Reducing pressures on the NHS: the emerging role of the physiotherapist in healthcare reform: Difference between revisions
No edit summary |
Chee Wee Tan (talk | contribs) No edit summary |
||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor '''- Your name will be added here if you created the original content for this page. | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | |||
== Introduction == | |||
The goal of this resource is to provide a learning tool for students, recent graduates and junior physiotherapists at a time where integration of health and social care is a priority in service provision. This aims to give them the knowledge and capacity to expand future physiotherapy from what was once a traditional ‘mono-role’ into something advanced, exciting and current. Throughout practice based placements and these initial years, these new practitioners can demonstrate key attributes in foreseeing what services need to be developed to accommodate the changing population. Usually allied health professionals begin their career as graduates then following junior clinical years, will branch into specialisms as their career progresses however emerging roles and physiotherapy pathways are allowing them to structure their career accordingly resulting in practice being undertaken in a variety of untraditional settings. | |||
'''''‘Success requires not only the right vision but also the right workforce’''''' (DoH, 2008) | |||
<br> | |||
[[Image:Wiki1.jpg]] | |||
<br> | |||
== Learning Outcomes == | |||
On completion of this page: | |||
•The learner will be able to identify the knowledge, skills, behaviours and values which are required by physiotherapists working within emerging roles in the NHS. | |||
•The learner will be able to distinguish between different roles in physiotherapy practice and identify the knowledge, skills and qualifications required to work in each area. | |||
== Recent Related Research (from <a href="http://www.ncbi.nlm.nih.gov/pubmed/">Pubmed</a>) == | |||
<div class="researchbox"> | <div class="researchbox"> | ||
<span>Feed goes here!!|charset=UTF-8|short|max=10</span> | |||
</div> | </div> | ||
== References == | |||
References will automatically be added here, see <a href="Adding References">adding references tutorial</a>. | |||
</ | <span class="fck_mw_references" _fck_mw_customtag="true" _fck_mw_tagname="references" /></div> | ||
Revision as of 16:31, 5 November 2015
Original Editor - Your name will be added here if you created the original content for this page.
Top Contributors - Sophie Brewster, Ruaraidh McNaughton, Hetvi Kara, Stephen Rhys Evans, Omar Rasheed, Amy Young, Kim Jackson, 127.0.0.1, Chee Wee Tan, Evan Thomas, Admin, Michelle Lee, Sonja Murphy and Angeliki Chorti
Introduction[edit | edit source]
The goal of this resource is to provide a learning tool for students, recent graduates and junior physiotherapists at a time where integration of health and social care is a priority in service provision. This aims to give them the knowledge and capacity to expand future physiotherapy from what was once a traditional ‘mono-role’ into something advanced, exciting and current. Throughout practice based placements and these initial years, these new practitioners can demonstrate key attributes in foreseeing what services need to be developed to accommodate the changing population. Usually allied health professionals begin their career as graduates then following junior clinical years, will branch into specialisms as their career progresses however emerging roles and physiotherapy pathways are allowing them to structure their career accordingly resulting in practice being undertaken in a variety of untraditional settings.
‘Success requires not only the right vision but also the right workforce’ (DoH, 2008)
Learning Outcomes[edit | edit source]
On completion of this page:
•The learner will be able to identify the knowledge, skills, behaviours and values which are required by physiotherapists working within emerging roles in the NHS.
•The learner will be able to distinguish between different roles in physiotherapy practice and identify the knowledge, skills and qualifications required to work in each area.
•The learner will be able to identify further learning opportunities available to new graduates to assist in progressing to working in an emerging role.
•The learner will be able to critically reflect upon the challenges facing each emerging role and looking to the future, where each role will fit within the NHS.
Guide to Resource[edit | edit source]
This resource is an informative CPD package for new graduates looking into five emerging roles within the NHS. We will explore these roles independently and analyse how these fit into the 20/20 vision and the The National Delivery Plan for the Allied Health Professions in Scotland 2012-2015. We will also consider the pressures on the NHS at present and how each of the emerging roles we have decided upon will impact NHS service provision. We have also included email responses from selected physiotherapists who are working in these roles, in order to gain an insight into their views and experiences.
Content (hyperlinks)
We have selected the following emerging roles within physiotherapy. We are aware that there are many other roles that we will not be covering in the wiki, such as… (ADD TO) We have selected these roles as they have been recently discussed the physiotherapy magazine, Frontline and also at the annual physiotherapy UK conference and trade exhibition 2015 in Liverpool. The roles we have selected all fit into the main theme of the resource, which is relieving time pressures on the NHS.
Emerging roles:
- Prescribing rights
- Physiotherapists in emergency care settings
-Primary care/ GP surgeries - Injection therapy/ acupuncture
- Humanitarian Crisis
We intend to facilitate the learner's deeper understanding of these topics with opportunities for reflection and learning questions throughout. These will be outlined with the symbol: <img src="/images/e/ea/Question_Mark.jpg" _fck_mw_filename="Question Mark.jpg" alt="" />
?? Stepping stones table/ diagram ??[edit | edit source]
Workforce Development[edit | edit source]
Since 1948, the NHS workforce has erupted from approximately 144, 000 staff to a current 1.4 million in England alone with over 300 organisations (NHS, 2013). By 2033 over one quarter of the population will be aged over sixty-five. Demographically the health service will require future changes such as more first point of contact practitioners, increases in rehabilitation, prescribing abilities, and a higher need for surgical procedures and as a result, AHPs have recently been called upon to provide such services. Too often the range of knowledge, skills and competencies of AHPs is not fully and widely understood (DoH, 2008). Education opportunities and training programmes therefore must be integrally linked into current and emerging models or care in addition to scientific and technological advances. Allied Health Professionals (AHPs) have the talent and capacity to look beyond individual clinical practice and instead can are looking to maximise their contributions by getting involved in partnerships, leadership roles and scientific research (DoH, 2008; 2011).
