Prescribing in Physiotherapy for Pain: Difference between revisions
Kim Jackson (talk | contribs) (Reworded introduction Treatment of pain) |
m (Corrected spacing and spelling) |
||
| (8 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Daniel Neilson|Daniel Neilson]], [[User:Darren Kripaitis|Darren Kripaitis]], [[User:David Rossiter|David Rossiter]], [[User:Mary Graham|Mary Graham]] and [[User:Rosy Cuthbert|Rosy Cuthbert]] as part of the [[Current_and_Emerging_Roles_in_Physiotherapy_Practice|Queen Margaret University's Current and Emerging Roles in Physiotherapy Practice Project]] <br>'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | <div class="editorbox"> '''Original Editor ''' - [[User:Daniel Neilson|Daniel Neilson]], [[User:Darren Kripaitis|Darren Kripaitis]], [[User:David Rossiter|David Rossiter]], [[User:Mary Graham|Mary Graham]] and [[User:Rosy Cuthbert|Rosy Cuthbert]] as part of the [[Current_and_Emerging_Roles_in_Physiotherapy_Practice|Queen Margaret University's Current and Emerging Roles in Physiotherapy Practice Project]] <br>'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== Introduction == | == Introduction == | ||
| Line 5: | Line 5: | ||
With changing demographics, higher expectations and an increase in long term conditions <ref>Department of Health. Long-term conditions compendium of information: 3rd edition. 2012; Available at: https://www.gov.uk/government/publications/long-term-conditions-compendium-of-information-third-edition. Accessed 5th November, 2015.</ref> there is a heightened pressure and demand on the NHS. To meet these demands the roles within the NHS have had to change and expand. As recently as 2013, physiotherapists in England have been granted the right to independently [[Prescribing Rights in the UK|prescribe]], giving them the ability to prescribe drugs, including some controlled drugs. These prescriptions must be used “within the overarching framework of human movement, performance and function” <ref>NHS England Publications. Frequently Asked Questions: Independent prescribing by physiotherapists and podiatrists Publications Gateway Reference 00364 . 2013; Available at:https://www.england.nhs.uk/wp-content/uploads/2013/08/faqs-ippp1.pdf. Accessed 15th November, 2015.</ref> | With changing demographics, higher expectations and an increase in long term conditions <ref>Department of Health. Long-term conditions compendium of information: 3rd edition. 2012; Available at: https://www.gov.uk/government/publications/long-term-conditions-compendium-of-information-third-edition. Accessed 5th November, 2015.</ref> there is a heightened pressure and demand on the NHS. To meet these demands the roles within the NHS have had to change and expand. As recently as 2013, physiotherapists in England have been granted the right to independently [[Prescribing Rights in the UK|prescribe]], giving them the ability to prescribe drugs, including some controlled drugs. These prescriptions must be used “within the overarching framework of human movement, performance and function” <ref>NHS England Publications. Frequently Asked Questions: Independent prescribing by physiotherapists and podiatrists Publications Gateway Reference 00364 . 2013; Available at:https://www.england.nhs.uk/wp-content/uploads/2013/08/faqs-ippp1.pdf. Accessed 15th November, 2015.</ref> | ||
It is important for physiotherapists to understand their scope and limitations to allow them to practice within this framework, as with this change we need to ensure that we remain working within our scope of practice to give the safest and best possible patient centred care. In a narrative review, Crane and Delany<ref name="Crane and Delany 2013">Crane J, Delany C. Physiotherapists in emergency departments: responsibilities, accountability and education. Physiotherapy 2013; 99:95-100.</ref> | It is important for physiotherapists to understand their scope and limitations to allow them to practice within this framework, as with this change we need to ensure that we remain working within our scope of practice to give the safest and best possible patient centred care. In a narrative review, Crane and Delany<ref name="Crane and Delany 2013">Crane J, Delany C. Physiotherapists in emergency departments: responsibilities, accountability and education. Physiotherapy 2013; 99:95-100.</ref>comment that physiotherapists demonstrate an excellent ability to clinically reason and adapt to the changing needs of the societies they serve. The UK government has been convinced that prescribing is within physiotherapy’s scope because physiotherapists already possess the core skills that it requires. | ||
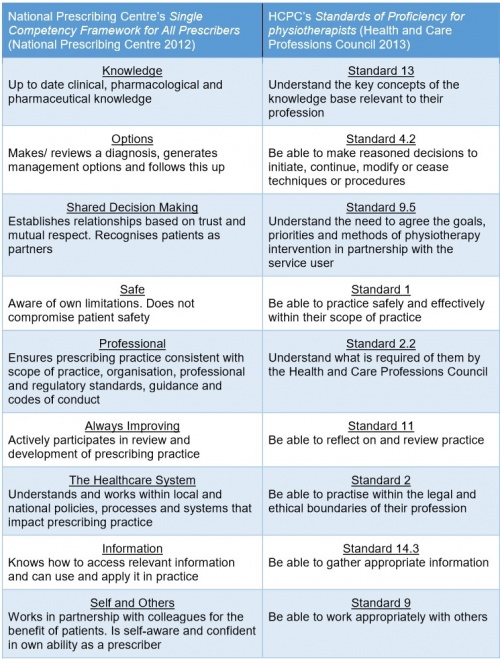
The National Prescribing Centre<ref>National Prescribing Centre., A single competency framework for all prescribers. http://www.webarchive.org.uk/wayback/archive/20140627112901/http://www.npc.nhs.uk/improving_safety/improving_quality/resources/single_comp_framework_v2.pdf (accessed 6 Nov 2015)</ref> has produced a framework that applies to all prescribers, no matter what profession they come from. Below is a comparison of this framework it to the HCPC’s Standards of Proficiency for physiotherapists<ref>Health and Care Professions Council. Standards of proficiency: Physiotherapists. http://www.hcpc-uk.co.uk/assets/documents/10000DBCStandards_of_Proficiency_Physiotherapists.pdf (accessed 11 Nov 2015).</ref>: | The National Prescribing Centre<ref>National Prescribing Centre., A single competency framework for all prescribers. http://www.webarchive.org.uk/wayback/archive/20140627112901/http://www.npc.nhs.uk/improving_safety/improving_quality/resources/single_comp_framework_v2.pdf (accessed 6 Nov 2015)</ref> has produced a framework that applies to all prescribers, no matter what profession they come from. Below is a comparison of this framework it to the HCPC’s Standards of Proficiency for physiotherapists<ref>Health and Care Professions Council. Standards of proficiency: Physiotherapists. http://www.hcpc-uk.co.uk/assets/documents/10000DBCStandards_of_Proficiency_Physiotherapists.pdf (accessed 11 Nov 2015).</ref>: | ||
[[Image:Grp6 table 1.jpg|border|center|500x700px]] | [[Image:Grp6 table 1.jpg|border|center|500x700px]] | ||
== Scope of Practice == | == Scope of Practice == | ||
Prescribing may appear a strange addition to a physiotherapist’s toolkit and outside the remit of the profession, which are defined by the Chartered Society of Physiotherapy<ref>Chartered Society of Physiotherapy. Medicines, prescribing and physiotherapy. file:///C:/Users/user/Downloads/csp_pd019_medicines_prescribing_physiotherapy_2013_0.pdf (accessed 25 Oct 2015)</ref> as anything within the 4 pillars of practice. These are: | Prescribing may appear a strange addition to a physiotherapist’s toolkit and outside the remit of the profession, which are defined by the Chartered Society of Physiotherapy<ref>Chartered Society of Physiotherapy. Medicines, prescribing and physiotherapy. file:///C:/Users/user/Downloads/csp_pd019_medicines_prescribing_physiotherapy_2013_0.pdf (accessed 25 Oct 2015)</ref> as anything within the 4 pillars of practice. These are: | ||
