Patellofemoral Joint: Difference between revisions
(Edited the articulating surfaces, muscles, kinematics and kinitics.) |
mNo edit summary |
||
| Line 58: | Line 58: | ||
Compression at the patellofemoral joint:<ref name="p1" /> | Compression at the patellofemoral joint:<ref name="p1" /> | ||
{| width="300" border="1" align="left" cellpadding="1" cellspacing="1" | {| class="wikitable sortable" width="300" border="1" align="left" cellpadding="1" cellspacing="1" | ||
|- | |- | ||
! scope="col" | Activity | ! scope="col" | Activity | ||
Revision as of 18:57, 23 May 2020
Original Editor - Elvira Muhic
Lead Editors - Elvira Muhic, Kim Jackson, Lilian Ashraf, WikiSysop, Ahmed Essam, 127.0.0.1, Admin, Rachael Lowe, Evan Thomas, Michelle Lee, Vidya Acharya, Rucha Gadgil, Jess Bell and Robin Tacchetti
Description[edit | edit source]
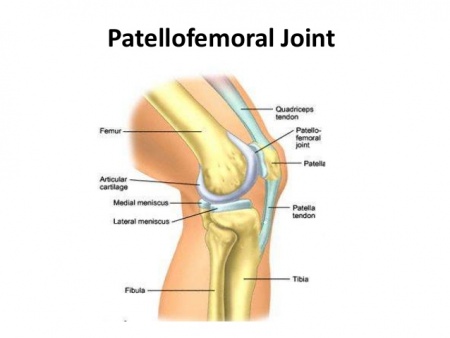
The patellofemoral joint is a unique and complex structure consisting of static elements (bones and ligaments) and dynamic elements (neuromuscular system).[1] The patella has a configuration of a triangle with its apex directed inferiorly. Superiorly, it articulates with the trochlea, the distal articulating surface of the femur, which are the main articulating surfaces of the patellofemoral joint.[2]
Anatomy[edit | edit source]
Articulating Surfaces[edit | edit source]
Patella
The patella is a triangular shaped seasmoid bone, the posterior surface of the patella is covered with articular cartilage.[3]
The articular cartilage of the patella is similar to that of other joints in that it contains a solid phase and a fluid phase that is mostly composed of collagen and glycosaminoglycans. The solid phase is somewhat permeable and when the articular surface is under load, the fluid gradually redistributes itself within the solid matrix. Therefore, the pressure within the fluid is strongly associated with the cushioning effect of the articular cartilage and the low friction coefficient of articular surfaces. Any damage to the articular surfaces causes a loss of pressure within the fluid phase, which subsequently results in higher stresses on the collagen fibers and more vulnerability leading to possible breakdown.[1]
Intercondylar groove
The patella articulates with the intercondylar groove (trochlear groove). The intercondylar groove lateral facet is more prominent anteriorly and steeper than the medial facet to help stabilize the patella against excessive lateral pull.
Ligaments[edit | edit source]
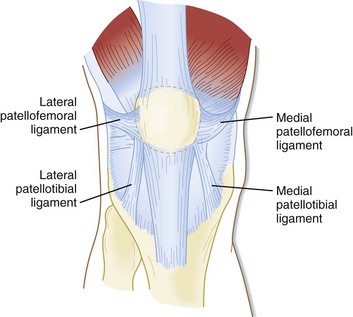
The patellar retinaculum is an important stabilizer of the patellofemoral joint, mainly its medial and lateral components.[4]
The Medial Patellofemoral Ligament (MPFL) - originates on the medial femur and has a “sail-shaped” attachment on the patella and quadriceps tendon. Because of its wider attachment than its origin, several authors have promoted the technique of using a double-bundled graft to recreate the anatomy of this complex. Kang and colleagues described two components of MPFL fibers, using the term superior-oblique bundle and inferior-straight bundle. The clinical significance of this is not yet known, but the authors suggested the bundles may vary in their roles as dynamic versus static stabilizers. Furthermore, length differences between the two bundles or attachment sites, have been described. Mochizuki and colleagues showed the length of the MPFL fibers from the origin to the medial patella was 56.3+/-5.1 mm vs. 70.7+/-4.5 mm to the quadriceps tendon.[5]
The Lateral Patellofemoral Ligament (LPFL) - is an important lateral stabilizer of the patella against medial subluxation or dislocation. Some authors describe the lateral patellofemoral ligament as a palpable thickening of the joint capsule between the patella and femoral epicondyle.[6]
Muscles[edit | edit source]
The quadriceps muscle is the largest and strongest extensor muscle, consisting of rectus femoris and vastus group (vastus lateralis, vastus intermedius and vastus medialis).
The vastus group produces 80% of the knee extension torque and the rectus femoris produces 20% of the knee extension torque.
The vastus medialis has 2 distinct fibre directions. The vastus medialis longus (VML) attaches at 15 to 18 degrees medial to quadriceps tendon and vastus medialis oblique (VMO) attaching at 50 to 55 degrees. The VMO more oblique pull on the patella stabilizes the patella against excessive lateral pull.
Lateral tracking is guided by both the vastus lateralis and the iliotibial band. Patellar motion is further constrained by the patellofemoral ligament, the patellotibial ligament, and the retinaculum.[2]
Joint Mechanics[edit | edit source]
Kinematics[edit | edit source]
At full knee extension, the quadriceps muscle is relaxed and the patella is resting on the suprapatellar fat pad. The patella migrates inferiorly as the knee flexes.
At 20-30 degrees of knee flexion the patella moves inferiorly, lying in the shallow part of the intercondylar groove, explaining why lateral patella dislocations occur near this range. The patella contacts the femur with its inferior pole.
