extremity Functional Scale. Rehabilitation Measures Database. http://www.rehabmeasures.org/default.aspx</ref> On the ODI, the patient scored a 33/50 putting her at 66% disability in the catergory of "crippling back pain."<ref name="ODI">Oswestry Disability Index. Rehabilitation Measures Database. http://www.rehabmeasures.org/default.aspx</ref> <br> | ||
<br> | |||
== | *''' [[Image:RhabdoUrine-490x500.jpg|thumb|left]]Image 1:''' <span style="font-size: 13.2799997329712px; line-height: 1.5em;">Urine from a person with rhabdomyolysis showing the characteristic brown discoloration as a result of myoglobinuria <ref>Rhabdomyolysis Wikipedia Page. http://en.wikipedia.org/wiki/Rhabdomyolysis</ref></span> | ||
== Physical Examination == | |||
'''AROM:''' | |||
UE WNL | |||
Trunk forward flexion 50% limited | |||
Trunk extension 50% limited<br> | |||
Hip flexion 80% limited | |||
All other LE WNL<br> | |||
<br> | |||
'''Palpation:''' Swollen and tender B lumbar back extensors | |||
<br> | |||
'''MMT:'''<br> | |||
UE 4+/5 | |||
Hip flexion 4-/5 | |||
Hip abd/add 4-/5 | |||
Knee extension 4/5 | |||
Knee flexion 4/5 | |||
Ankle 5/5 | |||
<br> | |||
'''Sensation:''' Normal | |||
<br> | <br> | ||
'''Reflexes:''' Normal | |||
== Clinical Impression == | |||
Our clinical impression at first glance would be that the patient is still suffering from flu like symptoms. Another possible diagnosis could be sciatica since her pain is presenting in her low back and legs. It would be critical to ask the patient to describe the type of pain that she is experiencing. Given that the patient’s pain is bilateral and she is having blood in her urine leads us to suspect that her pain is from systemic origins. A number of kidney disorders can cause blood to be present in the urine including urinary tract infections, kidney infections, kidney stones, glomerulonephritis, inherited disorders such as sickle cell anemia, or advanced stages of kidney cancer.<ref name="Mayo">Diseases and Conditions: Blood in Urine (hematuria) Causes. Mayo Clinic. http://www.mayoclinic.org/diseases-conditions/blood-in-urine/basics/causes/con-20032338</ref> Because this patient had no complaints of painful urination, flank pain, no history of cancer or inherited disorders, and no direct trauma to the kidneys lead us to suspect rhabdomyolysis caused by an infection. | |||
== Summarization of Examination Findings == | |||
With a working diagnosis of infectious rhabdomyolysis the patient would be referred out to a physician for immediate medical treatment. | |||
== Intervention == | |||
The treatment of rhabdomyolysis is primarily directed at preserving renal function. Intravenous (IV) hydration must be initiated as early as possible.<ref name="AFP" /><br> | |||
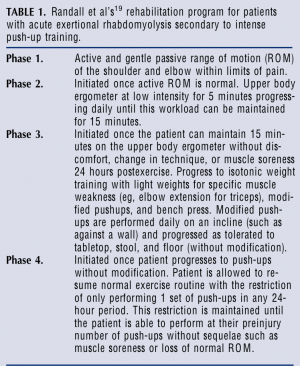
Once patients have completed initial medical management, they should undergo physical therapy rehabilitation to regain full range of motion (ROM), muscle strength, and full function before progressing back to full physical activity. There is no set protocol of how to treat a patient with rhabdomyolysis. Each treatment should be centered to fit the patient’s individual needs. Below is an example of a treatment presented in the Journal of Orthopedic and Sports Physical Therapy in 2003. This rehabilitation program was used for the diagnosis of acute exertional rhabdomyolysis (AER) secondary to intense push-up training.<ref name="Moore">Baxter R, Moore J. Diagnosis and Treatment of Acute Exertional Rhabdomyolysis. Journal of Orthopaedic and Sports Physical Therapy 2003; 33(3): 104-108</ref> Using the framework from this protocol, therapists can individualize an intervention for their patient's specific deficits. The basis behind the program is gradual progression from PROM to slowly building a tolerance for exercising the specific muscle groups affected without any symptoms after each session.<br> | |||
[[Image:Image1.PNG|thumb|right]]<br> | |||
*The patient described above would begin passive and active ROM to regain trunk mobility. Once full motion is restored painfree the therapist can begin to slowly strengthen the LE musculature and trunk stabilizers to the patient's tolerance beginning with light walking on a treadmill or recumbent bike for a short time period and increasing the duration and intensity of exercises as the patient progresses without any further reoccuring symptoms. | |||