| Line 33: | Line 18: | ||
#Kindred methods of treatment | #Kindred methods of treatment | ||
Any physiotherapist must not only work within their own personal scope of practice, but also within the scope of the profession.<ref>Chartered Society of Physiotherapy. Practice guidance for physiotherapist supplementary and/or independent prescribers in the safe use of medicines. file:///C:/Users/user/Downloads/csp_pd026_practice_guidance_prescribers_aug2013_0_0.pdf (accessed 25 Oct 2015)</ref> Although prescribing is within the scope of the profession, like any skill, it only becomes part of an individual physiotherapist’s scope of practice when they become competent through training<ref name="CSP 1" />. This means that before prescribing | Any physiotherapist must not only work within their own personal scope of practice, but also within the scope of the profession.<ref>Chartered Society of Physiotherapy. Practice guidance for physiotherapist supplementary and/or independent prescribers in the safe use of medicines. file:///C:/Users/user/Downloads/csp_pd026_practice_guidance_prescribers_aug2013_0_0.pdf (accessed 25 Oct 2015)</ref> Although prescribing is within the scope of the profession, like any skill, it only becomes part of an individual physiotherapist’s scope of practice when they become competent through training<ref name="CSP 1" />. This means that before prescribing can be deemed a suitable addition to a physiotherapist’s skill set, they must already be an expert in the field they wish to apply it<ref name="NPC 2012" />. As a consequence, although the scope of prescribing within physiotherapy is very wide, it is limited to only an individual's clinical speciality.<ref name="CSP 1" /> This is a major difference from medical prescribing who may prescribe for any condition. The following pre-requisites are necessary so safely undertake the role of prescribing: | ||
* Understand the legal context relevant to prescribing | |||
* Understand pharmacodynamics, pharmacokinetics, pharmacology and therapeutics relevant to prescribing | |||
* Understand different prescribing mechanisms | |||
* Able to make prescribing decisions based on relevant physical examination assessment and history taking | |||
* Able to communicate information about medicines and prescriptions clearly | |||
* Able to monitor response to medications and modify or cease treatment as appropriate within scope of practice | |||
* Able to undertake medication calculations | |||
* Able to identify adverse medication reactions, interactions and take appropriate action | |||
* Able to recognise medication error and respond appropriately | |||
Once a physiotherapist decides that prescribing would be of benefit to their practice there are two types of prescriber they can become, based on their level of training supplementary prescribers or independent subscribers. | Once a physiotherapist decides that prescribing would be of benefit to their practice there are two types of prescriber they can become, based on their level of training supplementary prescribers or independent subscribers. | ||
=== Supplementary Prescribers | === Supplementary Prescribers === | ||
Supplementary prescribers can prescribe any medication, but it must be detailed in a written CMP. The CMP is created in partnership with the patient and a medical prescriber.<ref name="CSP 1" /> This means that although they are accountable for their decision to prescribe, they share accountability with the medical prescriber for the decision to put the medication in the CMP<ref name="CSP 1" />. In their nursing supplementary prescriber counterparts, this leads many doctors to feel that they have the ultimate responsibility for both the supplementary prescriber and patient. This can result in supplementary prescribers feeling subordinate, rather than in partnership with their medical prescriber.<ref>Creedon R, Byrne S, Kennedy J, McCarthy S. The impact of nurse prescribing on the clinical setting. British Journal of Nursing 2015; 24:878-885.</ref> | Supplementary prescribers can prescribe any medication, but it must be detailed in a written CMP. The CMP is created in partnership with the patient and a medical prescriber.<ref name="CSP 1" /> This means that although they are accountable for their decision to prescribe, they share accountability with the medical prescriber for the decision to put the medication in the CMP<ref name="CSP 1" />. In their nursing supplementary prescriber counterparts, this leads many doctors to feel that they have the ultimate responsibility for both the supplementary prescriber and patient. This can result in supplementary prescribers feeling subordinate, rather than in partnership with their medical prescriber.<ref>Creedon R, Byrne S, Kennedy J, McCarthy S. The impact of nurse prescribing on the clinical setting. British Journal of Nursing 2015; 24:878-885.</ref> | ||
| Line 58: | Line 47: | ||
=== Non-Prescribers === | === Non-Prescribers === | ||
The vast majority of physiotherapists globally are not prescribers and there appears to be debate regarding what their level of involvement in prescribing should be. In Australia, like in the UK, this is felt to be a legislative ‘grey’ area; different | The vast majority of physiotherapists globally are not prescribers and there appears to be debate regarding what their level of involvement in prescribing should be. In Australia, like in the UK, this is felt to be a legislative ‘grey’ area; different physiotherapists have different opinions on the extent of their scope regarding medicines.<ref>Morris JH, Grimmer K. Non-medical prescribing by physiotherapists: Issues reported in the current evidence. Manual Therapy 2014; 19:82-6.</ref> This is reflected in the guidance provided by professional bodies, as they feel an individual’s scope should vary depending on the depth of knowledge that they can demonstrate.<ref name="CSP 2" /> | ||