<p><p>Training and Career Pathways
</p>
</p>
In most health organisations AHP career pathways are well established with junior practitioners progressing into clinical specialists, extended scope or advanced practitioners with a consultant role (ADD DESCRIPTORS)often being the pinnacle career goal. However, 2008 saw the launch of a UK-wide ‘Modernising Allied Health Professions Careers’ project, more recently known as Skills for HealthThis web-based tool was constructed to target AHPs planning more flexible and alternative career pathways to ensure breath and depth of expertise and maximise future employment opportunities. This resource provides professionals with a framework of competencies and includes a web-based resource documenting AHP and support worker roles. The Chartered Society of Physiotherapy (CSP) furthered this by providing a physiotherapy specific online resource for members to keep their knowledge and skills updated. This includes a set of learning and development principles, the code of professional values and behaviour and a framework of physiotherapy knowledge and skills hoped to be of use to current practicioners (CSP, 2010). It has been suggested that by offering greater clarity of accountability, responsibility and primary roles at all levels, this will lead to enhanced future workforce planning and training commissioning, ensuring that the in the future, patients will have access to a paramount level of care for their needs.In support of the 2020 vision to achieve a first class integrated workforce in the UK by 2020, this is hoped to aid planning and service redesign and pays particular attention to leadership and the capacity and capability of AHPs. In addition to training, from a commissioner’s perspective these tools help to develop services by maximising the potential of AHPs to play a larger role in transforming care, having the competency to work across organisational boundaries (DoH, 2008). Academia, research and management job opportunities have shifted the focus from effective clinical practice to ensuring this practice is evidence-based and up-to-date and is able to respond efficiently and effectively to accommodate changing service requirements. According to Framework 15 attracting and recruiting the right people into training programmes will benefit workforce planning for the future. Each year Health Education England (HEE) invests £4.8 billion of it’s £5 billion budget on education and training of this prospective workforce (HEE, 2014) to drive healthcare changes. However this said, 60% of this is spent on doctors making up 12% of the workforce while AHPs account for 40% of this population.
</p>
The Department of Health (2008) anticipate that in 10 years time, 60% of the current healthcare workforce will still be providing NHS services. Thus supporting them through career frameworks will help to fulfil their individual potentials. In the Framework 15 document (HEE, 2014) there are five global drivers of change considered. These are demographics; technology innovation; social, political, economic and environmental drivers; current and future service models and finally the expectations of patients and other staff. Workforce planners will utilise these factors when balancing an expected demand with an efficient demand(DoH, 2008). 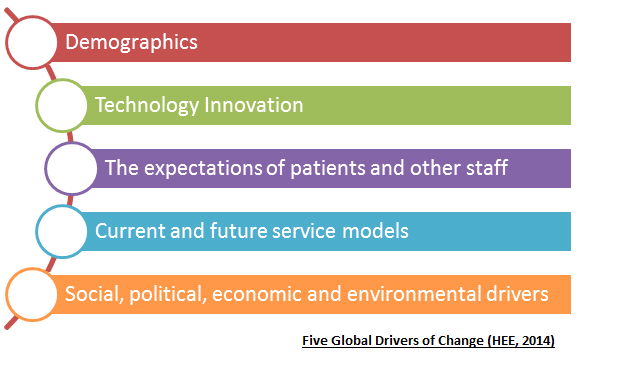
</p>
</p>
Primary Care[edit | edit source]
Description[edit | edit source]
Primary care is defined as the first point of contact for someone seeking medical care, typically a general practitioner or a family doctor. Primary care acts to coordinate any other specialists that the patient may need (World Health Organisation/Europe 2004).
Self-referral to physiotherapy is not covered in this wiki, as it is not considered a new or emerging role within the profession.
General Practitioners in the UK are suffering from an unstainable workload, which is limiting their appointment times with patients. Despite this, the government continues to push for GP surgeries to be open 7 days a week. If these plans go ahead, the strain placed on these AHPs will continue to grow. Added to the fact that the UK has an aging population, the strain on GPs and the rest NHS will not reach breaking point if drastic changes in primary health care are not made. The following is a quote from Sara Khan, a GP from Hertfordshire (Khan 2013): “patient demand has steadily risen, in many cases from an increasingly ageing population. It is to be celebrated that modern medicine is helping us live longer, but a side effect is that we develop conditions that require expensive care. My appointments with older patients are frequently longer due to multiple, complicated health needs that require careful need and attention. This inevitably eats into the time I have for appointments with other patients.”
This article, <a href="http://www.theguardian.com/commentisfree/2013/jul/24/stop-blaming-gps-out-of-hours-nhs">avaialble here</a> is one of many highlighting the current issues surrounding primary care in the UK.
This unstainable workload has caused great unrest among GPs, leading to the looming GP crisis. A survey of 1,004 GPs in the UK, as part of the BBC’s Inside Out programme (BBC 2015) found that 56% said they plan to retire before they turn 60. The workload, out of hours working and volume of consultations were some of the reasons for this. A summary of the findings can be found <a href="http://www.bbc.co.uk/mediacentre/latestnews/2015/inside-out-family-doctors">here</a>.