<br> | |||
*'''Table 1''': Rehabilitation program for patients with acute exertional rhabdomyolysis secondary to intense push up training. <ref>Randall T. Butler N. Vance AM. Rehabilitation of Ten Soldiers with Exertional Rhabdomyolysis. Mil Med; 1996.</ref><br> | |||
== Outcomes == | == Outcomes == | ||
Typically patient will return to normal activities within a couple weeks to a few months after treatment depending on the severity. The earlier the patient is able to begin treatment including IV fluids or possibly dialysis to reduce the risk of kidney damage the better their prognosis. Patients that are not treated quickly may go into renal failure, but is rarely fatal. <ref>Ozawa H, Noma S, Nonaka I. [Myositis and rhabdomyolysis with influenza infection]. Nippon Rinsho. 2000;58(11):2276-81.</ref> Some patients may have residual muscle pain or fatigue that can be addressed with physical therapy intervention. <ref>Rhabdomyolysis: MedlinePlus Medical Encyclopedia. http://www.nlm.nih.gov/medlineplus/ency/article/000473.htm Last updated March 15, 2015. Accessed March 29, 2015.</ref> For the case described above physical therapy can be beneficial for the patient if she continues to have lingering back and leg pain after her initial treatment. The protocol listed above was designed for exertional rhabdomyolysis of the shoulders, but the core concepts can be redesigned to fit other patients with residual muscle pain. (5) A gradual approach will be beneficial to patients that present with muscle pain after an episode of rhabdomyolysis as to return their body's to the demands of normal activities without risking another breakdown of muscles. | |||
== Discussion == | == Discussion == | ||
Physical therapists are likely to be one of the first healthcare professionals to see patients that present with rhabdomyolysis as their underlying cause due to the muscular origin of their pain. Being able to identify the red flags, such as dark urine, is vital in the diagnosis and referral of the patient to get immediate treatment and therefore decreasing the risk of severe kidney damage. Patients may be hesitant to discuss changes they have noticed in their urine without the therapist specifically asking about it. Taking an accurate history from the patient can lead to asking the correct questions to determine a diagnosis. It is also important to know the etiology of the disease that may be presenting. Rhabdomyolysis has several known causes with the most common being infectious disease, such as influenza, and over exertion during exercise. If a patient comes to the clinic with muscle pain or fatigue along with complaints of a cold or high intensity exercise recently, adding in a question about the color of their urine may prove to be pertinent in making the correct diagnosis.<br> | |||
== Related Pages == | == Related Pages == | ||
<div>MedlinePlus: [http://www.nlm.nih.gov/medlineplus/ency/article/000473.htm www.nlm.nih.gov/medlineplus/ency/article/000473.htm]</div> | |||
Physiopedia: [http://www.physio-pedia.com/Rhabdomyolysis www.physio-pedia.com/Rhabdomyolysis] | |||
Infectious vs Non-infectious Rhabdo (MedScape): [http://www.medscape.com/viewarticle/433872 www.medscape.com/viewarticle/433872] | |||
A case study (1995): [http://cid.oxfordjournals.org/content/22/4/642.full.pdf cid.oxfordjournals.org/content/22/4/642.full.pdf] | |||
== References == | == References == | ||
| Line 76: | Line 109: | ||
References will automatically be added here, see [[Adding References|adding references tutorial]]. | References will automatically be added here, see [[Adding References|adding references tutorial]]. | ||
<references /> | <references /> | ||
[[Category:Case Studies]] | |||
Latest revision as of 00:31, 12 March 2018
Author/s[edit | edit source]
Kat Brock, Lindsay Matijevich, Evan Scher, and Katy Wiggins from Bellarmine University Physical Therapy Program's Pathophysiology of Complex Patient Problems Project.