At 60-90 degrees knee flexion the patella occupies the intercondylar groove. There is maximum contact between the patella and the intercondylar groove (1/3 of the posterior surface area of the patella).
At 135 degrees of knee flexion (near full knee flexion), the patella contacts the femur with its superior pole and rests below the intercondylar groove.[3]
Kinetics[edit | edit source]
The patellofemoral joint is exposed to high compression forces.[3]
Compression at the patellofemoral joint:[2]
| Activity | Force | %Body Weight | Pounds of Force |
|---|---|---|---|
| Walking | 850 N | 1/2 x BW | 100 Ibs |
| Bike | 850 N | 1/2 x BW | 100 Ibs |
| Stair Ascend | 1500 N | 3.3 x BW | 660 Ibs |
| Stair Descend | 4000 N | 5 x BW | 1000 Ibs |
| Jogging | 5000 N | 7 x BW | 1400 Ibs |
| Squatting | 5000 N | 7 x BW | 1400 Ibs |
| Deep Squatting | 15000 | 20 x BW | 4000 Ibs |
The compression forces of the patellofemoral joint is influenced by the quadriceps muscle force and the knee flexion angle.
The patella acts like a pulley with the quadriceps tendon attaching to it proximally and the patellar tendon attaching to it distally transmitting the forces of the knee extensor mechanism. The resultant of the Quadriceps tendon and patellar tendon forces is directed to the intercondylar groove.
The compression force in the patellofemoral joint increases with increasing knee flexion. This can be explained through the squat exercise, as the person squats deeper the force demand on the quadriceps muscle increases and the angle between quadriceps tendon and patellar tendon increases, increasing the compression force.
At 60-90 degrees of knee flexion there is maximum patellofemoral joint compression forces and also maximum contact area between the patella and the femur, protecting the joint against the high compression forces.[3]
Pathology/Injury[edit | edit source]
Techniques[edit | edit source]
Examination[edit | edit source]
Examination of the patellofemoral joint involves:[1]
- observation of the position of the patella with the knee in 90° of flexion: patella alta, patella baja, or patellar lateralization may be present.
- observation of patellar tracking in terminal extension (30-0°): a J-curve may be present.
- assess the patellar glide: a tight lateral retinaculum can decrease the medial glide; a medial glide of less than 5 mm (1 quadrant) can indicate a tight retinaculum. If a positive apprehension sign (fear of the patella popping out of position) is elicited with assessment of the patellar glide, suspect a patella subluxation or dislocation.
- palpate the pain: tenderness is often found on the patellar facets, the trochlea, and the peripatellar soft tissue. Tenderness to palpation at the superior or inferior poles of the patella usually indicates another pathology.
- assess the patella compression test. Compress and push the affected patella distally. Pain is a positive test associated with anterior knee pain. An active test, in which the patient contracts the quadriceps tendon against a compressed patella, has a high false-positive rate.
- assess the Q-angle. The Q-angle is the angle formed by a line created from the ASIS to the mid patella intersecting with a line created from the mid patella to the tibial tubercle with the knee in full extension. The average Q-angle for males is 14°, and the average for females is 17°. An increase in this angle can indicate abnormal patellar tracking.
| [8] | [9] | [10] |
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Kim Y-M, Joo Y-B. Patellofemoral Osteoarthritis. Knee Surgery Related Research. 2012;24(4):193-200. doi:10.5792/ksrr.2012.24.4.193.
- ↑ 2.0 2.1 2.2 Medscape. Drugs and Diseases. Patellofemoral Joint Syndromes. Available at: http://emedicine.medscape.com/article/90286-overview#showall (accessed 08 august 2016).
- ↑ 3.0 3.1 3.2 3.3 Neumann DA. Kinesiology of the musculoskeletal system; Foundation for rehabilitation. Mosby & Elsevier. 2010.
- ↑ NAVARRO, Marcelo Schmidt et al. Relationship between the lateral patellofemoral ligament and the width of the lateral patellar facet. Acta ortop. bras. [online]. 2010, vol.18, n.1, pp.19-22. ISSN 1413-7852.
- ↑ Healio MedBlog. Orthopedics. Business of Orthopedics. BLOG: Update on medial patelofemoral anatomy, implications for reconstruction. Available at: http://www.healio.com/orthopedics/business-of-orthopedics/news/blogs/%7B556829f5-0f97-42a6-9c3f-4f6ffe7aa48e%7D/patellofemoral-update/blog-update-on-medial-patellofemoral-anatomy-implications-for-reconstruction (accesed 10 august 2016).
- ↑ Borbas P, Koch P, Fucentese S. Lateral Patellofemoral Ligament Reconstruction Using a Free Gracilis Autograft. ORTHOPEDICS. 2014; 37: e665-e668. doi: 10.3928/01477447-20140626-66
- ↑ Roy Wung. Patellofemoral joint motion and patellar tracking. Available from: https://www.youtube.com/watch?v=Q-80Qi5cx9o (accessed 27 august 2016).
- ↑ Jason Craig. Examination of the Patellofemoral Joint - Palpation. Available from: https://www.youtube.com/watch?v=LgBNuWQMSC8 (accessed 27 august 2016).
- ↑ Jason Craig. Patellofemoral Joint Examination - Observations. Available from: https://www.youtube.com/watch?v=we9COmZ-cig (accessed 27 august 2016).
- ↑ Jason Craig. Patellofemoral Joint Examination - Observations in Sitting. Available from: https://www.youtube.com/watch?v=gmt5hiYlyDQ (accessed 27 august 2016).