Due to a lack of government funding and the likely shortage of GP’s, the role of physiotherapists in primary care is currently being explored. The importance of the profession in the future of primary care is highlighted in a report by the Primary Care Workforce Commission (2015). <a href="http://hee.nhs.uk/wp-content/blogs.dir/321/files/2015/02/The-future-of-primary-care-v7-webFINAL.pdf">The report</a> endorses self referral to services and highlights the potential benefits of physiotherapists working alongside GPs, as a first point of contact for patients. Physiotherapists pride themselves for being autonomous in assessing, diagnosing, treating and discharging patients. Some advanced practitioners and extended scope practitioner physiotherapists are trained to prescribe drugs and provide injection therapy to patients.
“GPs within the West Wakefield Health and Wellbeing Project have developed a hypothesis that 50% of a GP’s workload could be undertaken by other staff. I want physiotherapy to form a significant part of this 50%” Dr Chris Jones, Programme Director, West Wakefield Health and Wellbeing Project.
(Taken from CSP leaflet: physiotherapy works for primary care (CSP LEAFLET). A link to the leaflet can be found <a href="http://www.csp.org.uk/professional-union/practice/your-business/evidence-base/physiotherapy-works/primary-care">here</a>.
<img src="/images/7/70/Physio_works_for_primary_care.png" _fck_mw_filename="Physio works for primary care.png" alt="" />
Rachel Newton, the CSP’s head of policy, has asked for CSP physiotherapists with experience of working in primary care to come forward and share their experiences. She told Frontline magazine “Evidence from members is essential to making the case to decision makers for the potential for physiotherapy within primary care” (CSP 2015ii). The <a href="http://www.csp.org.uk/icsp/primarycare">Primary Care iCSP group</a> was set up for CSP members to share experiences and benefits of physiotherapy in primary care.
Question: Isn’t self referral to physiotherapy the same as seeing a physiotherapist in primary care?
Answer: No. As with any self referral to a health service, you will still be placed on a waiting list. Ideally waiting times for Physiotherapist working in primary care will be the same as for GPs.
Cost Effectiveness[edit | edit source]
The main proposed benefit of physiotherapists working in primary care is reducing healthcare costs. It is estimated that MSK conditions make up 30% of a GPs appointments, yet 85% of those do not need to see a GP (Ludvigsson and Enthoven 2012). If patients were offered different professionals as their first point of contact, a huge number of GP appointments would be made available. The following costs saving benefits have been suggested by a CSP leaflet: physiotherapy works for primary care (CSP LEAFLET).
- Reduce referrals to secondary care orthopaedics
- Reduce unrequired investigations (x-ray, MRI)
- Reduce onward referrals to physiotherapy in community and secondary care
- Increase the number of patients able to self-manage effectively increase the number of referrals to leisure centres and other forms of physical activity prevention
However, there is no reference provided for these statements, therefore their relevance is questionable.
An <a href="http://www.csp.org.uk/frontline/article/vanguard-primary-care-treatment-musculoskeletal-conditions">article</a> in Frontline magazine (CSP 2015i) describes the need for physiotherapy as a profession to adapt and expand in response to the NHS England’s Five year forward view (NHS ENGLAND 2014). This calls for a step change in the integration of services to improve primary care. The frontline article is focuses on the 5-year journey of Amanda Hensman-Crook, formally a band 8a physiotherapist. After a successful 3 month pilot working alongside GPs, she was offered a permanent post at the GP practice, under the new title of MSK practitioner. Her pilot was based on estimates that approximately one in three GP consultations are MSK related. An audit of the service since June 2015 suggests a 20% fall in referrals to secondary MSK treatment. GPs and patients were found to be very happy with the service. A downside of this innovative service is that physiotherapists in this role will have shorter appointment times with patients. According to the article, the Hampshire service offers a 20 minute consultation, which is half the typical appointment time for a secondary care MSK service. This shows that physiotherapists can be effective in working alongside GPs as a first point of contact. If physiotherapists have the required knowledge and skills, they can relieve some of the pressures on GPs in primary care. The reduction in referrals to secondary MSK treatment highlights the money saving benefits of this system.
<img class="FCK__MWTemplate" src="http://www.physio-pedia.com/extensions/FCKeditor/fckeditor/editor/images/spacer.gif" _fckfakelement="true" _fckrealelement="4" _fck_mw_template="true">
Youtube Video – NHS Wales – advanced MSK physiotherapists
Training/ Qualifications[edit | edit source]
From the literature, it appears to mainly advanced practitioner physiotherapists who are working alongside GPs in primary care. Amanda Hensman-Crook, who began working in a GP practice LINK, was a band 8a physiotherapist before she started working under the title of advanced practitioner. The following is a link to a short descriptor of advanced practitioner physiotherapists. LINK . Further training/qualifications to become an advanced practitioner physiotherapist include:
- One year university courses, such as the MSc advanced practitioner physiotherapist course at the University of East Anglia. These courses offer further learning for qualified physiotherapists in advanced areas, such as independent and supplementary prescribing.
- A high level of experience is required by employers. Band 5 physiotherapists will first have to specialise in one area of physiotherapy and then gain considerable experience in this area.
Band 7 physiotherapists are expected to take up a leadership role within the team. This includes helping less qualified physiotherapists further their learning through CPD exercises. They are also expected to be comfortable managing complex cases and be experts in reviewing emerging evidence within their area of specialised knowledge.
A barrier to progressing to advanced practitioner level is course fees for advanced physiotherapy masters courses. Fees range from £7000 for UK/EU students to £15000 for international students.
As working in primary care is an emerging role in physiotherapy the NHS is still piloting the idea around the UK. As a result, there is no recognised progression pathway beyond reaching an advanced practitioner level of expertise.