Studies investigating this have found that physiotherapists are frequently asked a wide variety of questions regarding NSAIDs and often feel pressured by patients to provide advice and recommendations regarding them. Almost all felt concerned that they lacked sufficient knowledge to confidently provide this, commensurate with their duty of care to their patients.<ref name="Kumar and Grimmer 2005">Kumar S, Grimmer K. Nonsteroidal anti-inflammatory drugs (NSAIDs) and physiotherapy management of musculoskeletal conditions: a professional minefield? Therapeutics and Clinical Risk Management 2005; 1:69-76.</ref> | Studies investigating this have found that physiotherapists are frequently asked a wide variety of questions regarding [[NSAIDs]] and often feel pressured by patients to provide advice and recommendations regarding them. Almost all felt concerned that they lacked sufficient knowledge to confidently provide this, commensurate with their duty of care to their patients.<ref name="Kumar and Grimmer 2005">Kumar S, Grimmer K. Nonsteroidal anti-inflammatory drugs (NSAIDs) and physiotherapy management of musculoskeletal conditions: a professional minefield? Therapeutics and Clinical Risk Management 2005; 1:69-76.</ref><br>There are a few very specific emergency events where a non-prescribing physiotherapist may aid the administration of drugs. If a patient brings in their medication its with instructions, in an emergency, you may administer it in accordance with these, as you are assisting them to take their prescribed medication. In an emergency, like any member of the public, a physiotherapist can also lawfully give certain life-saving POMs to someone acutely unwell without a prescription. The most important of these is adrenaline which is indicated for anaphylactic shock.<ref name="CSP 2" /> Below is a useful summary of who can prescribe and what they can prescribe<ref name="CSP 2" />:[[Image:Prescribing table.jpg|border|center]] | ||
<br>There are a few very specific emergency events where a non-prescribing physiotherapist may aid the administration of drugs. If a patient brings in their medication its with instructions, in an emergency, you may administer it in accordance with these, as you are assisting them to take their prescribed medication. In an emergency, like any member of the public, a physiotherapist can also lawfully give certain life-saving POMs to someone acutely unwell without a prescription. The most important of these is adrenaline which is indicated for anaphylactic shock.<ref name="CSP 2" /> Below is a useful summary of who can prescribe and what they can prescribe<ref name="CSP 2" />:[[Image:Prescribing table.jpg|border|center]] | |||
== Evidence Base For Prescribing Within Physiotherapy. == | == Evidence Base For Prescribing Within Physiotherapy. == | ||
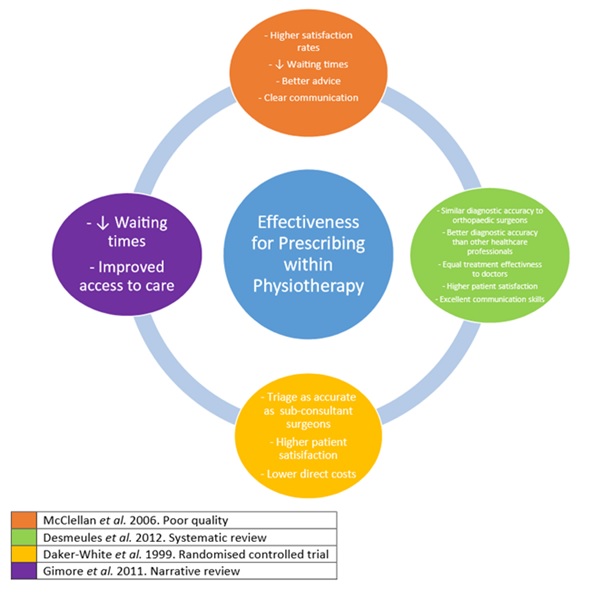
Overall, there is a lack of high quality evidence into the effectiveness of prescribing within physiotherapy, | Overall, there is a lack of high-quality evidence into the effectiveness of prescribing within physiotherapy, although there are many recognised benefits.<ref>Kersten P, McPherson K, Lattimer V, George S, Breton A, Ellis B. Physiotherapy extended scope of practice - who is doing what and why? Physiotherapy 2007; 93:235-42.</ref> Effective prescribing relies on the diagnostic accuracy of the prescriber. Physiotherapists in a range of MSK advanced scope roles have been shown through randomised controlled trials and systematic reviews to have equal diagnostic skill to orthopaedic surgeons and to be more accurate than other healthcare professionals, including non-orthopaedic physicians.<ref>Desmeules F, Roy JS, MacDermid JC, Champagne F, Hinse O, Woodhouse LJ. Advance practice physiotherapy in patients with musculoskeletal disorders: A systematic review. BMC Musculoskeletal Disorders 2012; 13:1-21.</ref><ref>Daker-White G, Carr AJ, Harvey I, Wollhead G, Bannister G, Nelson I, Kammerling M. A randomised controlled trial. Shifting the boundaries of doctors and physiotherapists in orthopaedic outpatient departments. Journal of Epidemiology and Community Health 1999; 53:643-50.</ref> In addition to this, the UK Department of Health for the year January 2005 to January 2006 reported that of the 60,000 medication incidents, none were related to physiotherapists.<ref>Morris JH, Grimmer K. Non-medical prescribing by physiotherapists: Issues reported in the current evidence. Manual Therapy 2014; 19:82-6.</ref>[[Image:Physio prescribing evidence.jpg|border|center]] | ||
== Traditional Physiotherapists Treatment of Pain == | == Traditional Physiotherapists Treatment of Pain == | ||
Physiotherapists are often referred patients whose main complaint is pain. It is therefore important to understand the nature, cause, pathology of pain and also whether it is acute or chronic. Below is a brief summary of pain, however, for a more detailed explanation of pain see | Physiotherapists are often referred patients whose main complaint is pain. It is therefore important to understand the nature, cause, pathology of pain and also whether it is acute or chronic. Below is a brief summary of pain, however, for a more detailed explanation of pain see [[Pain Mechanisms|Pain Mechanisms]]<br>[[Image:Grp6 pain2.jpg]] | ||
== Traditional Management Method == | |||
== Traditional Management | |||
To manage pain physiotherapists use a biopsychosocial approach, factoring in not just the biological but the psychological and social aspects that can influence a patient's perception of pain. We do this as evidence has shown that pain, catastrophising and social support have a statistically significant impact on future function<ref>Jensen MP, Moore MR, Bockow TB, Ehde DM, Engel JM. Psychosocial factors and adjustment to chronic pain in persons with physical disabilities: a systematic review. 2011 Arch Phys Med Rehabil</ref>. Recovery time may also be impacted by the belief the patient has on their recovery time.<ref>Ramond A, Bouton C, Richard I, Roquelaure Y, Baufreton C, Legrand E, et al. Psychosocial risk factors for chronic low back pain in primary care--a systematic review. Fam Pract 2011 Feb;28(1):12-21.</ref> | |||
<br>In Breivik et al.'s<ref name="Breivik et al 2006">Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. European journal of pain 2006;10(4):287-287</ref> study of pain in Europe it was found that 2/3rds of the population questioned were being treated either additionally or solely by non medicated means, including 30% for massage and 21% for physical therapy. Evidence suggests that GP care alone is not as effective as a combined approach of more exercise, education and traditional care<ref>Lin CC, Haas M, Maher CG, Machado LA, van Tulder MW. Cost-effectiveness of general practice care for low back pain: a systematic review. European Spine Journal 2011;20(7):1012-1023.</ref>. Currently physiotherapists use various evidence based means to support those with pain, this includes exercise therapy, cognitive behavioural therapy, acceptance and commitment therapy and potentially an increasing use medication to support their patients<ref>CSP. Physiotherapy works: Chronic pain. 15 April 2014; Available at: http://www.csp.org.uk/professional-union/practice/your-business/evidence-base/physiotherapy-works/chronic-pain. Accessed 1st November, 2015.</ref>. | <br>In Breivik et al.'s<ref name="Breivik et al 2006">Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. European journal of pain 2006;10(4):287-287</ref> study of pain in Europe it was found that 2/3rds of the population questioned were being treated either additionally or solely by non medicated means, including 30% for massage and 21% for physical therapy. Evidence suggests that GP care alone is not as effective as a combined approach of more exercise, education and traditional care<ref>Lin CC, Haas M, Maher CG, Machado LA, van Tulder MW. Cost-effectiveness of general practice care for low back pain: a systematic review. European Spine Journal 2011;20(7):1012-1023.