Patient Characteristics[edit | edit source]
Patient is a 55 year old female that reports to your clinic with complaints of low back pain and leg pain. She is a full time teacher at a local high school. She has history of hypertension that is now controlled with diet and exercise but other comorbidities have not been found. The patient disclosed that she had the flu last week but has not been tested or had a diagnosis confirmed. She has had no other treatment prior to this therapy session.
Examination[edit | edit source]
Patient complains of back pain that is making it difficult to sit for long periods at work. She reports bilateral tenderness over her low back and generalized weakness of the lower extremities. She states that she can't afford to miss anymore school so it's important that she get her pain resolved as quickly as possible. She says that she is still fatigued but attributes that to being sick and still not being fully recovered. She also mentions during the evaluation that she felt extremely hot and clammy. Her temperature was taken and measured 101. 3°F. When asked of any other symptoms she has noticed, she remarks that her urine has been unusually dark the past week and almost looks bloody. She also states that she has been experiencing some mild shortness of breath that has been getting worse the past couple days. Again this was attributed to being sick, dehydrated, and deconditioned.[1]
Patient has a history of hypertension but has been able to control it with diet and exercise and has not taken medication for her high blood pressure in 5 years. Her father also has a history of congestive heart failure and type 2 diabetes. She had her gallbladder removed 7 years ago but has had no other major surgeries. She is currently not taking any prescription medications regularly but has been taking over the counter Aleve® for her back and leg pain.
Patient reported outcome measures were used during the evaluation in this case study. The patient completed a Visual Analog Scale (VAS), Lower Extremity Functional Scale (LEFS), and a Oswestry Disability Index (ODI). On the VAS, the patient reported that her pain was a 2/10 at best, a 6/10 at worst, and was currently at a pain level of 3/10. On the LEFS, the patient scored a 30/80 putting her at 37% of her maximum function.[2] On the ODI, the patient scored a 33/50 putting her at 66% disability in the catergory of "crippling back pain."[3]
- Image 1: Urine from a person with rhabdomyolysis showing the characteristic brown discoloration as a result of myoglobinuria [4]
Physical Examination [edit | edit source]
AROM:
UE WNL
Trunk forward flexion 50% limited
Trunk extension 50% limited
Hip flexion 80% limited
All other LE WNL
Palpation: Swollen and tender B lumbar back extensors
MMT:
UE 4+/5
Hip flexion 4-/5
Hip abd/add 4-/5
Knee extension 4/5
Knee flexion 4/5
Ankle 5/5
Sensation: Normal
Reflexes: Normal
Clinical Impression[edit | edit source]
Our clinical impression at first glance would be that the patient is still suffering from flu like symptoms. Another possible diagnosis could be sciatica since her pain is presenting in her low back and legs. It would be critical to ask the patient to describe the type of pain that she is experiencing. Given that the patient’s pain is bilateral and she is having blood in her urine leads us to suspect that her pain is from systemic origins. A number of kidney disorders can cause blood to be present in the urine including urinary tract infections, kidney infections, kidney stones, glomerulonephritis, inherited disorders such as sickle cell anemia, or advanced stages of kidney cancer.[5] Because this patient had no complaints of painful urination, flank pain, no history of cancer or inherited disorders, and no direct trauma to the kidneys lead us to suspect rhabdomyolysis caused by an infection.
Summarization of Examination Findings[edit | edit source]
With a working diagnosis of infectious rhabdomyolysis the patient would be referred out to a physician for immediate medical treatment.
Intervention[edit | edit source]
The treatment of rhabdomyolysis is primarily directed at preserving renal function. Intravenous (IV) hydration must be initiated as early as possible.[1]
Once patients have completed initial medical management, they should undergo physical therapy rehabilitation to regain full range of motion (ROM), muscle strength, and full function before progressing back to full physical activity. There is no set protocol of how to treat a patient with rhabdomyolysis. Each treatment should be centered to fit the patient’s individual needs. Below is an example of a treatment presented in the Journal of Orthopedic and Sports Physical Therapy in 2003. This rehabilitation program was used for the diagnosis of acute exertional rhabdomyolysis (AER) secondary to intense push-up training.[6] Using the framework from this protocol, therapists can individualize an intervention for their patient's specific deficits. The basis behind the program is gradual progression from PROM to slowly building a tolerance for exercising the specific muscle groups affected without any symptoms after each session.