Evidence to support[edit | edit source]
A study by Ludvigsson and Enthoven (2012) evaluated physiotherapists as primary assessors of patients with MSK conditions. 51 patients with a MSK disorder were primarily assessed by a physiotherapist and 42 by a GP. Participants completed a patient satisfaction questionnaire. It was concluded that physiotherapists can be used as primary assessors of MSK conditions in primary care, as few patients needed additional GP assessment. The physiotherapists were found to be capable of identifying confirmed serious pathologies and patient satisfaction was higher with physiotherapists than GPs. The participants who were seen by a physiotherapist felt confident in the information they received and the support to self-manage their conditions. The main limitation of the study, acknowledged by the authors was the participants were not randomly allocated to be seen by a physiotherapist or GP, thereby researcher bias is not excluded.
A study by Pinnington, Miller and Stanley (2004) evaluated prompt access to physiotherapy in the management of low back pain in primary care. The authors identify the issue of delays in getting access to specialised treatment in patients with low back pain. In the study, physiotherapist-led back pain clinics were established. Results were compared other published interventions from the literature. Data on pain, disability and well-being were collected at recruitment and 12 weeks later. The patients maintained diaries and GPs were interviewed before and after the study to obtain qualitative data. Comparative costings were derived from national and local sources. Results showed that more than 70% of the 614 patients seen only required a single visit and the majority of the patients were seen within 72 hours. Prompt access to physiotherapy reduced time taken off work and cost less per episode of back pain, compared with normal management. Qualitative data showed that patients valued early access to physiotherapy, particularly for reassurance. GPs also praised the service, largely due to the positive patient responses. This study shows the cost effectiveness among benefits of using physiotherapists as a first point of contact for patients with low back pain. This is more significant given low back pain is the most commonly presented MSK condition (Pinnington, Miller and Stanley 2004). A limitation is the study is from 2004, therefore the practices used by the physiotherapists are likely to be outdated. The study also does not specify the level or qualifications of the physiotherapists.
Holdsworth, Webster and McFadyen (2008) investigated physiotherapists and GPs views on self-referral and physiotherapy scope of practice. Data was gathered using a survey questionnaire, with both qualitative and quantitative questioning. They found the idea of physiotherapists working as first point of contact is strongly supported by the majority of physiotherapists and GPs. Potential benefits for patients were identified if physiotherapists adopted extended roles within a MSK setting, such as injection therapy and prescribing medications.
The following are examples of positive comments from physiotherapists and GPs extracted from Holdsworth, Webster and McFadyen (2008)
GP comments:
It makes logical sense, after all, physios are the experts when it comes to managing many musculoskeletal conditions’
Physiotherapists’ comments:
‘I was rather nervous of seeing self-referring patients at the start, wasn’t sure what to expect but now feel much more confident, it's just a question of being thorough and nothing more really’
‘I’m happy as I know that if I have any concerns, I can get the patients seen by their GP really quickly’
‘Our GPs have been great and want us to take on more aspects of the patients’ management as they see the time it could save them and they must trust us to want us to do this’
The Betsi Cadwaladr University Health Board (2015) in North Wales published results from a pilot study, in which advanced MSK physiotherapy practitioners are working in GP practices. LINK. It shows an additional 671 appointments were made available during the six-month pilot phase. Around one third of the appointments were MSK related which helped free-up GPs to concentrate on other patients and more complex cases. This data is from a National Health Board website, therefore can be deemed reliable.
In summary, an expansion of physiotherapy within primary care provides an immediate solution to GP shortages and delivers the transformation of primary care needed for a sustainable health system tailored to modern population needs (CSP 2015). More clarity is needed on how to reach these roles working alongside GPs in primary care and the additional qualifications required.
Self assessment questions:
1. From the above studies, what are the main proposed benefits of physiotherpaists working in primary care?
2. How did the patinets feel about being seen by physiotherapists, rather than GPs?
Challenges[edit | edit source]
As the concept of physiotherapists working alongside GPs is at the piloting stage, there is currently no established pathway beyond reaching an advanced practitioner or band 7 level of expertise. Because of this there are currently no postions in primary care being advertised for physiotherapists in the UK. From the research there appears to be no disadvantages of using physiotherapists as first point of contact as for MSK conditions. It is woth noting that the studies in the literature only use physiotherapists for MSK conditions. The ability of physiotherapists working in GP practices to assess, diagnose and treat patinets with other conditions, such as neorological remains to be seen. One challenge is training physiotherapists to the required level of expertise. However, the experience as working as a MSK specialist for a number of years appears to be sufficient.