</ref>. Currently physiotherapists use various evidence based means to support those with pain, this includes exercise therapy, cognitive behavioural therapy, acceptance and commitment therapy and potentially an increasing use medication to support their patients<ref>CSP. Physiotherapy works: Chronic pain. 15 April 2014; Available at: http://www.csp.org.uk/professional-union/practice/your-business/evidence-base/physiotherapy-works/chronic-pain. Accessed 1st November, 2015.</ref>. A Cochrane review agreed with these findings that for LBP physiotherapy treatment combined with physical conditioning and cognitive behaviour treatment, reduced the number of sick days for this group. Evidence has been shown that this physiotherapy treatment can improve quality of life and daily function <ref>Malmros B, Mortensen L, Jensen MB, Charles P. Positive effects of physiotherapy on chronic pain and performance in osteoporosis. Osteoporosis Int 1998;8(3):215-221.</ref>. Marienke et al.<ref>Van Middelkoop M, Rubinstein SM, Kuijpers T, Verhagen AP, Ostelo R, Koes BW, et al. A systematic review on the effectiveness of physical and rehabilitation interventions for chronic non-specific low back pain. European Spine Journal 2011;20(1):19-39.</ref> in a systematic review of the managment of chronic pain found that there was a general low quality of evidence, but exercise therapy, behavioural treatment and working with an MDT approach all had some evidence to support their use. Traditionally these methods are shown to have a good evidence base, but by adding the ability to presribe physiotherapists should have even more tools to support those in pain. | ||
== The Impact of Medication in Physiotherapy == | |||
Knowledge of drugs indications and side effects are important when determining whether a patient would benefit from them. If a patient has already been prescribed any of these drugs, management may vary e.g. MSK pain- a patient may be more tolerant of certain exercise because of their reduced pain, the physiotherapist would have an idea of how much to push the patient.<br>Drugs affecting mood/sleep tolerance also have an impact on rehabilitation, allowing specific treatment plans to be adjusted in a patient centred manner. | |||
< | The message should also be delivered to the patient that no drug works perfectly, and knowledge of their side effects should be made known. All physiotherapists should have sufficient competence to advise patients on where to obtain appropriate medication advice, as patients perceive physiotherapists to have up to date knowledge in this area<ref name="Kumar and Grimmer 2005" />. | ||
== | === Effect of Drugs on the Nervous System === | ||
Drugs interfere with the transmission of nerve impulses following noxious (harmful) stimulation, occurring at peripheral or central channels sites. The intention of administering analgesic drugs is to modulate the formation of noxious chemicals or to modulate the activation of neuronal channels transmitting noxious stimuli<ref name="Stein 2013">Stein C. Opioids, sensory systems and chronic pain. Eur J Pharmacol 2013;716(1):179-187.</ref>. | Drugs interfere with the transmission of nerve impulses following noxious (harmful) stimulation, occurring at peripheral or central channels sites. The intention of administering analgesic drugs is to modulate the formation of noxious chemicals or to modulate the activation of neuronal channels transmitting noxious stimuli<ref name="Stein 2013">Stein C. Opioids, sensory systems and chronic pain. Eur J Pharmacol 2013;716(1):179-187.</ref>. | ||
=== Drug Types Used for Chronic Pain === | |||
* Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) | |||
* Opioids | |||
* Antidepressants | |||
* Muscle relaxants | |||
* Serotonergic compounds, | |||
* Antiepileptics | |||
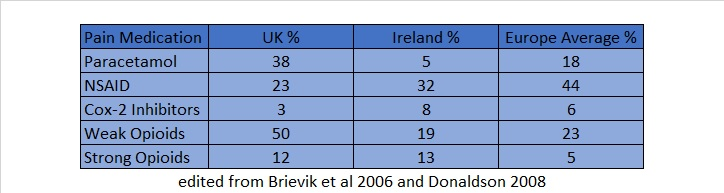
= | The following table highlights how countries place different focus on which drugs are the most effective for the treatment of pain<ref name="Breivik et al 2006" />. The most common drugs used in both Europe and in the UK were opioids and NSAIDs. Both have disadvantages that physiotherapists should be aware of. | ||
[[Image:Grp6_table_4.png]]<br> | |||
< | ==== NSAIDs ==== | ||
Taking [[NSAIDs]] causes general inhibition of target enzymes (cyclooxygenases I and II) which reduces inflammation, however, they can lead to major health issues affecting the GI tract, mucosal protection and gut motility<ref>Wehling M. Non-steroidal anti-inflammatory drug use in chronic pain conditions with special emphasis on the elderly and patients with relevant comorbidities: management and mitigation of risks and adverse effects. Eur J Clin Pharmacol 2014;70(10):1159-1172.</ref>. Side effects can lead to ulcers, renal failure, heart failure and atherosclerosis<ref name="Wehling 2014">Wehling M. Non-steroidal anti-inflammatory drug use in chronic pain conditions with special emphasis on the elderly and patients with relevant comorbidities: management and mitigation of risks and adverse effects. Eur J Clin Pharmacol 2014;70(10):1159-1172</ref>. These health risks are known but often neglected in practice. For these reasons, NSAIDs are not recommended for long term use in chronic pain, “alternative drugs, low-dose/short-term use, but especially nonpharmacologic approaches, such as physiotherapy, exercise, neurophysiologic measures, and local therapies”<ref name="Wehling 2014" /> should be priorities in management. They are contraindicated in patients with a history of peptic ulcer, myocardial infarction (MI), stroke or heart failure, or with impaired renal function<ref>Conaghan PG. A turbulent decade for NSAIDs: update on current concepts of classification, epidemiology, comparative efficacy, and toxicity. Rheumatol Int 2012;32(6):1491-1502.</ref>.Examples of NSAIDs commonly used to treat pain: | |||
* Ibuprofen | |||
* Naproxen | |||
==== Opioids ==== | |||
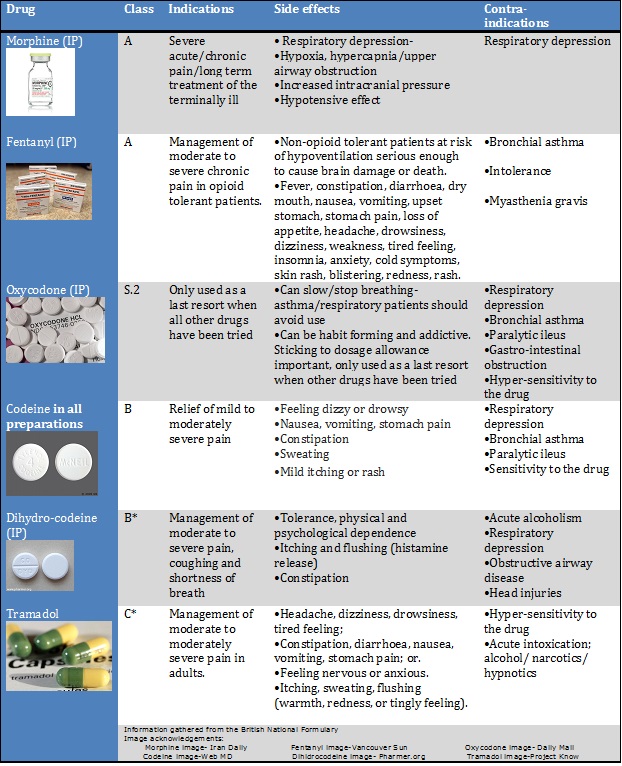
= | These drugs are classed as A, B or C. All controlled drugs for injection are bracketed under Class A <ref name="HCPC 2015">HCPC., Medicines and prescribing. Available from: http://www.hpc-uk.org/aboutregistration/medicinesandprescribing/ [Accessed 26th October 2015]</ref>. Opioids work by attaching to proteins known as opioid receptors in the brain and spinal cord to reduce the perception of pain. However, persistent use of these drugs can produce a tolerance whereby their effects decrease with repeated use of the same dose, so that increasing doses need to be used to gain the same effect. Abrupt cessation of opioid use can then lead to hyperplasia- a heightened sensitivity to pain | ||
<br> | [[Image:Opioid_Table.jpg|center]] Information gathered from the British National Formulary <br>Opioids are often used for: | ||
* Acute pain following surgery | |||
* Palliative care | |||
* Headaches | |||
