Pelvic Floor Distress Inventory (PFDI - 20): Difference between revisions
Kirsten Ryan (talk | contribs) No edit summary |
Kim Jackson (talk | contribs) m (Text replacement - "[[Incontinence|" to "[[Urinary Incontinence|") |
||
| (32 intermediate revisions by 10 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor '''- | '''Original Editor '''- [[User:Kirsten Ryan|Kirsten Ryan]] | ||
''' | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Objective | == Objective == | ||
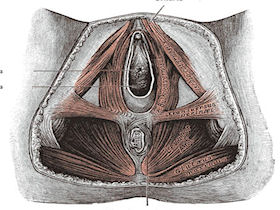
[[Image:Pelvic floor.jpg|right]] | |||
== | The Pelvic Floor Distress Inventory Questionnaire-20 (PFDI-20) is the short-form version of the Pelvic Floor Distress Inventory (PFDI).<ref name="Barber" /> Similar to the [[Pelvic Floor Impact Questionnaire (PFIQ - 7)|PFIQ-7]], it is a health-related quality of life questionnaire for women with pelvic floor conditions to fill out.<ref name="Barber" /> The PFDI-20 is comprised of 3 scales, which include the Urinary Distress Inventory-6 (UDI-6), Pelvic Organ Prolapse Distress Inventory-6 (POPDI-6), and the Colorectal-Anal Distress Inventory-8 (CRADI-8).<ref name="Barber" /> | ||
Women with disorders of the pelvic floor including urinary incontinence, pelvic organ prolapse, and fecal incontinence.<ref name="Barber">Barber MD, Walters MD, Bump RC. Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 adn PFIQ-7). Am J Obstet Gynecol 2005;193:103-113.</ref> | == Intended Population == | ||
Women over the age of 18 with disorders of the pelvic floor including urinary [[Urinary Incontinence|incontinence]], [[Pelvic Organ Prolapse|pelvic organ prolapse]], and [[Low Back Pain and Pelvic Floor Disorders|fecal incontinence]].<ref name="Barber">Barber MD, Walters MD, Bump RC. Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 adn PFIQ-7). Am J Obstet Gynecol 2005;193:103-113.</ref> | |||
== Method of Use == | == Method of Use == | ||
Since it is comprised of the UDI-6, POPDI-6, and the CRADI-8, the PFDI-20 includes 20 questions.<ref name="Barber" /> Each question begins with a "yes" or "no" response. If "yes," the patient must indicate how much bowl, bladder, or pelvic symptoms have been bothering them in the past 3 months on a 4-point scale that ranges from "not at all" (0) to "quite a bit" (4).<ref name="Barber" /> The scale scores are found individually by calculating the mean value of their corresponding questions and then multiplying by 25 to obtain a value that ranges from 0 to 100.<ref name="Barber" /> The sum of the 3 scales are added together to get the PFDI-20 summary score, which ranges from 0 to 300.<ref name="Barber" /> | |||
== Evidence == | == Evidence == | ||
=== Correlation === | |||
Correlation, represented by r, ranges from -1.0 to +1.0. If the r value is 0 that means there is no correlation. If the r value is close to -1.0 that means that both values will decrease linearly. If the r value is close to +1.0 that means that both values will increase linearly. | |||
Correlation of the short-form versions with the long-form versions:[[Pelvic Floor Impact Questionnaire (PFIQ - 7)|[1]]] | |||
* UDI-6 r=0.86<ref name="Barber" /> | |||
* POPDI-6 r=0.92<ref name="Barber" /> | |||
* CRADI-8 r=0.93<ref name="Barber" /> | |||
=== Reliability === | === Reliability === | ||
The | The test-retest reliability, represented by intraclass correlation coefficients (ICC):[[Pelvic Floor Impact Questionnaire (PFIQ - 7)|[1]]] | ||
* PFDI-20 ICC=0.93<ref name="Barber" /> | |||
* UDI-6 ICC=0.82<ref name="Barber" /> | |||
* POPDI-6 ICC=0.91<ref name="Barber" /> | |||
* CRADI-8 ICC=0.84<ref name="Barber" /> | |||
=== Validity === | === Validity === | ||
The PFDI-20 demonstrates construct validity as it demonstrates a significant association with appropriate measures of symptom severity and pelvic floor diagnoses.<ref name="Barber" /> | The PFDI-20 demonstrates construct validity as it demonstrates a significant association with appropriate measures of symptom severity and pelvic floor diagnoses.<ref name="Barber" /> | ||
=== Responsiveness === | === Responsiveness === | ||
Each of the 3 scales of the PFDI-20 demonstrated moderate to excellent responsiveness with effect size and standardized response mean values ranging from .70 to 1.28. The sensitivity of the PFDI-20 as a whole was excellent with an effect size of 1.48 P < .0001 and standardized response mean of 1.09 P < .0001. The ability of the PFDI-20 to discriminate between subjects who indicated that they were "worse" after surgery from those who indicated they were "better" was excellent with c-statistic of .95.<ref name="Barber" /> | Each of the 3 scales of the PFDI-20 demonstrated moderate to excellent responsiveness with effect size and standardized response mean values ranging from 0.70 to 1.28.<ref name="Barber" /> The sensitivity of the PFDI-20 as a whole was excellent with an effect size of 1.48 P < .0001 and standardized response mean of 1.09 P < .0001.<ref name="Barber" /> The ability of the PFDI-20 to discriminate between subjects who indicated that they were "worse" after surgery from those who indicated they were "better" was excellent with c-statistic of .95.<ref name="Barber" /> | ||
=== Clinically Meaningful Change === | |||