Physiotherapists in Emergency Care Settings[edit | edit source]
Description[edit | edit source]
In recent years, physiotherapists have been placed in accident and emergency (A&E) departments to improve patient care, free up hospital beds by preventing unnecessary admissions and target optimal functioning of attendees. Emergency department physiotherapy is incorporated in the umbrella of an extended scope of practice. Clinicians in this area display a considerable depth of academic knowledge, clinical skills and experience and may be involved in providing interventions traditionally beyond the physiotherapy scope of practice (Anaf & Sheppard, 2007). In addition to frontline emergency physiotherapy practitioners (EPPs), increasingly physiotherapists are being made part of the integrated multidisciplinary team working in A&E and on medical assessment units (CSP, 2011). In Scotland such teams are seen at the Borders General Hospital where the Rapid Assessment and Discharge team are heavily involved in early patient contact, and the Integrated Assessment Team at the Victoria Hospital in Fife who carry out a falls assessment on every patient over the age of 64 attending A&E and assist with safe discharge (NHS Fife, 2014). It is recommended that 80% of patients attending A&E not staying in to be admitted should have length of stay less than 240 minutes (Taylor et al. 2011). These practitioners support medical professionals in assessing patients presenting with musculoskeletal conditions, helping to reduce breaches of this four hour waiting target and excessive delays (CSP, 2011)BBC News Article: A&E Waiting in England Worst for a decade.This allows patients to be assessed and either admitted or discharged home in a timely and safe manner with the appropriate resources in an attempt to prevent future re-admissions. The physiotherapist is also able to liaise with the MDT in deciding if the patient requires further input such as increased care package or community physiotherapy. In August 2013, in response to NHS England’s urgent and Emergency Care Review, the CSP confronted the increased need for physiotherapy services in acute medical departments, including A&E (McMillan, 2013).To meet the growing demands of emergency healthcare, EPPs operate as frontline staff whose role includes the assessment of musculoskeletal conditions, sending for further investigations such as bloods and scans, the management of soft tissue injuries and wounds in addition to educating and advising. This allows for doctors working in the department to focus their attention to more complex acute cases and improves the flow of patients through the system. Frontline physiotherapists are particularly relevant in treating the elderly where admission to hospital is much more likely to result in a consequential spiral of hospital acquired infections, delirium and often reduced functional capacity, resulting in extended stays. An increasing elderly population and patients with two or more long term conditions has recently meant two out of three A&E visits are for those falling into these brackets and with increased access to GP out of hours services since 2004 there has been an additional 4 million A&E attendants (Reesᵃ, 2015). Increases in bed occupancy yet a 6% decrease in bed numbers since 2010 has seen patients being shifted between wards, putting further extension on their length of stay (Reesᵇ, 2015) Historically allied health professionals in A&E were occupational therapists due to their main role in the organisation of discharges. However, with the integration of health and social care advancing multidisciplinary team working, currently in situations such as these, there is an overlap in physiotherapist and occupational therapist roles in order to provide the best possible approach to patient-centred care.
One of our student editors has placement experience with the RAD team at the Borders general Hospital near Melrose. She reports:
“The Rad team which was still being piloted at the time of my placement was made up of one band 6 physiotherapist, one occupational therapist and a further senior physiotherapist with a dual physiotherapy and social care role. Although I was only there for a short period, it was clear the positive effects this set up was having on acute care and I really enjoyed being part of something current and emerging. We aimed to see patients within 12 hours of attending A&E if required, whether that be on the Medical Assessment Unit following admission or if they were discharged home we would contact them via the phone and even go and see them in the community when necessary. The set up of the team enabled interdisciplinary assessments of mobility and functional ability e.g. self-care to occur, providing patients with the appropriate resources and equipment to ensure a safe discharge and reduce the change of future re-admission. In A&E the majority of the patient’s we saw had newly acquired walking aids so time was spent teaching their use and working with the patient to ensure they were able to function optimally and safely in their home environment. We also saw patients who had long term conditions that unrelated MSK problems were now making harder to manage.
My favourite aspect of the placement was the variation. One day could be spent in MAU, preparing patients for discharge without any requirement for the team in A&E while other days could be spent solely in A&E or out on home-visits without a hospital ward in sight. This highlighted to me how the profession is changing as we try to move care out into the community. I was aware however of some challenges facing the team. Due to being a pilot the team was still establishing itself across the hospitals, with better knowledge of its purpose in some areas than others. This also meant that here was also no set protocol as to when RAD input was sourced and different methods of triage were being tried and tested over the course of my placement. This finished with the prospect of the RAD team being based in the A&E department to increase awareness. I did not have any doubt however that with a bit of perseverance this would happen.”
In view of this tight window in which to see suitable patients, NHS London Care Commissioning Standards (NHS Healthcare for London, 2011) state that many hospitals have reviewed their A&E services, extending emergency physiotherapy input to cover weekends and extended hours in order to maximise the cost-effectiveness of the service.
Cost Effectiveness[edit | edit source]
With the average cost of an A&E visit costing the NHS approximately £115 this method of service provision reduces direct costs with similar clinical outcomes (CSP, 2011). The CSP evidence-based briefing Physiotherapy Works: Accident and Emergency found that in 2012-2013 of the 18.3million people that attended A&E, around 21% presented with musculoskeletal (MSK) related injuries, an estimated £440 million worth of healthcare costs. 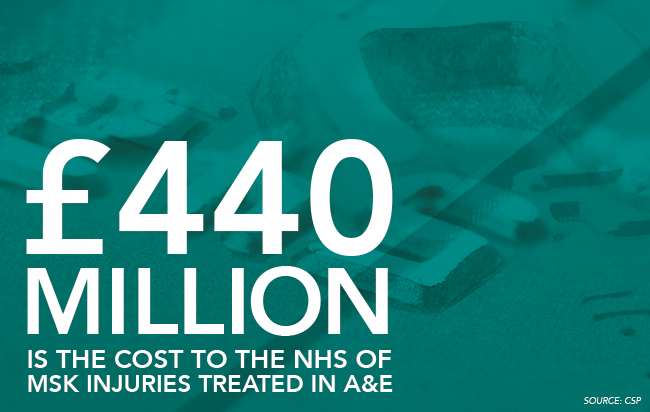
It was recorded that 446000 more people attended emergency departments throughout the UK in 2014 compared to 2013 (Reesᵃ, 2015). Winter 2014-2015 therefore saw huge negative media coverage of A&E provision with increased demand and rises in missed targets with higher reported major incidents (Jenner, 2015; Reesᵃ, 2015)BBC News Article: NHS set for a bumpy start to 2015. Incapacity in emergency departments was quoted as being “the biggest operational challenge facing the NHS” (Reesᵃ, 2015).In light of this, it is being more accepted that in order to lower the pressures and direct costs of these deficiencies, the skill mix of AHPs should be exploited (Jenner, 2015). If used properly, the abilities of physiotherapists could bring huge benefits in the assessment, diagnosis and treatment of MSK and chronic respiratory exacerbations such as Chronic Obstructive Pulmonary Disorder, in addition to providing vast experience and learning opportunities for the physiotherapists themselves (Jenner, 2015).