* [[Fibromyalgia]] | |||
* [[Rheumatoid Arthritis|Rheumatoid arthritis]] | |||
* [[Cancer Pain|Cancer pain]] | |||
Addiction is also a problem with use of opioids, with overdoses and abuse of prescriptions becoming a health issue as people crave the relief and the feelings of euphoria associated with them<ref name="CDC 2012">Centers for Disease Control and Prevention (CDC). CDC grand rounds: prescription drug overdoses - a U.S. epidemic. MMWR Morb Mortal Wkly Rep 2012 Jan 13;61(1):10-13.</ref>. | |||
=== Efficacy of Using Opioids: Drug Therapy vs Alternative Treatment === | |||
Long-term pharmacological treatment of Chronic Non-Cancer Pain (CNCP) is highly disputed. Non-opioids (e.g. NSAIDs) can induce gastrointestinal ulcers, bleeding or cardiovascular complications<ref name="Trelle et al 2011">Trelle S, Reichenbach S, Wandel S, Hildebrand P, Tschannen B, Villiger PM, et al. Cardiovascular safety of non-steroidal anti-inflammatory drugs: network meta-analysis. BMJ 2011 Jan 11;342:c7086.</ref>. However, opioids can produce cognitive impairments, tolerance and addiction<ref name="Von Korff et al 2011">Von Korff M, Kolodny A, Deyo RA, Chou R. Long-term opioid therapy reconsidered. Ann Intern Med 2011;155(5):325-328</ref>. All patients taking opioids are also at risk of attaining withdrawal symptoms. | |||
A study by Reinecke ''et al''. <ref name="Reinecke et al 2015">Reinecke H, Weber C, Lange K, Simon M, Stein C, Sorgatz H. Analgesic efficacy of opioids in chronic pain: recent meta‐analyses. Br J Pharmacol 2015;172(2):324-333</ref> suggested that the treatment of chronic pain with opioids compared to traditional physiotherapy and psychological treatment was not significantly better in terms of pain intensity, functioning and quality of life. However, as each patient has individual benefits and side effects, efficacy of their treatment cannot be objectively predetermined. It is worth noting the study did not last longer than 3 months and there was significant dropout rates due in part to adverse side effects of the drugs. | A study by Reinecke ''et al''. <ref name="Reinecke et al 2015">Reinecke H, Weber C, Lange K, Simon M, Stein C, Sorgatz H. Analgesic efficacy of opioids in chronic pain: recent meta‐analyses. Br J Pharmacol 2015;172(2):324-333</ref> suggested that the treatment of chronic pain with opioids compared to traditional physiotherapy and psychological treatment was not significantly better in terms of pain intensity, functioning and quality of life. However, as each patient has individual benefits and side effects, efficacy of their treatment cannot be objectively predetermined. It is worth noting the study did not last longer than 3 months and there was significant dropout rates due in part to adverse side effects of the drugs. | ||
| Line 147: | Line 110: | ||
Randomised controlled trials with the same control e.g a placebo, and with the same outcome measure e.g. pain score, are not always directly comparable between individuals. There is also generally a lack of longitudinal studies demonstrating long-term effects of opioid usage for chronic pain patients. Guidelines therefore recommends medication should be maintained or halted based on individual monitoring over time. | Randomised controlled trials with the same control e.g a placebo, and with the same outcome measure e.g. pain score, are not always directly comparable between individuals. There is also generally a lack of longitudinal studies demonstrating long-term effects of opioid usage for chronic pain patients. Guidelines therefore recommends medication should be maintained or halted based on individual monitoring over time. | ||
== | == Conclusion == | ||
There are many pros and cons in the case for Physiotherapists prescribing medication for patients experiencing pain. However, more research needs to take place to ensure that these extended scope roles are supported. the fact is that independent prescribing has been introduced and physiotherapy as a profession has taken a huge step forward. The important thing now is for the profession to continue to move forward, adapt and improve. | |||
< | Critical reflection, and continuing to develop learning and skills are of vital importance at this point. A survey of nurse prescribing found that work based learning and training days were both effective ways at developing their prescribing knowledge, whilst 89% of the nurses surveyed felt they developed their prescribing skills since qualifying<ref name="Royal college of nursing 2013">Royal college of nursing. Nurse prescribing: Update 2013. http://journals.rcni.com/userimages/ContentEditor/1379936184622/Nurse-Prescribing.pdf (accessed 25th October 2015).</ref>. Aspects such as free supplements, guides, and online learning resources however were only used by few. Physiotherapists working in extended scope roles felt the support of the medical profession is the most crucial aspect underpinning the success of their role, as they were aware of their own limited scope of practice<ref>Dawson LJ, Ghazi F. The experience of physiotherapy extended scope practitioners in orthopaedic outpatient clinics. Physiotherapy. 2004 Dec 1;90(4):210-6.</ref>. Nevertheless, prescribing within physiotherapy offers a streamlined, and potentially very effective holistic intervention for patients. They, and other non-prescribers have been shown to decrease waiting times, improve patient satisfaction and offers physiotherapists a new and wider perspective on patient care. | ||
= References = | == References == | ||
<references /> | <references /> | ||
Latest revision as of 13:23, 7 September 2023
Top Contributors - Rosy Cuthbert, Mary Graham, Kim Jackson, Daniel Neilson, David Rossiter, Admin, 127.0.0.1, Evan Thomas, Michelle Lee, Claire Knott, Melissa Coetsee and Ines Musabyemariya
Introduction[edit | edit source]
With changing demographics, higher expectations and an increase in long term conditions [1] there is a heightened pressure and demand on the NHS. To meet these demands the roles within the NHS have had to change and expand. As recently as 2013, physiotherapists in England have been granted the right to independently prescribe, giving them the ability to prescribe drugs, including some controlled drugs. These prescriptions must be used “within the overarching framework of human movement, performance and function” [2]
It is important for physiotherapists to understand their scope and limitations to allow them to practice within this framework, as with this change we need to ensure that we remain working within our scope of practice to give the safest and best possible patient centred care. In a narrative review, Crane and Delany[3]comment that physiotherapists demonstrate an excellent ability to clinically reason and adapt to the changing needs of the societies they serve. The UK government has been convinced that prescribing is within physiotherapy’s scope because physiotherapists already possess the core skills that it requires.