- The patient described above would begin passive and active ROM to regain trunk mobility. Once full motion is restored painfree the therapist can begin to slowly strengthen the LE musculature and trunk stabilizers to the patient's tolerance beginning with light walking on a treadmill or recumbent bike for a short time period and increasing the duration and intensity of exercises as the patient progresses without any further reoccuring symptoms.
- Table 1: Rehabilitation program for patients with acute exertional rhabdomyolysis secondary to intense push up training. [7]
Outcomes[edit | edit source]
Typically patient will return to normal activities within a couple weeks to a few months after treatment depending on the severity. The earlier the patient is able to begin treatment including IV fluids or possibly dialysis to reduce the risk of kidney damage the better their prognosis. Patients that are not treated quickly may go into renal failure, but is rarely fatal. [8] Some patients may have residual muscle pain or fatigue that can be addressed with physical therapy intervention. [9] For the case described above physical therapy can be beneficial for the patient if she continues to have lingering back and leg pain after her initial treatment. The protocol listed above was designed for exertional rhabdomyolysis of the shoulders, but the core concepts can be redesigned to fit other patients with residual muscle pain. (5) A gradual approach will be beneficial to patients that present with muscle pain after an episode of rhabdomyolysis as to return their body's to the demands of normal activities without risking another breakdown of muscles.
Discussion[edit | edit source]
Physical therapists are likely to be one of the first healthcare professionals to see patients that present with rhabdomyolysis as their underlying cause due to the muscular origin of their pain. Being able to identify the red flags, such as dark urine, is vital in the diagnosis and referral of the patient to get immediate treatment and therefore decreasing the risk of severe kidney damage. Patients may be hesitant to discuss changes they have noticed in their urine without the therapist specifically asking about it. Taking an accurate history from the patient can lead to asking the correct questions to determine a diagnosis. It is also important to know the etiology of the disease that may be presenting. Rhabdomyolysis has several known causes with the most common being infectious disease, such as influenza, and over exertion during exercise. If a patient comes to the clinic with muscle pain or fatigue along with complaints of a cold or high intensity exercise recently, adding in a question about the color of their urine may prove to be pertinent in making the correct diagnosis.
Related Pages[edit | edit source]
Physiopedia: www.physio-pedia.com/Rhabdomyolysis
Infectious vs Non-infectious Rhabdo (MedScape): www.medscape.com/viewarticle/433872
A case study (1995): cid.oxfordjournals.org/content/22/4/642.full.pdf
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ 1.0 1.1 Sauret J, Marinides G, Wang G. Rhabdomyolysis. American Family Physician [serial online]. March 2002;65(5):907-907-12, 777-80, 2p passim. Available from: CINAHL, Ipswich, MA. Accessed March 25, 2015.
- ↑ Lower Extremity Functional Scale. Rehabilitation Measures Database. http://www.rehabmeasures.org/default.aspx
- ↑ Oswestry Disability Index. Rehabilitation Measures Database. http://www.rehabmeasures.org/default.aspx
- ↑ Rhabdomyolysis Wikipedia Page. http://en.wikipedia.org/wiki/Rhabdomyolysis
- ↑ Diseases and Conditions: Blood in Urine (hematuria) Causes. Mayo Clinic. http://www.mayoclinic.org/diseases-conditions/blood-in-urine/basics/causes/con-20032338
- ↑ Baxter R, Moore J. Diagnosis and Treatment of Acute Exertional Rhabdomyolysis. Journal of Orthopaedic and Sports Physical Therapy 2003; 33(3): 104-108
- ↑ Randall T. Butler N. Vance AM. Rehabilitation of Ten Soldiers with Exertional Rhabdomyolysis. Mil Med; 1996.
- ↑ Ozawa H, Noma S, Nonaka I. [Myositis and rhabdomyolysis with influenza infection]. Nippon Rinsho. 2000;58(11):2276-81.
- ↑ Rhabdomyolysis: MedlinePlus Medical Encyclopedia. http://www.nlm.nih.gov/medlineplus/ency/article/000473.htm Last updated March 15, 2015. Accessed March 29, 2015.