Training/ Qualifications[edit | edit source]
Integration of roles requires training at masters level in addition to being signed off as competent. McMillan (2013) reports the role as a challenging varied environment with a high degree of responsibility and that previous MSK experience will assist with the management of what comes literally through the front door. Conditions can include minor head or rib injuries which if dealt with incorrectly can mean dealing with life or death situations (McMillan, 2013). Richard Parris a consultant in emergency medicine is optimistic about the future of physiotherapists in the emergency department: “the physiotherapists are a real asset…we don’t have any hierarchy or boundaries”, however reports that it is not for the faint hearted (McMillan, 2013).
In Australia, emergency physiotherapists must have a minimum of 5 years clinical practice post-graduation including 3 years spent in a relevant specialist area. Additional training or postgraduate study in a relevant clinical area is also desirable (Crane & Delany, 2011). However, there is currently a lack of a clear direct career pathway to get to this position meaning that practitioners are responsible for developing their own range of specialist skills. MSK postgraduate or masters certificates tend to be more directed at outpatient and private physiotherapy roles instead of for use in the emergency department. In Australia, most emergency physiotherapists are undertaking short courses such as plastering, sports, spinal and vestibular to complement their practice.
It has been realised that educational requirements for this sort of role placed within the broader health system network, however, needs to be standardised across settings in order to establish the wider effect of the service. Educational support including onsite training and supervision can be used as part of the programme in addition to certified courses in the absence of specific qualifications however this still means there is a lack of overall structure of training and defines the need for evidence-based regulatory.
Evidence to support[edit | edit source]
The UK is the worldwide leader in innovative physiotherapy practice (Crane&Delany, 2013). Services are continuously changing to meet the growing and changing patient demands while increasing workforce flexibility (Crane & Delany, 2013). As a result there is an evolving need to provide practitioners with an ethical and evidence-based framework to support changing practice such as the development of the emergency physiotherapist role. Within Australia, career paths are widening for physiotherapists as they try to establish similar counterparts (Crane&Delany, 2013) due to an increasing demand on emergency departments. Some would argue the emergency physiotherapist role has been better suited to the political need to improve patient waiting times rather than patient outcomes, however, Taylor et al. (2011) found that patients with musculoskeletal problems presenting at A&E were just as, if not more satisfied to see a physiotherapist as the first point of contact. Crane and Delany (2013) suggested that musculoskeletal physiotherapists expand their physiotherapy practice in the emergency department by requesting and interpreting radiology results, blood tests,x-rays managing minor wounds and fractures, applying plaster, managing analgesia and referring on to the most appropriate option in an efficient manner. Although predominantly involved with the management of MSK conditions Effectiveness of musculoskeletal emergency practitioners. Anaf and Sheppard (2007) comment on the emergency Physiotherpists role in effectively managing minor chest fractures, whiplash, recent burns limiting functional movement and torticolosis.
Similar to the UK, in Australia Crane and Delany (2013) found that EPs enabled doctors to treat more critical and complex patients faster and reduced overall waiting time through the emergency department. Taylor et al. (2011) found that when operating as primary contact practitioners, patient length of stay could be reduced by up to 59.5 minutes compared with secondary contact practitioners. In the same non-randomised controlled trial, waiting time and treatment time of those attending A&E was also reduced following treatment by an emergency physiotherapist compared to secondary contact. This was thought to be a result of bypassing the initial doctor’s assessment. In addition to reducing the workload of other staff, this system improved patient flow and had no significant impact on re-presentation rate (Taylor et al. 2011) When satisfaction rates were investigated in this study, 85% of patients attending a physiotherapist in the emergency department were satisfied with the treatment they received as were 82% of patients who first saw a doctor followed by a physiotherapist. However, those receiving the primary physiotherapy contact felt things were explained more effectively and that they were given more time to ask questions and discuss their condition (Taylor et al. 2011).
The systematic review conducted by Kilner (2011) analysed the literature surrounding physiotherapists working as emergency practitioners, specifically its effect on health outcomes. Despite the previous findings, this research review did not fully support the engagement of physiotherapists in the emergency care setting. The ‘access block 'experienced across emergency departments worldwide requires government, economic and societal input overtime with physiotherapists working in emergency departments only a short-term solution to a long-term problem. However, Jogodka and Lebec, (2008) argue the need for mobility and exercise experts in the emergency departments and that when used appropriately, physiotherapists seen here can facilitate healing and prevent secondary complications. Kilner (2011) analysed that emergency physiotherapy affects outcomes on three main levels: system, provider and client. It was determined that although physiotherapists working in A&E were more likely to give advice to patients and arrange for follow up physiotherapy that doctors or nurses working in the same area, at a system and provider level, there is insufficient existing evidence regarding the effects of physiotherapy in A&E. Richardson et al. (2005) for example conducted a randomised controlled trial which failed to establish the cost-effectiveness of such a service. Kilner (2011) agreed that emergency physiotherapy resulted in increased patient satisfaction, decreased waiting times and improved clinical outcomes in the short term, however were not convinced of the reliability of its long term effects.