The National Prescribing Centre[4] has produced a framework that applies to all prescribers, no matter what profession they come from. Below is a comparison of this framework it to the HCPC’s Standards of Proficiency for physiotherapists[5]:
Scope of Practice[edit | edit source]
Prescribing may appear a strange addition to a physiotherapist’s toolkit and outside the remit of the profession, which are defined by the Chartered Society of Physiotherapy[6] as anything within the 4 pillars of practice. These are:
- Massage
- Exercise and movement
- Electrotherapy
- Kindred methods of treatment
Any physiotherapist must not only work within their own personal scope of practice, but also within the scope of the profession.[7] Although prescribing is within the scope of the profession, like any skill, it only becomes part of an individual physiotherapist’s scope of practice when they become competent through training[8]. This means that before prescribing can be deemed a suitable addition to a physiotherapist’s skill set, they must already be an expert in the field they wish to apply it[9]. As a consequence, although the scope of prescribing within physiotherapy is very wide, it is limited to only an individual's clinical speciality.[8] This is a major difference from medical prescribing who may prescribe for any condition. The following pre-requisites are necessary so safely undertake the role of prescribing:
- Understand the legal context relevant to prescribing
- Understand pharmacodynamics, pharmacokinetics, pharmacology and therapeutics relevant to prescribing
- Understand different prescribing mechanisms
- Able to make prescribing decisions based on relevant physical examination assessment and history taking
- Able to communicate information about medicines and prescriptions clearly
- Able to monitor response to medications and modify or cease treatment as appropriate within scope of practice
- Able to undertake medication calculations
- Able to identify adverse medication reactions, interactions and take appropriate action
- Able to recognise medication error and respond appropriately
Once a physiotherapist decides that prescribing would be of benefit to their practice there are two types of prescriber they can become, based on their level of training supplementary prescribers or independent subscribers.
Supplementary Prescribers[edit | edit source]
Supplementary prescribers can prescribe any medication, but it must be detailed in a written CMP. The CMP is created in partnership with the patient and a medical prescriber.[8] This means that although they are accountable for their decision to prescribe, they share accountability with the medical prescriber for the decision to put the medication in the CMP[8]. In their nursing supplementary prescriber counterparts, this leads many doctors to feel that they have the ultimate responsibility for both the supplementary prescriber and patient. This can result in supplementary prescribers feeling subordinate, rather than in partnership with their medical prescriber.[10]
Supplementary prescribing is particularly suited to the care of chronic conditions, as once a CMP is in place, a medical prescriber can pass over management of a patient to the supplementary prescriber. Supplementary prescribers have expert knowledge of medications within their specialty, and can therefore modify or prescribe any drug detailed within the CMP, but have no influence on drugs that patients receive for other co-morbidities.[11] As experts in prescribing they may also provide detailed advice on any aspect of a medication for a patient, so long as they are used in their area of clinical specialty.[11]
Independent Prescribers[edit | edit source]
Independent prescribers share many features and core skills with supplementary prescribers.[9] However, as they prescribe completely autonomously and not in partnership with medical prescribers, they are wholly responsible for every aspect of the prescribing process.[8] They can actually prescribe fewer medicines than a supplementary prescriber, for example, being able to prescribe only seven controlled drugs:[8]
- Diazepam
- Dihydrocodeine
- Lorazepam
- Morphine
- Oxycodone
- Temazepam
- Fentanyl
Non-Prescribers[edit | edit source]
The vast majority of physiotherapists globally are not prescribers and there appears to be debate regarding what their level of involvement in prescribing should be. In Australia, like in the UK, this is felt to be a legislative ‘grey’ area; different physiotherapists have different opinions on the extent of their scope regarding medicines.[12] This is reflected in the guidance provided by professional bodies, as they feel an individual’s scope should vary depending on the depth of knowledge that they can demonstrate.[11]
Studies investigating this have found that physiotherapists are frequently asked a wide variety of questions regarding NSAIDs and often feel pressured by patients to provide advice and recommendations regarding them. Almost all felt concerned that they lacked sufficient knowledge to confidently provide this, commensurate with their duty of care to their patients.[13]
There are a few very specific emergency events where a non-prescribing physiotherapist may aid the administration of drugs. If a patient brings in their medication its with instructions, in an emergency, you may administer it in accordance with these, as you are assisting them to take their prescribed medication. In an emergency, like any member of the public, a physiotherapist can also lawfully give certain life-saving POMs to someone acutely unwell without a prescription. The most important of these is adrenaline which is indicated for anaphylactic shock.[11] Below is a useful summary of who can prescribe and what they can prescribe[11]:
Evidence Base For Prescribing Within Physiotherapy.[edit | edit source]
Overall, there is a lack of high-quality evidence into the effectiveness of prescribing within physiotherapy, although there are many recognised benefits.[14] Effective prescribing relies on the diagnostic accuracy of the prescriber. Physiotherapists in a range of MSK advanced scope roles have been shown through randomised controlled trials and systematic reviews to have equal diagnostic skill to orthopaedic surgeons and to be more accurate than other healthcare professionals, including non-orthopaedic physicians.[15][16] In addition to this, the UK Department of Health for the year January 2005 to January 2006 reported that of the 60,000 medication incidents, none were related to physiotherapists.[17]
Traditional Physiotherapists Treatment of Pain[edit | edit source]
Physiotherapists are often referred patients whose main complaint is pain. It is therefore important to understand the nature, cause, pathology of pain and also whether it is acute or chronic. Below is a brief summary of pain, however, for a more detailed explanation of pain see Pain Mechanisms
Traditional Management Method[edit | edit source]
To manage pain physiotherapists use a biopsychosocial approach, factoring in not just the biological but the psychological and social aspects that can influence a patient's perception of pain. We do this as evidence has shown that pain, catastrophising and social support have a statistically significant impact on future function[18]. Recovery time may also be impacted by the belief the patient has on their recovery time.[19]
In Breivik et al.'s[20] study of pain in Europe it was found that 2/3rds of the population questioned were being treated either additionally or solely by non medicated means, including 30% for massage and 21% for physical therapy. Evidence suggests that GP care alone is not as effective as a combined approach of more exercise, education and traditional care[21]. Currently physiotherapists use various evidence based means to support those with pain, this includes exercise therapy, cognitive behavioural therapy, acceptance and commitment therapy and potentially an increasing use medication to support their patients[22]. A Cochrane review agreed with these findings that for LBP physiotherapy treatment combined with physical conditioning and cognitive behaviour treatment, reduced the number of sick days for this group. Evidence has been shown that this physiotherapy treatment can improve quality of life and daily function [23]. Marienke et al.[24] in a systematic review of the managment of chronic pain found that there was a general low quality of evidence, but exercise therapy, behavioural treatment and working with an MDT approach all had some evidence to support their use. Traditionally these methods are shown to have a good evidence base, but by adding the ability to presribe physiotherapists should have even more tools to support those in pain.
