Ramsay Hunt Syndrome
Original Editor - Wendy Walker
Lead Editors - Wendy Walker, Kim Jackson, Poonam Sepat, Evan Thomas, WikiSysop, Claire Knott, Naomi O'Reilly and Wendy Snyders
Introduction[edit | edit source]
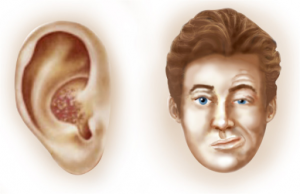
Ramsay Hunt [RHS] syndrome is defined as an acute peripheral facial palsy/neuropathy associated with erythematous vesicular rash of the skin of the ear canal, auricle (also termed herpes zoster oticus), and/or mucous membrane of the oropharynx[1]. It is commonly asociated with moderate to severe otalgia (earache).
This syndrome is also known as geniculate neuralgia or nervus intermedius neuralgia.
The syndrome was first described in 1907 by Dr James Ramsay Hunt, describing a patient who had otalgia (ear pain) associated with cutaneous and mucosal rashes, which he ascribed to infection of the geniculate ganglion by human herpesvirus 3 (ie, varicella-zoster virus [VZV])[2].
Mechanism of Injury / Pathological Process[edit | edit source]
Ramsay Hunt syndrome is defined as VZV infection of the head and neck that involves the facial nerve = the seventh cranial nerve (CN VII)[3]. Other cranial nerves (CN) might be also involved, including CN VIII, IX, V, and VI (in order of frequency). This infection often causes vesiculation and ulceration of the external ear, as well as ipsilateral facial neuropathy (in CN VII), radiculoneuropathy, or geniculate ganglionopathy. In some cases there are also vesicles on the ipsilateral anterior two thirds of the tongue and soft palate.
VZV infection causes 2 distinct clinical syndromes. Primary infection, also known as varicella or chickenpox, is a common pediatric erythematous disease characterized by a highly contagious generalized vesicular rash. The annual incidence of varicella infection has significantly declined after the introduction of mass vaccination programs in most countries of the world[4].
After chickenpox, VZV remain latent in neurons of cranial nerve and dorsal root ganglia. Subsequent reactivation of latent VZV can result in localized vesicular rash, known as herpes zoster. VZV infection or reactivation involving the geniculate ganglion of CN VII within the temporal bone is the main pathophysiological mechanism of Ramsay Hunt syndrome
Clinical Presentation[edit | edit source]
The presenting feature is often otalgia: pain deep within the ear. A herpetic rash or blisters, which may be on the skin of the ear canal, auricle or both. Facial palsy develops either concurrently or after several days of the otalgia.
Patients usually present with paroxysmal pain deep within the ear. The pain often radiates outward into the pinna of the ear and may be associated with a more constant, diffuse, and dull background pain. The onset of pain usually precedes the rash by several hours and even days.
Classic Ramsay Hunt syndrome can be associated with the following[5]:
Vesicular rash of the ear or mouth (as many as 80% of cases)
The rash might precede the onset of facial paresis/palsy (involvement of the seventh cranial nerve [CN VII])
Ipsilateral lower motor neuron facial palsy (CN VII)
Vertigo and ipsilateral hearing loss (CN VII)
Tinnitus
Otalgia
Headaches
Dysarthria
Gait ataxia
Fever
Diagnostic Procedures[edit | edit source]
In most cases, the diagnosis is made purely on clinical findings: the presence of herpetic blisters in and around the ear, accompanied in most cases by pain in and around the ear and an ipsilateral facial palsy.
On occasions virological studies, both serological and molecular, can be used to confirm the clinical diagnosis.
In particular, VZV antigen detection by direct immunofluorescence assay (DFA) is used, which has sensitivity of 90% and specificity close to 99%[6].
Structural lesions (such as Acoustic Neuroma) can be ruled out by MRI or CT scan.
Medical Management[edit | edit source]
Corticosteroids and oral acyclovir are commonly used in the treatment of Ramsay Hunt syndrome. In one review, combined therapy using corticosteroids plus intravenous acyclovir did not show benefit over corticosteroids alone in promoting facial nerve recovery after 6 months. The Cochrane Study on antiviral medication in RHS concludes that more studies are needed[7].
Vestibular suppressants may be helpful if vestibular symptoms are severe.
As with Bell's palsy, care must be taken to prevent corneal irritation and injury. Referral should be made to an Opthalmologist. Also, see advice page on Dry Eye for further information.
Patients with long term facial palsy may also experience dental problems: see advice page on Dental Issues
Differential Diagnosis[edit | edit source]
The following conditions can present in with similar symptoms@
Bell's Palsy - this is the most common cause of sudden onset, non-traumatic facial palsy, and can be differentiated from RHS by the absence of severe otalgia (only mild pain in the region of the mastoid usually occurs in Bell's Palsy) and the absence of vesicles and involvement of other cranial nerves.
Persistent Idiopathic Facial Pain - this is not associated with facial palsy
Postherpetic Neuralgia - not associated with facial palsy
Temporomandibular Disorders - not associated with facial palsy
Trigeminal Neuralgia - not associated with facial palsy
Physiotherapy Interventions[edit | edit source]
Physiotherapy management of the facial paralysis or weakness is as detailed in the section on Facial Palsy.
It is also important to provide information on care of the eye in order to prevent formation of corneal ulcer: see advice page on Dry Eye.
Resources[edit | edit source]
The charity Facial Palsy UK have a page on RHS
The website RamsayHunt.org offers information and support
American organisation National Organization for Rare Disorders has a useful page on RHS
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1PAjVVEin27IaEPoWa7fz5k1_hztXaknK1vTt1wxgmW0R-pQFH|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
- ↑ Bhupal HK. Ramsay Hunt syndrome presenting in primary care. Practitioner. 2010 Mar. 254(1727):33-5
- ↑ Goldani LZ, Ferreira da Silva LF, Dora JM. Ramsay Hunt syndrome in patients infected with human immunodeficiency virus. Clin Exp Dermatol. 2009 Jun 1
- ↑ Furuta Y, Aizawa H, Ohtani F, et al. Varicella-zoster virus DNA level and facial paralysis in Ramsay Hunt syndrome. Ann Otol Rhinol Laryngol. 2004 Sep. 113(9):700-5
- ↑ Kleinschmidt-DeMasters BK, Gilden DH. The expanding spectrum of herpesvirus infections of the nervous system. Brain Pathol. 2001 Oct. 11(4):440-51
- ↑ Ryu EW, Lee HY, Lee SY, Park MS, Yeo SG. Clinical manifestations and prognosis of patients with Ramsay Hunt syndrome. Am J Otolaryngol. 2011 Nov 8
- ↑ Coffin SE, Hodinka RL. Utility of direct immunofluorescence and virus culture for detection of varicella-zoster virus in skin lesions. J Clin Microbiol. 1995 Oct. 33(10):2792-5
- ↑ Uscategui T, Doree C, Chamberlain IJ, Burton MJ. Antiviral therapy for Ramsay Hunt syndrome (herpes zoster oticus with facial palsy) in adults. Cochrane Database Syst Rev. 2008 Oct 8. CD006851