Challenges[edit | edit source]
The biggest challenge to physiotherapists working in emergency care settings is a lack of adequate funding as explained by... (VIDEO CLIP).Crane and Delany (2013)however also found that there was a possibility that patient satisfaction with primary contact physiotherapists could be due to the decreased waiting time they experienced rather than the interaction had and treatment received from the professional. In addition to this they found that there was nothing specific to say that the decreased waiting times were not due simply to an extra member of staff working in the department, not necessarily a physiotherapist. However they felt that by varying the skill mix in the department, better outcomes were being achieved and McClellan et al. (2006) analysed that even when compared to a doctor, patients with MSK related conditions preferred to see a physiotherapist directly. Despite these boundaries, Taylor et al. (2011) analysed that both patients and fellow staff reported high levels of satisfaction with emergency physiotherapists. The main variation came from staff knowledge regarding the proficiency and scope of emergency physiotherapists of which they (Taylor et al. 2011) investigated. This was particularly true amongst other staff members in the emergency department (Taylor et al. 2001). It appeared [in Australia] there was a general debate as to if physiotherapists were working with an extended scope of practice or if they were just advancing their already established skills. However, in the UK, emergency physiotherapists have been defined as ‘clinical specialists working beyond recognised scope of physiotherapy practice in innovative or non-traditional roles ‘(Crane & Delany, 2013).
Working in newly formed teams can prove difficult for physiotherapists in emergency settings. Inter-disciplinary relationships must be built quickly in a pressurised environment where individuals tend to have more responsibility than other roles (Anaf & Sheppard, 2007; Crane & Delany, 2013) as unlike outpatient and inpatient settings, emergency departments are much less hierarchical resulting in an increased level of duty.
Case Studies of Hospitals offering this service[edit | edit source]
Salford Royal NHS Foundation treats 88500 patients in A&E annually. In 2010 an advanced physiotherapy practitioner role was introduced in the department to treat MSK presentations. This includes the ordering of x-rays and further tests in addition to managing ongoing referrals. This service has been proposed to reduce waiting times while providing high quality and efficient service with direct access to a physiotherapist available to all presenting patients. The foundation has reported a cost saving of approximately £32 per patient (a 60% reduction) largely due to a reduced need for more expensive medical staff. 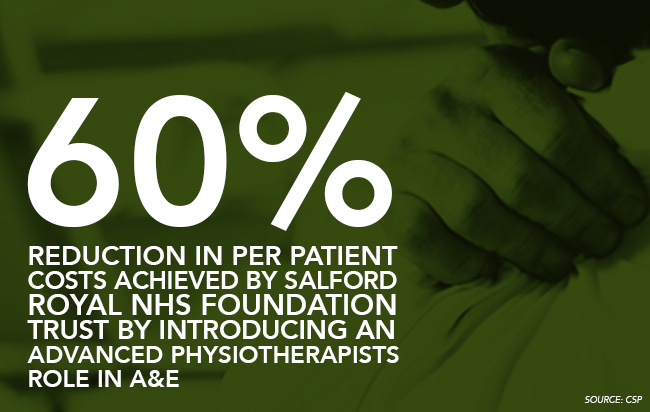
The Royal Bolton Hospital provides clinical specialist physiotherapists in their A&E department to deal with their relentless influx of patients and attributes much of their success and enviable record of prompt treatment and discharge to this provision. Usman Arif is one of these practitioners and also clinical lead for three additional physiotherapists sharing their time between the emergency department and MSK outpatients. He comments: “Every day here is different. It’s stimulating and the workload is so varied I learn something new every week” (McMillan, 2013). The first pilot scheme was launched in 2003 with working hours 8am-4pm weekdays and 8-6pm at weekends with enhanced pay (McMillan, 2013). In addition doctors in A&E have the scope to request a second opinion of a physiotherapist at a later date when very acute injuries and pain can limit their own initial assessment. Mr Arif went on to report:
“ we work with “minors” [those with less serious illnesses or injuries] as autonomous practitioners with an extended scope of practice, and also provide some input to paediatrics.”
Furthering this, many of the physiotherapists in this role are working towards their right to independently prescribe. Often already holding supplementary prescribing rights, Mr Arif comments that this is not adequate when working in A&E with patients you don’t see on a regular basis.
Victoria Hospital Fife
Borders General Hospital
Self assessment questions:
1. What part does physiotherapy in emergency care settings have to play in the 20:20 Vision and AHP National Delivery Plan for Scotland? What proposed benefits will most likely facilitate these strategies?
2. Think back to a previous visit to the accident and emergency department either for yourself or a family member/friend, perhaps before you commenced your physiotherapy career. How would you have felt being treated by professional that was not a doctor? Do you think this would have affected your views of the service provided? Take a few moments to reflect on how you would have reacted in this situation previously compared to how you may react now having read the above information.
Prescribing[edit | edit source]
Description[edit | edit source]
<a href="http://www.bbc.co.uk/news/health-18955680">BBC News Article: Prescription Powers</a>
Cost Effectiveness[edit | edit source]
Training/ Qualifications[edit | edit source]
Evidence to support[edit | edit source]
Challenges[edit | edit source]
Injection Therapy[edit | edit source]
Description[edit | edit source]
Cost Effectiveness[edit | edit source]
Training/ Qualifications[edit | edit source]
Evidence to support[edit | edit source]
Challenges[edit | edit source]
Humanitarian[edit | edit source]
Description[edit | edit source]
Physiotherapists have a critical role in helping people that have been affected by pandemics, natural disasters and other major emergencies. Physiotherapists need to be engaged at an organizational level so that they can provide appropriate services to affected communities and areas by saving lives and improving outcomes for survivors of these emergencies.