The Impact of Medication in Physiotherapy[edit | edit source]
Knowledge of drugs indications and side effects are important when determining whether a patient would benefit from them. If a patient has already been prescribed any of these drugs, management may vary e.g. MSK pain- a patient may be more tolerant of certain exercise because of their reduced pain, the physiotherapist would have an idea of how much to push the patient.
Drugs affecting mood/sleep tolerance also have an impact on rehabilitation, allowing specific treatment plans to be adjusted in a patient centred manner.
The message should also be delivered to the patient that no drug works perfectly, and knowledge of their side effects should be made known. All physiotherapists should have sufficient competence to advise patients on where to obtain appropriate medication advice, as patients perceive physiotherapists to have up to date knowledge in this area[13].
Effect of Drugs on the Nervous System[edit | edit source]
Drugs interfere with the transmission of nerve impulses following noxious (harmful) stimulation, occurring at peripheral or central channels sites. The intention of administering analgesic drugs is to modulate the formation of noxious chemicals or to modulate the activation of neuronal channels transmitting noxious stimuli[25].
Drug Types Used for Chronic Pain[edit | edit source]
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
- Opioids
- Antidepressants
- Muscle relaxants
- Serotonergic compounds,
- Antiepileptics
The following table highlights how countries place different focus on which drugs are the most effective for the treatment of pain[20]. The most common drugs used in both Europe and in the UK were opioids and NSAIDs. Both have disadvantages that physiotherapists should be aware of.
NSAIDs[edit | edit source]
Taking NSAIDs causes general inhibition of target enzymes (cyclooxygenases I and II) which reduces inflammation, however, they can lead to major health issues affecting the GI tract, mucosal protection and gut motility[26]. Side effects can lead to ulcers, renal failure, heart failure and atherosclerosis[27]. These health risks are known but often neglected in practice. For these reasons, NSAIDs are not recommended for long term use in chronic pain, “alternative drugs, low-dose/short-term use, but especially nonpharmacologic approaches, such as physiotherapy, exercise, neurophysiologic measures, and local therapies”[27] should be priorities in management. They are contraindicated in patients with a history of peptic ulcer, myocardial infarction (MI), stroke or heart failure, or with impaired renal function[28].Examples of NSAIDs commonly used to treat pain:
- Ibuprofen
- Naproxen
Opioids[edit | edit source]
These drugs are classed as A, B or C. All controlled drugs for injection are bracketed under Class A [29]. Opioids work by attaching to proteins known as opioid receptors in the brain and spinal cord to reduce the perception of pain. However, persistent use of these drugs can produce a tolerance whereby their effects decrease with repeated use of the same dose, so that increasing doses need to be used to gain the same effect. Abrupt cessation of opioid use can then lead to hyperplasia- a heightened sensitivity to pain
Information gathered from the British National Formulary
Opioids are often used for:
- Acute pain following surgery
- Palliative care
- Headaches
- Fibromyalgia
- Rheumatoid arthritis
- Cancer pain
Addiction is also a problem with use of opioids, with overdoses and abuse of prescriptions becoming a health issue as people crave the relief and the feelings of euphoria associated with them[30].
Efficacy of Using Opioids: Drug Therapy vs Alternative Treatment[edit | edit source]
Long-term pharmacological treatment of Chronic Non-Cancer Pain (CNCP) is highly disputed. Non-opioids (e.g. NSAIDs) can induce gastrointestinal ulcers, bleeding or cardiovascular complications[31]. However, opioids can produce cognitive impairments, tolerance and addiction[32]. All patients taking opioids are also at risk of attaining withdrawal symptoms.
A study by Reinecke et al. [33] suggested that the treatment of chronic pain with opioids compared to traditional physiotherapy and psychological treatment was not significantly better in terms of pain intensity, functioning and quality of life. However, as each patient has individual benefits and side effects, efficacy of their treatment cannot be objectively predetermined. It is worth noting the study did not last longer than 3 months and there was significant dropout rates due in part to adverse side effects of the drugs.
It is difficult to improve chronic pain through the use of opioids, because psychological and learning variables play a large part in the diagnosis; “learning, conditioning, cognition, affect, emotions, social and cultural influences, financial aspects of the health care system, litigation and others” have major influences[25]. Opioids may inhibit nociceptive pain, but have little impact on these factors. Prescribing opioids may therefore have a major impact on the way physiotherapist’s treat chronic pain, as a psychosocial approach focussing on these factors has traditionally been a mainstay of physiotherapy treatment
Randomised controlled trials with the same control e.g a placebo, and with the same outcome measure e.g. pain score, are not always directly comparable between individuals. There is also generally a lack of longitudinal studies demonstrating long-term effects of opioid usage for chronic pain patients. Guidelines therefore recommends medication should be maintained or halted based on individual monitoring over time.
Conclusion[edit | edit source]
There are many pros and cons in the case for Physiotherapists prescribing medication for patients experiencing pain. However, more research needs to take place to ensure that these extended scope roles are supported. the fact is that independent prescribing has been introduced and physiotherapy as a profession has taken a huge step forward. The important thing now is for the profession to continue to move forward, adapt and improve.
Critical reflection, and continuing to develop learning and skills are of vital importance at this point. A survey of nurse prescribing found that work based learning and training days were both effective ways at developing their prescribing knowledge, whilst 89% of the nurses surveyed felt they developed their prescribing skills since qualifying[34]. Aspects such as free supplements, guides, and online learning resources however were only used by few. Physiotherapists working in extended scope roles felt the support of the medical profession is the most crucial aspect underpinning the success of their role, as they were aware of their own limited scope of practice[35]. Nevertheless, prescribing within physiotherapy offers a streamlined, and potentially very effective holistic intervention for patients. They, and other non-prescribers have been shown to decrease waiting times, improve patient satisfaction and offers physiotherapists a new and wider perspective on patient care.
References[edit | edit source]
- ↑ Department of Health. Long-term conditions compendium of information: 3rd edition. 2012; Available at: https://www.gov.uk/government/publications/long-term-conditions-compendium-of-information-third-edition. Accessed 5th November, 2015.
- ↑ NHS England Publications. Frequently Asked Questions: Independent prescribing by physiotherapists and podiatrists Publications Gateway Reference 00364 . 2013; Available at:https://www.england.nhs.uk/wp-content/uploads/2013/08/faqs-ippp1.pdf. Accessed 15th November, 2015.
- ↑ Crane J, Delany C. Physiotherapists in emergency departments: responsibilities, accountability and education. Physiotherapy 2013; 99:95-100.
- ↑ National Prescribing Centre., A single competency framework for all prescribers. http://www.webarchive.org.uk/wayback/archive/20140627112901/http://www.npc.nhs.uk/improving_safety/improving_quality/resources/single_comp_framework_v2.pdf (accessed 6 Nov 2015)
- ↑ Health and Care Professions Council. Standards of proficiency: Physiotherapists. http://www.hcpc-uk.co.uk/assets/documents/10000DBCStandards_of_Proficiency_Physiotherapists.pdf (accessed 11 Nov 2015).