At the time of creation, the clinically meaningful change in quality of life (MCID)<ref name="crosby">Crosby RD, Kolotkin RL, Williams GR. Defining clinically meaningful change in health-related quality of life. Journal of clinical epidemiology. 2003 May 1;56(5):395-407.</ref> needed to be studied in larger populations.<ref name="Barber" /> Studies have found minimal importance changes (MIC) ranging from 23 to 45.<ref name="Barber" /><ref>Gelhorn HL, Coyne KS, Sikirica V, Gauld J, Murphy M. Psychometric evaluation of health-related quality-of-life measures after pelvic organ prolapse surgery. Female pelvic medicine & reconstructive surgery. 2012 Jul 1;18(4):221-6.</ref><ref>Utomo E, Blok BF, Steensma AB, Korfage IJ. Validation of the pelvic floor distress inventory (PFDI-20) and pelvic floor impact questionnaire (PFIQ-7) in a Dutch population. International urogynecology journal. 2014 Apr 1;25(4):531-44.</ref> For example, in their small sample size, Barber and colleagues (2004)<ref name="Barber" /> found a change in the summary score of 45 points or more to be meaningful after surgery.<ref name="Barber" /> However, it is important to consider that patients undergoing surgery also generally have higher scores at baseline.<ref name=":0">Wiegersma M, Panman CM, Berger MY, De Vet HC, Kollen BJ, Dekker JH. Minimal important change in the pelvic floor distress inventory-20 among women opting for conservative prolapse treatment. American journal of obstetrics and gynecology. 2017 Apr 1;216(4):397-e1.</ref> | |||
More recently, Wiegersma and colleagues (2017)<ref name=":0" /> aimed to determine the MIC in women undergoing conservative pelvic organ prolapse treatments for mild symptoms.<ref name=":0" /> They found that an improvement of 13.5 points to be helpful when evaluating the effects of conservative treatment strategies.<ref name=":0" /> | |||
=== Miscellaneous | === Miscellaneous === | ||
The strength of the PFDI-20 is that it is a short form that gives a comprehensive assessment of the effect of pelvic floor disorders on the quality of life of women, rather than assessing just one aspect of pelvic floor function such as urinary incontinence. A more generic quality-of-life form as the SF-36 has demonstrated poor responsiveness in patients undergoing treatment for urinary incontinence. In these patient populations, it may be important to use both a generic quality-of-life instrument and a condition-specific instrument that has demonstrated responsiveness. The PFDI-20 is easy to use in both clinical and research settings.<ref name="Barber" /> | The strength of the PFDI-20 is that it is a short form that gives a comprehensive assessment of the effect of pelvic floor disorders on the quality of life of women, rather than assessing just one aspect of pelvic floor function such as urinary incontinence. A more generic quality-of-life form as the SF-36 has demonstrated poor responsiveness in patients undergoing treatment for urinary incontinence. In these patient populations, it may be important to use both a generic quality-of-life instrument and a condition-specific instrument that has demonstrated responsiveness. The PFDI-20 is easy to use in both clinical and research settings.<ref name="Barber" /> | ||
== Links == | == Links == | ||
*[https://www.sralab.org/sites/default/files/2017-06/WUC_Pelvic_Floor_Questionnaire.pdf Overview of PFDI-20 on the Rehabilitation Measures Database.] | |||
*[http://www.womenshealthapta.org/wp-content/uploads/2013/12/PFDI-PFIQ.pdf Paper by Barber et al 2005 describing the development of the PFIQ-7] | |||
== | == References == | ||
< | <references /> | ||
[[Category:Outcome_Measures]] | |||
[[Category:Pelvic Health]] | |||
[[Category:Pelvis]] | |||
[[Category:Womens_Health]] | |||
[[Category:Mens_Health]] | |||
[[Category:Pelvis]] | |||
[[Category:Pelvis - Outcome Measures]] | |||
Latest revision as of 10:49, 24 May 2022
Original Editor - Kirsten Ryan
Top Contributors - Kirsten Ryan, Admin, Michelle Walsh, Laura Ritchie, Kim Jackson, Tony Lowe, WikiSysop, Oyemi Sillo, Nicole Hills and Evan Thomas
Objective[edit | edit source]
The Pelvic Floor Distress Inventory Questionnaire-20 (PFDI-20) is the short-form version of the Pelvic Floor Distress Inventory (PFDI).[1] Similar to the PFIQ-7, it is a health-related quality of life questionnaire for women with pelvic floor conditions to fill out.[1] The PFDI-20 is comprised of 3 scales, which include the Urinary Distress Inventory-6 (UDI-6), Pelvic Organ Prolapse Distress Inventory-6 (POPDI-6), and the Colorectal-Anal Distress Inventory-8 (CRADI-8).[1]
Intended Population[edit | edit source]
Women over the age of 18 with disorders of the pelvic floor including urinary incontinence, pelvic organ prolapse, and fecal incontinence.[1]
Method of Use[edit | edit source]
Since it is comprised of the UDI-6, POPDI-6, and the CRADI-8, the PFDI-20 includes 20 questions.[1] Each question begins with a "yes" or "no" response. If "yes," the patient must indicate how much bowl, bladder, or pelvic symptoms have been bothering them in the past 3 months on a 4-point scale that ranges from "not at all" (0) to "quite a bit" (4).[1] The scale scores are found individually by calculating the mean value of their corresponding questions and then multiplying by 25 to obtain a value that ranges from 0 to 100.[1] The sum of the 3 scales are added together to get the PFDI-20 summary score, which ranges from 0 to 300.[1]
Evidence[edit | edit source]
Correlation[edit | edit source]
Correlation, represented by r, ranges from -1.0 to +1.0. If the r value is 0 that means there is no correlation. If the r value is close to -1.0 that means that both values will decrease linearly. If the r value is close to +1.0 that means that both values will increase linearly.