The WCPT encourages engagement of physiotherapists when disasters of all sorts strike. Physiotherapists should
- be involved in developing ideas and policies that helps communities, areas, and towns prepare for disasters
- be involved in preventative measures and education throughout the disaster, also before and especially after
- provide appropriate treatment, intervention and rehabilitation to survivors
- ensure that areas have adequate access to appropriate physiotherapy treatment/interventions which includes rehabilitation to achieve best possible care for their needs.
- Prepare by learning about risks and preventions strategies to react to disasters from home, work and different environment settings
- Give particular attention to, and raise awareness for certain groups like elderly and disability groups at times of disaster
Taken from the CSP website : http://www.csp.org.uk/frontline/article/gaza-alert-physiotherapy-humanitarian-response,
Zoe Clift who is an extended scope practitioner and St Thomas hospital in London explained a typical day working in the Israel:
7am - At Handicap International (HI) office for security brief
9am - Meet with Rafah area team to start clinical visits. First patient (median nerve and flexor tendon injury) assessment/treatment plan completed by local Gaza team with only reassurance needed from us – fantastic to see the progress in their clinical skills and their growing confidence.
10am - Second clinical visit (median nerve and tibial ex-fix, plus patient’s son with head injury). Local physio points out where he lives amid the rubble ... a reminder for me of the situation the clinicians are living and working in.
12.30pm - Visit nine-year-old girl, arranged specifically for review of possible lower limb peripheral nerve injury and wound/dressing review. Referred to me and Lesley (major trauma nurse) as local therapy team all male. Simple clinical session gaining patient trust – emotionally this is probably the toughest case we have seen.
13.30pm - Debrief with Rafah team. Reassured them they are doing a fantastic job at learning new skills and applying them. Brilliant to feel we are leaving them with tools to continue.
3pm - Final mission de-brief at HI office. Extremely positive feedback. We agree to continue work to provide plan/guidance for next time – it’s not ‘if’ but ‘when
Speaking at the Physiotherapy UK conference and trade exhibition in Liverpool on the 16-17 of October, Peter Skelton, talked about the role of rehabilitation professionals responding to humanitarian emergencies and how it is becoming increasingly recognisable around the globe.
He informed that for the first time, physiotherapists were being initiated into emergency medical teams such as UKIETR. This new emerging role is being led by the World Health organisation (WHO) and in the UK, they are building its professional capacity to respond to emergencies via the UKIETR. This includes the training and recruitment of medical and allied health professionals by UK – Med and save the children.
Members will receive full training in humanitarian response, funding for the project and also backfill payments into the NHS. Handicap international have facilitated the recruitment of RP’s to the UKIETR. From this they have developed a rehabilitation specific training in collaboration with 10 different professional networks in the UK. They have developed theoretical and practical training components covering spinal cord injury, amputation, fracture, burns, nerve injury and soft tissue injury. The involvement of the professional networks is crucial as it ensures training is based on current best practice and gathers input form the UK’s leading clinicians.
At this present time, 63 rehabilitation professionals are on the register. One physiotherapist has been deployed to Typhoon Haiyan in the Philippines and 9 physiotherapists have been deployed to the Gaza crisis to treat patients and to provide specialised education to local health professionals.
Peter Skelton concluded that this is the first time specialised humanitarian training has become available to those who wish to work within humanitarian emergencies. However he believes there still needs to be an improvement in recruitment of physiotherapists who are highly skilled in trauma.
Doctors without borders are a group of health professionals which help people deal with the complications of war. They are a international humanitarian organisation who are best known for their contribution in war - torn regions and developing countries. At this present times, they have 60 on-going projects around the world. Their main aim is to provide healthcare support to those needed, however they also carry out research to provide evidence which supports the healthcare they are providing.
Here is a video showing the work doctors without borders do when dealing with a natural disaster:
<img class="FCK__MWTemplate" src="http://www.physio-pedia.com/extensions/FCKeditor/fckeditor/editor/images/spacer.gif" _fckfakelement="true" _fckrealelement="1" _fck_mw_template="true">
Cost Effectiveness[edit | edit source]
Volunteering[edit | edit source]
If you wish to be involved in a disaster area it is very important that it is done through an established group as opposed to doing it alone. Having different numerous individuals and small groups getting involved can be problematic as opposed to supportive. Usually governments have their own administrations and agencies working to capacity which is why they are unable to deal with individual volunteers. A list of organizations involved in relief programs can be found <a href="http://www.wcpt.org/node/36994">here</a>.
Sometimes these organisatinos assemble teams to serve in a particular area for week, sometimes even months. Careful planning and consideration by the individual physiotherapist needs to be taken to see if this is appropriate for the individual. Sometimes groups ask volunteers to make a 3 month commitment and often more on particular disasters.
Training/ Qualifications[edit | edit source]
Veterans international are a international humanitarian group that address the effects and consequences of war that has gone on in Cambodia. To apply to work with Veterans international you have to have the following :
•Have a Bachelors Degree in Physiotherapy or a related subject then you will be suited for this project.
•Ideally, a qualified physiotherapist would also possess at least two years’ experience of practicing professionally.
Evidence to support[edit | edit source]
Challenges[edit | edit source]
Conclusion[edit | edit source]
Recent Related Research (from <a href="http://www.ncbi.nlm.nih.gov/pubmed/">Pubmed</a>)[edit | edit source]
Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
References will automatically be added here, see <a href="Adding References">adding references tutorial</a>.
<span class="fck_mw_references" _fck_mw_customtag="true" _fck_mw_tagname="references" />