- ↑ Chartered Society of Physiotherapy. Medicines, prescribing and physiotherapy. file:///C:/Users/user/Downloads/csp_pd019_medicines_prescribing_physiotherapy_2013_0.pdf (accessed 25 Oct 2015)
- ↑ Chartered Society of Physiotherapy. Practice guidance for physiotherapist supplementary and/or independent prescribers in the safe use of medicines. file:///C:/Users/user/Downloads/csp_pd026_practice_guidance_prescribers_aug2013_0_0.pdf (accessed 25 Oct 2015)
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 Chartered Society of Physiotherapy. Medicines, prescribing and physiotherapy. file:///C:/Users/user/Downloads/csp_pd019_medicines_prescribing_physiotherapy_2013_0.pdf (accessed 25 Oct 2015)
- ↑ 9.0 9.1 National Prescribing Centre., A single competency framework for all prescribers. http://www.webarchive.org.uk/wayback/archive/20140627112901/http://www.npc.nhs.uk/improving_safety/improving_quality/resources/single_comp_framework_v2.pdf (accessed 6 Nov 2015)
- ↑ Creedon R, Byrne S, Kennedy J, McCarthy S. The impact of nurse prescribing on the clinical setting. British Journal of Nursing 2015; 24:878-885.
- ↑ 11.0 11.1 11.2 11.3 11.4 Chartered Society of Physiotherapy. Practice guidance for physiotherapist supplementary and/or independent prescribers in the safe use of medicines. file:///C:/Users/user/Downloads/csp_pd026_practice_guidance_prescribers_aug2013_0_0.pdf (accessed 25 Oct 2015)
- ↑ Morris JH, Grimmer K. Non-medical prescribing by physiotherapists: Issues reported in the current evidence. Manual Therapy 2014; 19:82-6.
- ↑ 13.0 13.1 Kumar S, Grimmer K. Nonsteroidal anti-inflammatory drugs (NSAIDs) and physiotherapy management of musculoskeletal conditions: a professional minefield? Therapeutics and Clinical Risk Management 2005; 1:69-76.
- ↑ Kersten P, McPherson K, Lattimer V, George S, Breton A, Ellis B. Physiotherapy extended scope of practice - who is doing what and why? Physiotherapy 2007; 93:235-42.
- ↑ Desmeules F, Roy JS, MacDermid JC, Champagne F, Hinse O, Woodhouse LJ. Advance practice physiotherapy in patients with musculoskeletal disorders: A systematic review. BMC Musculoskeletal Disorders 2012; 13:1-21.
- ↑ Daker-White G, Carr AJ, Harvey I, Wollhead G, Bannister G, Nelson I, Kammerling M. A randomised controlled trial. Shifting the boundaries of doctors and physiotherapists in orthopaedic outpatient departments. Journal of Epidemiology and Community Health 1999; 53:643-50.
- ↑ Morris JH, Grimmer K. Non-medical prescribing by physiotherapists: Issues reported in the current evidence. Manual Therapy 2014; 19:82-6.
- ↑ Jensen MP, Moore MR, Bockow TB, Ehde DM, Engel JM. Psychosocial factors and adjustment to chronic pain in persons with physical disabilities: a systematic review. 2011 Arch Phys Med Rehabil
- ↑ Ramond A, Bouton C, Richard I, Roquelaure Y, Baufreton C, Legrand E, et al. Psychosocial risk factors for chronic low back pain in primary care--a systematic review. Fam Pract 2011 Feb;28(1):12-21.
- ↑ 20.0 20.1 Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. European journal of pain 2006;10(4):287-287
- ↑ Lin CC, Haas M, Maher CG, Machado LA, van Tulder MW. Cost-effectiveness of general practice care for low back pain: a systematic review. European Spine Journal 2011;20(7):1012-1023.
- ↑ CSP. Physiotherapy works: Chronic pain. 15 April 2014; Available at: http://www.csp.org.uk/professional-union/practice/your-business/evidence-base/physiotherapy-works/chronic-pain. Accessed 1st November, 2015.
- ↑ Malmros B, Mortensen L, Jensen MB, Charles P. Positive effects of physiotherapy on chronic pain and performance in osteoporosis. Osteoporosis Int 1998;8(3):215-221.
- ↑ Van Middelkoop M, Rubinstein SM, Kuijpers T, Verhagen AP, Ostelo R, Koes BW, et al. A systematic review on the effectiveness of physical and rehabilitation interventions for chronic non-specific low back pain. European Spine Journal 2011;20(1):19-39.
- ↑ 25.0 25.1 Stein C. Opioids, sensory systems and chronic pain. Eur J Pharmacol 2013;716(1):179-187.
- ↑ Wehling M. Non-steroidal anti-inflammatory drug use in chronic pain conditions with special emphasis on the elderly and patients with relevant comorbidities: management and mitigation of risks and adverse effects. Eur J Clin Pharmacol 2014;70(10):1159-1172.
- ↑ 27.0 27.1 Wehling M. Non-steroidal anti-inflammatory drug use in chronic pain conditions with special emphasis on the elderly and patients with relevant comorbidities: management and mitigation of risks and adverse effects. Eur J Clin Pharmacol 2014;70(10):1159-1172
- ↑ Conaghan PG. A turbulent decade for NSAIDs: update on current concepts of classification, epidemiology, comparative efficacy, and toxicity. Rheumatol Int 2012;32(6):1491-1502.
- ↑ HCPC., Medicines and prescribing. Available from: http://www.hpc-uk.org/aboutregistration/medicinesandprescribing/ [Accessed 26th October 2015]
- ↑ Centers for Disease Control and Prevention (CDC). CDC grand rounds: prescription drug overdoses - a U.S. epidemic. MMWR Morb Mortal Wkly Rep 2012 Jan 13;61(1):10-13.
- ↑ Trelle S, Reichenbach S, Wandel S, Hildebrand P, Tschannen B, Villiger PM, et al. Cardiovascular safety of non-steroidal anti-inflammatory drugs: network meta-analysis. BMJ 2011 Jan 11;342:c7086.
- ↑ Von Korff M, Kolodny A, Deyo RA, Chou R. Long-term opioid therapy reconsidered. Ann Intern Med 2011;155(5):325-328
- ↑ Reinecke H, Weber C, Lange K, Simon M, Stein C, Sorgatz H. Analgesic efficacy of opioids in chronic pain: recent meta‐analyses. Br J Pharmacol 2015;172(2):324-333
- ↑ Royal college of nursing. Nurse prescribing: Update 2013. http://journals.rcni.com/userimages/ContentEditor/1379936184622/Nurse-Prescribing.pdf (accessed 25th October 2015).
- ↑ Dawson LJ, Ghazi F. The experience of physiotherapy extended scope practitioners in orthopaedic outpatient clinics. Physiotherapy. 2004 Dec 1;90(4):210-6.