Correlation of the short-form versions with the long-form versions:[1]
Reliability[edit | edit source]
The test-retest reliability, represented by intraclass correlation coefficients (ICC):[1]
Validity[edit | edit source]
The PFDI-20 demonstrates construct validity as it demonstrates a significant association with appropriate measures of symptom severity and pelvic floor diagnoses.[1]
Responsiveness[edit | edit source]
Each of the 3 scales of the PFDI-20 demonstrated moderate to excellent responsiveness with effect size and standardized response mean values ranging from 0.70 to 1.28.[1] The sensitivity of the PFDI-20 as a whole was excellent with an effect size of 1.48 P < .0001 and standardized response mean of 1.09 P < .0001.[1] The ability of the PFDI-20 to discriminate between subjects who indicated that they were "worse" after surgery from those who indicated they were "better" was excellent with c-statistic of .95.[1]
Clinically Meaningful Change[edit | edit source]
At the time of creation, the clinically meaningful change in quality of life (MCID)[2] needed to be studied in larger populations.[1] Studies have found minimal importance changes (MIC) ranging from 23 to 45.[1][3][4] For example, in their small sample size, Barber and colleagues (2004)[1] found a change in the summary score of 45 points or more to be meaningful after surgery.[1] However, it is important to consider that patients undergoing surgery also generally have higher scores at baseline.[5]
More recently, Wiegersma and colleagues (2017)[5] aimed to determine the MIC in women undergoing conservative pelvic organ prolapse treatments for mild symptoms.[5] They found that an improvement of 13.5 points to be helpful when evaluating the effects of conservative treatment strategies.[5]
Miscellaneous[edit | edit source]
The strength of the PFDI-20 is that it is a short form that gives a comprehensive assessment of the effect of pelvic floor disorders on the quality of life of women, rather than assessing just one aspect of pelvic floor function such as urinary incontinence. A more generic quality-of-life form as the SF-36 has demonstrated poor responsiveness in patients undergoing treatment for urinary incontinence. In these patient populations, it may be important to use both a generic quality-of-life instrument and a condition-specific instrument that has demonstrated responsiveness. The PFDI-20 is easy to use in both clinical and research settings.[1]
Links[edit | edit source]
- Overview of PFDI-20 on the Rehabilitation Measures Database.
- Paper by Barber et al 2005 describing the development of the PFIQ-7
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 1.22 1.23 Barber MD, Walters MD, Bump RC. Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 adn PFIQ-7). Am J Obstet Gynecol 2005;193:103-113.
- ↑ Crosby RD, Kolotkin RL, Williams GR. Defining clinically meaningful change in health-related quality of life. Journal of clinical epidemiology. 2003 May 1;56(5):395-407.
- ↑ Gelhorn HL, Coyne KS, Sikirica V, Gauld J, Murphy M. Psychometric evaluation of health-related quality-of-life measures after pelvic organ prolapse surgery. Female pelvic medicine & reconstructive surgery. 2012 Jul 1;18(4):221-6.
- ↑ Utomo E, Blok BF, Steensma AB, Korfage IJ. Validation of the pelvic floor distress inventory (PFDI-20) and pelvic floor impact questionnaire (PFIQ-7) in a Dutch population. International urogynecology journal. 2014 Apr 1;25(4):531-44.
- ↑ 5.0 5.1 5.2 5.3 Wiegersma M, Panman CM, Berger MY, De Vet HC, Kollen BJ, Dekker JH. Minimal important change in the pelvic floor distress inventory-20 among women opting for conservative prolapse treatment. American journal of obstetrics and gynecology. 2017 Apr 1;216(4):397-e1.